Gingival recession: part 2. Surgical management using pedicle grafts
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
KEY POINTS * Gingival recession can be corrected using pedicle grafts but careful case selection is essential for complete root coverage. * To ensure success of periodontal plastic surgery
several patient and tooth related factors need to be assessed before surgery. * Pedicle grafts are not suitable in cases with thin gingival biotype and in areas where there is a lack of
keratinised tissue. ABSTRACT This paper is the second in a three part series looking at the aetiology and management of gingival recession. Part one discussed the aetiology and non-surgical
management and this part aims to discuss the use of pedicle soft tissue grafts in the treatment of gingival recession. This article also considers the factors affecting the outcome of
surgical procedures used to treat localised recession defects. The third paper in this series will consider the use of free soft tissue grafts and guided tissue regeneration. You have full
access to this article via your institution. Download PDF SIMILAR CONTENT BEING VIEWED BY OTHERS CLINICAL EFFECTIVENESS OF PERIOSTEAL PEDICLE GRAFT FOR THE MANAGEMENT OF GINGIVAL RECESSION
DEFECTS—A SYSTEMATIC REVIEW AND META-ANALYSIS Article 07 June 2023 DO IMMEDIATELY PLACED IMPLANTS HAVE BETTER OUTCOMES WHEN PLACED WITH A MINIMAL SPLIT-THICKNESS ENVELOPE FLAP? Article 17
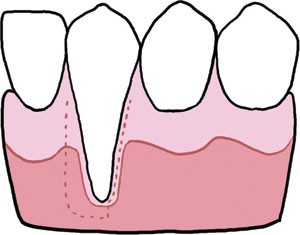
December 2021 ACHIEVING THE OPTIMAL EMERGENCE PROFILE: THE ROLE OF SOFT TISSUE GRAFTING AND PONTIC SITE DEVELOPMENT Article Open access 13 December 2024 INTRODUCTION Gingival recession is
defined as the apical displacement of the gingival margin from the Cemento-Enamel Junction (CEJ).1 The patient's main complaint often relates to poor aesthetics and occasionally it is
related to sensitivity. Part 1 in this series discussed the aetiology of gingival recession and the non-surgical management. This paper aims to introduce some of the surgical options
available to correct localised recession defects. PERIODONTAL PLASTIC SURGERY Periodontal plastic surgery describes any surgical procedures involving the mucogingival tissues. It includes
surgery which attempts to increase the width of keratinised tissue around a tooth and cover any exposed root surface associated with a recession defect. The main indications for surgical
intervention to correct recession defects include the need to improve localised soft tissue aesthetics, reduce hypersensitivity, improve plaque control and prevent further progression of
recession defect.2 CLASSIFICATION OF GINGIVAL RECESSION Miller3 has classified gingival recession into four categories (Table 1). These categories can be used to assess the recession defect
present and predict the possible outcome of any periodontal plastic surgery procedure which would aim to cover the recession defect and restore aesthetics. Defects classified as
Miller's Class I and II can result in full coverage of the recession defect whereas class III would only provide partial coverage to the level of the interdental bone. Class IV defects
are unlikely to provide any root coverage as a result of surgical intervention and therefore any periodontal plastic surgery should be avoided. This is commonly seen in patients who have
developed recession due to chronic periodontal disease. FACTORS AFFECTING OUTCOME OF PERIODONTAL PLASTIC SURGERY There are several factors that can affect the outcome of any periodontal
plastic surgery procedures. These are listed below and should be assessed and corrected where possible before surgery as part of the pre-surgical preparation or during surgery in order to
improve the overall success of the procedure: A) CONDITION OF ROOT SURFACE - PRESENCE OF CALCULUS, CARIES, CONTAMINATED CEMENTUM OR RESTORATIONS ON ROOT SURFACE Any filling material or
caries on the root surface should be removed before surgery and the root surface should be prepared by scaling to remove any residual calculus and contaminated cementum. Removal of all
endotoxins, bacteria and other antigens found in contaminated cementum is essential to leave the root surface biologically compatible with healthy periodontal tissues. Lindhe and Nyman4 and
Lindhe _et al_.5 have highlighted that thorough debridement of the root surface is essential for a successful outcome of periodontal plastic surgery attempting to provide root coverage over
a recession defect. Some authors have suggested the use of citric acid to treat the root surface before the surgical procedure. The aim of this treatment is to remove the smear layer on the
root surface to allow connective tissue attachment to the root surface.6,7 Others have suggested the use of tetracycline hydrochloride to help promote the healing response post surgery
however, clinical studies have failed to show any improvements in outcome when using such agents.8 B) PROMINENT FRENAL ATTACHMENTS Prominent frenal attachment can contribute to the cause of
gingival recession. Before or as part of any periodontal plastic surgery it is worth considering carrying out a frenectomy to relieve any tension on the gingival tissues from a prominent
frenum which may otherwise result in failure of the surgical procedure. C) DEPTH OF VESTIBULE Patients with shallow vestibule depth should not be considered for pedicle grafts as this can
result in further decrease in vestibule depth. Alternative surgical procedures should be considered for these patients. D) TISSUE TYPE Patients with thin gingival biotype are likely to have
a poorer outcome than those with thick gingival biotype. When considering periodontal plastic surgery it is important to assess the periodontal tissues carefully to see if the gingival
tissues require a surgical procedure such as a connective tissue graft that will thicken the tissue while also correcting the recession defect. The amount of keratinised tissue available
adjacent to the recession defect should also be assessed when considering rotational or coronally advanced pedicle graft.8 E) SIZE OF THE RECESSION DEFECT AND GRAFT MATERIAL The graft
material harvested from the donor site should be large enough to cover the whole recession defect and extend beyond it in order to get adequate blood supply from the soft tissue surrounding
the recession defect. As the root surface does not contribute any blood supply to the graft material, recession defects which are narrow result in a better outcome than wide recession
defects as the overlap between graft material and recipient soft tissue bed will be greater. The graft should also be of an adequate thickness to prevent necrosis.2 The height of the
recession defect is not as critical as the width of the defect but will influence the choice of surgical procedure depending on the amount of attached gingival tissue available and the depth
of the vestibule.8 F) THICKNESS OF SPLIT THICKNESS FLAPS RAISED The split thickness pedicle flaps raised for many of the periodontal plastic surgery procedures play an important role in
nourishing the grafted tissue. It is essential that this tissue has a certain amount of thickness to be robust enough to fulfil this role. Evidence has shown that flaps with a thickness of
less than 1 mm can negatively affect the outcome in terms of the amount of root coverage achived.9 CONTRAINDICATIONS TO PERIODONTAL PLASTIC SURGERY A) SMOKING Any surgical procedure carried
out on smokers is likely to have a compromised healing response. Research has shown that smoking can significantly impair the outcome of surgical periodontal therapy when compared to
non-smokers.10,11,12,13 Periodontal plastic surgery should therefore be avoided in patients who smoke. B) POOR ORAL HYGIENE Patients with inadequate oral hygiene and active periodontal
disease should not be considered for periodontal plastic surgery. SURGICAL TECHNIQUES FOR CORRECTING RECESSION DEFECTS Periodontal plastic surgery is technique sensitive and involves
delicate handling of the mucogingival tissues. Burkhardt and Lang14 concluded that the use of magnification and microsurgical instruments to handle the tissues resulted in improved
vascularisation of connective tissue grafts and increased root coverage compared to macrosurgical techniques. There are three main types of periodontal plastic surgery procedures described
in the literature to treat recession defects. These include pedicle flaps, free grafts, and guided tissue regeneration.15 The rest of this article will look at the use of pedicle flaps and a
subsequent article in the series will discuss the use of free grafts and guided tissue regeneration. PEDICLE FLAPS A pedicle graft involves repositioning donor tissue from an area adjacent
to the recession defect to cover the exposed root surface. It avoids the need of a second surgical site and has the advantage of retaining its own blood supply from the base of the flap
which remains attached to the donor site. This helps nourish the graft and facilitates vascular union with the recipient site. The pedicle flap was first described by Grupe and Warren16 as a
laterally repositioned full thickness flap. Here the donor tissue is taken from one side of the recession defect and repositioned over the exposed root surface. This was later modified by
Hattler17 with the use of a split thickness flap repositioned in a similar way to cover multiple exposed root surfaces. Soon after, Cohen and Ross18 described the double-papilla repositioned
flap for use in areas where there was insufficient keratinised gingival tissue on any one side of the recession defect to reposition and cover the exposed root surface. Here the papillae
are taken from both sides of the recession defect and repositioned over the exposed root surface. This procedure limits itself to single tooth recession defects. The double-papilla flap can
also be performed either as a full thickness flap or a split thickness flap depending on the thickness of the gingival tissues.19 LATERALLY REPOSITIONED PEDICLE FLAP CLINICAL TECHNIQUE (FIGS
1A-G) Before raising the donor tissue, the width of the recession defect should be measured to gauge what size pedicle flap is required. To allow adequate union and healing of the
repositioned flap a cuff of epithelialised tissue around the margins of the recession defect is cut away to expose the underlying connective tissue. Similarly, the surface epithelium
adjacent to the recession defect on the side opposite to where the donor tissue will be taken is also removed to expose the underlying connective tissue (Fig. 1a-b). A pedicle flap twice the
width of the recession defect is then raised by making an oblique incision away from the recession defect leaving a few millimetres of keratinised gingival tissue around the adjacent tooth
at the donor site. A second oblique distal relieving incision is made towards the apical region from where the first incision terminated and extended beyond the mucogingival junction into
the alveolar lining mucosa. A split thickness pedicle flap is then raised and rotated over the exposed root surface and the connective tissue previously exposed on the opposite side (Fig.
1c). The graft tissue should be free from any tension; if not the relieving incision should be extended further apical. Once repositioned the pedicle flap is sutured down with fine
interrupted sutures (Fig. 1d) and pressure applied for a few minutes to minimise the clot underneath the pedicle flap. This is important to ensure good union between donor and recipient
tissues and to ensure good vascularisation of the grafted tissue. A periodontal dressing can be placed if necessary but is not mandatory. The donor site is left to heal by secondary
intention. If the flap is left under tension, or there is excessive movement and poor stabilisation or if the flap is too narrow for the recession defect, then there is a higher chance of
failure of the procedure. Figures 1e-g show an example of a Miller's Class III recession defect on the lower left first molar treated with a laterally repositioned pedicle flap. At one
week post-surgery there has been significant coverage of the exposed mesial root surface. Grafting of a Miller's Class III defect of this size is highly unlikely to provide full
coverage of the recession defect; however, significant improvement can be made with partial coverage of the root surface and an increased amount of keratinised tissue around the gingival
margin as shown in this case. A second surgical procedure with a coronally repositioned flap (discussed later) can be undertaken to try and cover the remaining exposed root surface if
necessary. DOUBLE PAPILLA ROTATIONAL FLAP CLINICAL TECHNIQUE (FIGS 2A-B) The width of the recession defect should be measured initially to ensure there is sufficient width of tissue
available from the two adjacent papillae to allow full coverage of the exposed root surface. A cuff of epithelialised tissue is removed from around the recession defect to expose the
underlying connective tissue (Fig. 2a). Split thickness flaps of the papillae either side of the recession defect with vertical reliving incisions on the distal line angle of the tooth in
front and mesial line angle of the tooth behind should be raised. The relieving incisions are extended beyond the mucogingival line and taken down to bone at this point to help release
tension in the flap. The two papillae are repositioned and placed over the exposed root surface and sutured together with fine interrupted sutures along the midline of the exposed root
surface (Fig. 2b). A sling suture is placed around the tooth to hold the grafted tissue in its position and prevent it from sliding apically. Gentle pressure is applied for a few minutes to
minimise the clot that forms under the pedicle graft and a periodontal dressing can be placed if necessary. The exposed connective tissue at the donor site can be left to heal by secondary
intention. Inadequate suturing and inadequate stabalisation can result in separation of the two pedicle flaps resulting in failure of the procedure. CORONALLY REPOSITIONED FLAP CLINICAL
TECHNIQUE (FIGS 3A-F) The coronally advanced flap was first described by Bernimoulin _et al_.20 The procedure can be performed either as a one stage technique to cover shallow recession
defects21 or a two stage technique which is combined with a free gingival graft, connective tissue graft or with guided tissue regeneration procedures. If the gingival tissue apical to the
recession defect has thin gingival biotype or there is insufficient keratinised tissue, a free gingival graft or a connective tissue graft can be carried out first to increase the thickness
and amount of keratinised tissue. After approximately three months of healing the tissue can be coronally repositioned as a second stage surgery. If the gingival biotype is thick and there
is adequate keratinised tissue (minimum 3 mm) then the tissue can be coronally repositioned as a one-stage technique. In order to carry out this procedure it is essential to ensure there are
shallow crevicular depths on interproximal surfaces and no interproximal bone loss.1 The amount of coronal advancement required is determined by measuring the height of the recession
defect. The same length is then measured from the tip of the papilla towards the apex and horizontal incisions are placed through the tissue for a split thickness flap. Vertical relieving
incisions are placed at the distal line angle of one tooth anteriorly and mesial line angle of one tooth posterior to the tooth with the recession defect (Fig. 3a). A split thickness flap of
even thickness is raised and extended beyond the mucogingival margin. The periosteum is released to allow freedom of movement of the flap. The most coronal part of the papilla which remains
intact is de-epithelialised before coronal advancement of the flap (Fig. 3b). The flap is then sutured in place approximately 0.5 mm to 1 mm coronal to the CEJ22 with interrupted sutures in
the papilla regions and along the reliving incisions (Fig. 3c). Gentle pressure is applied for a few minutes and if necessary a periodontal dressing can be placed. Excessive tension in the
coronally advanced flap can result in failure or a reduced amount of root coverage. Figures 3d-f show an example of a recession defect at UL2 treated initially with a connective tissue graft
(see article 3) to increase the thickness of the gingival tissues around the recession defect followed by a second surgical procedure with a coronally repositioned pedicle flap to cover the
recession defect. The tooth has also had some minor enameloplasty to decrease the length and some composite bonding to improve the overall shape of the tooth. PROGNOSIS Periodontal plastic
surgery has been shown to be effective in reducing gingival recession defects with a concomitant improvement in attachment levels.23 Achieving full root coverage following a single
periodontal plastic surgical procedure is difficult and success is often considered to be any decrease in amount of exposed root surface (Fig. 1g) ie an increase in gingival height from the
mucogingival line to the gingival margin.24 The size of the initial recession defect will also influence the final outcome. A recent systematic review found that overall a better percentage
of complete and mean root coverage was seen in recession defects less that 4 mm.9 The mean root coverage achieved with a laterally repositioned flap and the double papilla flap have shown to
vary between 34-81% and complete root coverage varies between 40-50% of sites.25,26 With these procedures there is a risk of donor site recession particularly with the laterally
repositioned flap of approximately 1 mm.27 The mean root coverage achieved with a single stage coronally repositioned flap varies between 55-99% and complete root coverage ranges from 24-95%
of sites.25,26 Pini-Patro _et al_.28 concluded that in order to achieve 100% root coverage with a coronally repositioned flap, the flap should be over compensated by 2-2.5 mm and sutured
tension free. However, this may be difficult in cases where there is a large recession defect and a shallow sulcus depth. The coronally advanced flap is often used together with a
subepithelial connective tissue graft and has proven to be the gold standard treatment in the treatment of recession defects.29 In Miller's Class I defects this combination has shown to
provide complete root coverage of the recession defect.30 The use of connective tissue grafts is discussed further in the third article in this series. CONCLUSIONS Pedicle flaps can be
useful in correcting small Miller's Class I and II recession defects. The graft has the advantage of retaining its own blood supply which can aid healing; however, this graft should be
restricted to cases where the gingival biotype is thick and there is sufficient amount of keratinised tissue adjacent to the recession defect. In cases with thin gingival biotype or limited
keratinised tissue it may be more sensible to consider a free graft, possibly in combination with a pedicle graft. REFERENCES * Kassab M M, Cohen R E . Treatment of gingival recession. _J Am
Dent Assoc_ 2002; 133: 1499–1506. Article Google Scholar * Saha S, Bateman G J . Mucogingival grafting procedures – an update. _Dent Update_ 2008; 35: 561–562, 565–568. Article Google
Scholar * Miller P D, Jr. A classification of marginal tissue recession. _Int J Periodontics Restorative Dent_ 1985; 5: 8–13. PubMed Google Scholar * Lindhe J, Nyman S . Long-term
maintenance of patients treated for advanced periodontal disease. _J Clin Periodontol_ 1984; 11: 504–514. Article Google Scholar * Lindhe J, Westfelt E, Nyman S, Socransky S S, Haffajee A
D . Long-term effect of surgical/non-surgical treatment of periodontal disease. _J Clin Periodontol_ 1984; 11: 448–458. Article Google Scholar * Miller P D, Jr. Root coverage using the
free soft tissue autograft following citric acid application. III. A successful and predictable procedure in areas of deep-wide recession. _Int J Periodontics Restorative Dent_ 1985; 5:
14–37. PubMed Google Scholar * Polson A M, Frederick G T, Ladenheim S, Hanes P J . The production of a root surface smear layer by instrumentation and its removal by citric acid. _J
Periodontol_ 1984; 55: 443–446. Article Google Scholar * Baker P. The management of gingival recession. _Dent Update_ 2002; 29: 114–120, 122–124, 126. Article Google Scholar * Chambrone
L, Sukekava F, Araújo M G, Pustiglioni F E, Chambrone L A, Lima L A . Root-coverage procedures for the treatment of localized recession-type defects: a Cochrane systematic review. _J
Periodontol_ 2010; 81: 452–478. Article Google Scholar * Preber H, Bergstrom J . Effect of cigarette smoking on periodontal healing following surgical therapy. _J Clin Periodontol_ 1990;
17: 324–328. Article Google Scholar * Trombelli L, Scabbia A . Healing response of gingival recession defects following guided tissue regeneration procedures in smokers and non-smokers. _J
Clin Periodontol_ 1997; 24: 529–533. Article Google Scholar * Martins A G, Andia D C, Sallum A W, Sallum E A, Casati M Z, Nociti Júnior F H . Smoking may affect root coverage outcome: a
prospective clinical study in humans. _J Periodontol_ 2004; 75: 586–591 Article Google Scholar * Chambrone L, Chambrone D, Pustiglioni F E, Chambrone L A, Lima L A . The influence of
tobacco smoking on the outcomes achieved by root-coverage procedures: a systematic review. _J Am Dent Assoc_ 2009; 140: 294–306. Article Google Scholar * Burkhardt R, Lang N P . Coverage
of localized gingival recessions: comparison of micro- and macrosurgical techniques. _J Clin Periodontol_ 2005; 32: 287–293. Article Google Scholar * Chambrone L, Sukekava F, Araújo M G,
Pustiglioni F E, Chambrone L A, Lima L A . Root coverage procedures for the treatment of localised recession-type defects. _Cochrane Database Syst Rev_ 2009; (2): CD007161. Google Scholar *
Grupe H E, Warren R F . Repair of gingival defects by a sliding flap operation. _J Periodontol_ 1956; 27: 92–95. Article Google Scholar * Hattler A B. Mucogingival surgery - utilization
of interdental gingiva as attached gingiva by surgical displacement. _Periodontics_ 1967; 5: 126–131. PubMed Google Scholar * Cohen D W, Ross S E . The double papillae repositioned flap in
periodontal therapy. _J Periodontol_ 1968; 39: 65–70. Article Google Scholar * Pfeifer J S, Heller R . Histologic evaluation of full and partial thickness lateral repositioned flaps: a
pilot study. _J Periodontol_ 1971; 42: 331–333. Article Google Scholar * Bernimoulin J P, Luscher B, Muhlemann H R . Coronally repositioned periodontal flap. Clinical evaluation after one
year. _J Clin Periodontol_ 1975; 2: 1–13. Article Google Scholar * Allen E P, Miller P D, Jr. Coronal positioning of existing gingiva: short term results in the treatment of shallow
marginal tissue recession. _J Periodontol_ 1989; 60: 316–319. Article Google Scholar * Maynard J G, Jr. Coronal positioning of a previously placed autogenous gingival graft. _J
Periodontol_ 1977; 48: 151–155. Article Google Scholar * Roccuzzo M, Bunino M, Needleman I, Sanz M . Periodontal plastic surgery for treatment of localized gingival recessions: a
systematic review. _J Clin Periodontol_ 2002; 29(Suppl 3): 178–194. Article Google Scholar * Wennström J L, Zucchelli G . Increased gingival dimensions. A significant factor for successful
outcome of root coverage procedures? A 2-year prospective clinical study. _J Clin Periodontol_ 1996; 23: 770–777. Article Google Scholar * Wennström J L. Mucogingival therapy. _Ann
Periodontol_ 1996; 1: 671–701. Article Google Scholar * Pagliaro U, Nieri M, Franceschi D, Clauser C, Pini-Prato G. Evidence based mucogingival therapy. Part 1: A critical review of the
literature on root coverage procedures. _J Periodontol_ 2003; 74: 709–740. Article Google Scholar * Caffesse R G, Guinard E A . Treatment of localized gingival recessions. Part IV. Results
after three years. _J Periodontol_ 1980; 51: 167–170. Article Google Scholar * Pini Prato G P, Baldi C, Nieri M et al. Coronally advanced flap: the postsurgical position of the gingival
margin is an important factor for achieving complete root coverage. _J Periodontol_ 2005; 76: 713–722. Article Google Scholar * Chambrone L, Faggion C M, Jr Pannuti C M, Chambrone L A .
Evidence based periodontal plastic surgery: an assessment of quality of systematic reviews in the treatment of recession-type defects. _J Clin Periodontol_ 2010; 37: 1110–1118. Article
Google Scholar * Cairo F, Pagliaro U, Nieri M . Treatment of gingival recession with coronally advanced flap procedures: a systematic review. _J Clin Periodontol_ 2008; 35(8 Suppl):
136–162. Article Google Scholar Download references ACKNOWLEDGEMENTS The authors would like to thank Dr Paul Baker, Specialist Periodontist for contributing the clinical pictures shown in
Figures 1e-g. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Restorative Dentistry, Specialist Registrar in Restorative Dentistry, Leeds Dental Institute, Clarendon Way, Leeds,
LS2 9LU, M. Patel * Department of Restorative Dentistry, Consultants in Restorative Dentistry, Leeds Dental Institute, Clarendon Way, Leeds, LS2 9LU, M. F. W.-Y. Chan Authors * M. Patel View
author publications You can also search for this author inPubMed Google Scholar * P. J. Nixon View author publications You can also search for this author inPubMed Google Scholar * M. F.
W.-Y. Chan View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to M. Patel. RIGHTS AND PERMISSIONS Reprints and
permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Patel, M., Nixon, P. & Chan, MY. Gingival recession: part 2. Surgical management using pedicle grafts. _Br Dent J_ 211, 315–319 (2011).
https://doi.org/10.1038/sj.bdj.2011.821 Download citation * Accepted: 21 July 2011 * Published: 07 October 2011 * Issue Date: 08 October 2011 * DOI: https://doi.org/10.1038/sj.bdj.2011.821
SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to
clipboard Provided by the Springer Nature SharedIt content-sharing initiative