The international spinal cord injury pain basic data set (version 2. 0)
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT OBJECTIVES: To revise the International Spinal Cord Injury Pain Basic Data Set (ISCIPBDS) based on new developments in the field and on suggestions from the spinal cord injury (SCI)
and pain clinical and research community. SETTING: International. METHODS: The ISCIPBDS working group evaluated suggestions regarding the utility of the ISCIPBDS and made modifications in
response to these and to significant developments in the field. The revised ISCIPBDS (version 2.0) was reviewed by members of the Executive Committee of the International SCI Standards and
Data Sets, the International Spinal Cord Society (ISCoS) Executive and Scientific Committees, the American Spinal Injury Association and American Pain Society Boards and the Neuropathic Pain
Special Interest Group of the International Association for the Study of Pain, individual reviewers and societies and the ISCoS Council. RESULTS: The ISCIPBDS (version 2.0) is significantly
shortened but still contains clinically relevant core questions concerning SCI-related pain. The revisions include an updated SCI pain classification, omission of three questions regarding
temporal pain pattern and three pain interference questions. The remaining three pain interference questions concern perceived interference with activities, mood and sleep for overall pain
rather than for individual pain problems and are scored on a 0 to 10 scale. SIMILAR CONTENT BEING VIEWED BY OTHERS THE INTERNATIONAL SPINAL CORD INJURY PAIN BASIC DATA SET (VERSION 3.0)
Article 25 July 2023 INTERNATIONAL SPINAL CORD INJURY CORE DATA SET (VERSION 3.0)—INCLUDING STANDARDIZATION OF REPORTING Article 28 October 2022 CROSS-CULTURAL ADAPTATION AND VALIDATION OF
THE FRENCH VERSION OF THE SPINAL CORD INJURY PAIN INSTRUMENT (SCIPI) Article 24 May 2022 INTRODUCTION After the International Spinal Cord Injury Pain Basic Data Set (ISCIPBDS; version 1.1)
was published in 20081 there have been several suggestions from the clinical spinal cord injury (SCI) field to shorten it in order to increase its clinical utility. In addition, there has
been a significant update of the SCI pain taxonomy.2, 3 For these reasons, the ISCIPBDS working group decided to review and update the current version. Both the original and the revised
ISCIPBDS (version 2.0) are intended to be collected by health-care professionals familiar with SCI, and to be used at the initial evaluation as well as at regular follow-up sessions. Data
should be collected by interview and each question read to the patient or research participant as worded. The overall purpose of the ISCIPBDS (version 2.0) is unchanged and consistent with
the purpose and vision of the International Spinal Cord Injury Data Sets.4 The ISCIPBDS should be used together with the International SCI Core Data Set,5 which includes information on date
of birth and injury, gender, the cause of the SCI and neurological status including positive and negative sensory signs. MATERIALS AND METHODS The development of the original ISCIPBDS and
information regarding the members of the working group was described in detail previously.1 The data collected provide a minimal amount of standardized information necessary for determining
interference of pain with physical and emotional function and sleep, probable pain diagnosis, location, intensity and duration. In order to ensure consistency in data collection and to
facilitate interpretation, detailed information is provided in the updated syllabus (version 2.0) for each variable and response category. The development of the revised version of the
ISCIPBDS (version 2.0) followed the same steps as the original version: * 1 The working group made the revisions as described below via e-mail discussions. A subset of the working group also
had a face-to-face meeting during the American Spinal Injury Association (ASIA) conference in May 2013 in Chicago. The version resulting from this meeting was further developed via e-mail
correspondence. * 2 The ISCIPBDS (version 2.0) was reviewed by members of the Executive Committee of the International SCI Standards and Data Sets. The suggestions from the Committee members
were discussed in the working group and appropriate changes were made. * 3 The ISCIPBDS (version 2.0) was reviewed by members of the International Spinal Cord Society (ISCoS) Executive and
Scientific Committees and ASIA Board with no further suggestions for improvement. * 4 The ISCIPBDS (version 2.0) was reviewed and endorsed by members of the American Pain Society (APS) Board
and the Neuropathic Pain Special Interest Group (NeuPSIG) of the International Association for the Study of Pain (IASP). * 5 Organizations, societies and individuals with an interest in
SCI-related pain were invited to review and comment on the ISCIPBDS (version 2.0). The data set was also posted on the ISCoS and ASIA websites to allow additional comments and suggestions. *
6 To finalize the ISCIPBDS (version 2.0), members of the ISCoS Executive and Scientific Committees and the ASIA Board reviewed the data set for final approval. RESULTS Several changes were
made from version 1.1 to version 2.0. These include: (1) omission of some items; (2) updating the SCI pain classification; and (3) Re-structuring of the ISCIPBDS. These changes (detailed
below) were made because of both recent updates to the pain classification scheme and suggestions from the field to shorten and focus the ISCIPBDS to facilitate its clinical utility.
OMISSION OF ITEMS The ISCIPBDS was shortened to contain only those items that we believe essential for a correct pain classification and for determining intensity and broad impact on
activities, sleep and mood. Items that did not address these critical factors were removed. The variables ‘Number of days with pain in the last 7 days including today’, ‘How long does your
pain usually last?’ and ‘When is the pain most intense?’, were removed as these were not considered critical for determining pain type, intensity and pain impact. Moreover, in a validation
study of the ISCIPBDS, we found little support for the validity of the two pain duration items (days of pain and duration of pain incidents6). The findings from our study influenced our
decision to remove these items. The following three interference items were removed: ‘How much do you limit your activities in order to keep your pain from getting worse?’, ‘How much has
your pain changed your ability to take part in recreational and other social activities?’ and ‘How much has your pain changed the amount of satisfaction or enjoyment you get from
family-related activities?’ In the validation study cited above, the internal consistency (Cronbach’s alpha) suggested some redundancy among the pain interference items and therefore we
concluded that all six items were not required to adequately assess the pain interference domain. In our study,6 we found that the three remaining interference items showed the strongest
associations with the validity criteria. We concluded from these findings that only three items were needed to provide a valid measure of pain interference. Another effort to shorten the
ISCIPBDS included the instruction to apply the pain interference items to overall pain rather than to each of the different pain problems. Moreover, in order to make these items consistent
with the pain intensity ratings, we changed the response levels from 0 to 6 to the more common 0 to 10 numerical rating scale (NRS) metric. UPDATED SCI PAIN CLASSIFICATION Our proposed
changes include updating the pain classification to be consistent with the new SCI pain taxonomy that has been published and validated.2, 3 Related to the variable Type of pain, an extra
option _‘Other’_ was added. In addition, only one choice of pain type can be made on the form. The codes include: Musculoskeletal (nociceptive) Visceral (nociceptive) Other (nociceptive)
At-level SCI (neuropathic) Below-level SCI (neuropathic) Other (neuropathic) Other Unknown These types of pain should be coded using the following criteria: MUSCULOSKELETAL (NOCICEPTIVE)
Musculoskeletal (nociceptive) pain refers to: (1) pain in a region with preserved sensation above, at or below the neurological level of injury (NLI) and (2) pain believed to be originating
in musculoskeletal structures. This pain type is indicated by pain with a dull or aching quality, pain initiated or aggravated by movement, tenderness of musculoskeletal structures on
palpation, relief in response to anti-inflammatory or opioid medications, or evidence of skeletal pathology on imaging consistent with the pain presentation. Examples include: mechanical
pain, spinal fractures, muscular injury, shoulder overuse syndromes and muscle spasm.7, 8, 9, 10 VISCERAL (NOCICEPTIVE) Visceral (nociceptive) pain refers to: (1) pain located in the thorax,
abdomen or pelvis; and (2) pain believed to originate in visceral structures. This pain type is indicated by dull, tender or cramping pain and related to visceral pathology or dysfunction,
such as infection or obstruction, for example, urinary tract infection, ureteric calculus and constipation.2, 7, 8, 9, 10 OTHER (NOCICEPTIVE) Other (nociceptive) pain refers to nociceptive
pains that do not fall into the musculoskeletal or visceral categories directly related or unrelated to SCI, for example, pain associated with ulceration of the skin and headache.9 AT-LEVEL
SCI (NEUROPATHIC) At-level SCI (neuropathic) pain refers to neuropathic pain distributed segmentally due to spinal cord or nerve root damage. At-level neuropathic pain is located
unilaterally or bilaterally anywhere within the dermatome of the NLI and three dermatomes below this level. This pain is often perceived as hot-burning, tingling, pricking, pins and needles,
squeezing, cold, electric or shooting and often associated with allodynia, hypoalgesia or hyperalgesia within the painful area. BELOW-LEVEL SCI (NEUROPATHIC) Below-level SCI (neuropathic)
pain refers to neuropathic pain that is located more than three dermatomes below the NLI and may be perceived up to the NLI. This pain is often perceived as hot-burning, tingling, pricking,
pins and needles, squeezing, cold, electric or shooting and often associated with allodynia, hypoalgesia or hyperalgesia within the painful area. OTHER (NEUROPATHIC) Other (neuropathic) pain
refers to neuropathic pains that are located above, at, or below the NLI but are not directly related to the SCI (for example, post-herpetic neuralgia, painful diabetic neuropathy, central
post-stroke pain, and compressive mononeuropathies).8, 9 OTHER Other pain refers to: (1) pain that is unrelated to the SCI and (2) pain without any identifiable noxious stimulus,
inflammation or damage to the nervous system, for example, Complex Regional Pain Syndrome type I, interstitial cystitis pain, irritable bowel syndrome pain and fibromyalgia. UNKNOWN Unknown
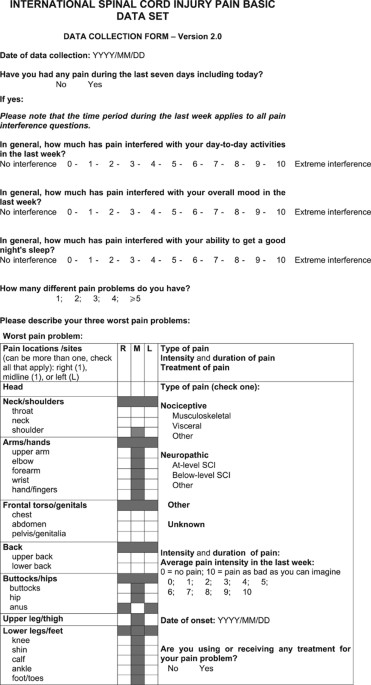
pain refers to pain of unknown etiology. RESTRUCTURING OF THE ISCIPBDS In addition to deletion of some items, we changed the order of the items (see Appendix). Because the three Pain
Interference questions refer to ‘overall pain’, these items will be asked before any questions regarding specific pain types. Moreover, respondents are asked to rate the interference items
on a 0 to 10 scale instead of 0 to 6 scale to be consistent with the pain intensity item. Please note that the psychometric properties were evaluated with these items scored between 0 and
6.6 However, we expect minimal to no effects on these properties with the revision. The remaining variables listed below are unchanged and described as previously.1 Date of data collection
Have you had any pain during the last 7 days including today? How many different pain problems do you have? Description of the three worst pain problems Location of pain Average pain
intensity in the last week Date of onset Are you using or receiving any treatment for your pain problem? The ISCIPBDS (version 2.0) data sheet is included in the Appendix and the data sheet
and the revised syllabus are available on the website of ISCoS (http://www.iscos.org.uk). Revised training cases are likewise available together with the syllabus on the ISCoS website.
DISCUSSION The revised ISCIPBDS (version 2.0) presented in this paper is an effort to provide an abbreviated, updated and standardized way of evaluating and reporting the diverse pains that
occur in persons with SCI. The ISCIPBDS has been significantly shortened, but assesses similar domains as the original version.1 The revised version presented in this paper was designed to
contain a minimum most critical clinically relevant pain information that can be collected in the daily practice of health-care professionals with expertise in SCI. Another criterion is that
the evaluation should be logistically feasible across various settings and countries including the developing countries. The ISCIPBDS (version 2.0) should, as the original version, be used
in combination with the ASIA Impairment Scale11 to determine the extent of neurological injury and to determine the location of pain relative to injury (that is, above, at and below). In
summary, the ISCIPBDS (version 2.0) is intended to be used to evaluate pain in daily clinical practice at both in- and out-patient SCI clinics around the world. In a specialized pain clinic
managing patients with SCI, more sophisticated methods including quantitative sensory assessments would add diagnostic precision. Although one might consider the revised ISCIPBDS to have
less content validity, because the revised version contains fewer items, our view is that it has retained the items that are most critical. Of more importance, perhaps, the Data Set is now
more brief, which will likely increase its clinical utility. It is our intention to continue to update and improve the ISCIPBDS and the working group (through the corresponding author)
welcomes additional suggestions and comments for further improvement. In particular, we welcome feedback from clinical practitioners regarding the utility of the ISCIPBDS in clinical
settings. DATA ARCHIVING There were no data to deposit. REFERENCES * Widerström-Noga E, Biering-Sørensen F, Bryce T, Cardenas DD, Finnerup NB, Jensen MP _et al_. The International Spinal
Cord Injury Pain Basic Data Set. _Spinal Cord_ 2008; 46: 818–823. Article PubMed Google Scholar * Bryce TN, Biering-Sorensen F, Finnerup NB, Cardenas DD, Defrin R, Lundeberg T _et al_.
International spinal cord injury pain (ISCIP) classification: part I. Background and description. _Spinal Cord_ 2012; 50: 413–417. Article CAS PubMed Google Scholar * Bryce TN,
Biering-Sorensen F, Finnerup NB, Cardenas DD, Defrin R, Ivan E _et al_. International spinal cord injury pain (ISCIP) classification: part 2. Initial validation using vignettes. _Spinal
Cord_ 2012; 50: 404–412. Article CAS PubMed Google Scholar * Biering-Sørensen F, Charlifue S, DeVivo M, Noonan V, Post M, Stripling T _et al_. International spinal cord injury data sets.
_Spinal Cord_ 2006; 44: 530–534. Article PubMed Google Scholar * DeVivo M, Biering-Sørensen F, Charlifue S, Noonan V, Post M, Stripling T _et al_. International Spinal Cord Injury Core
Data Set. _Spinal Cord_ 2006; 44: 535–540. Article CAS PubMed Google Scholar * Jensen MP, Widerström-Noga E, Richards JS, Finnerup NB, Biering-Sørensen F, Cardenas DD . Reliability and
validity of the International Spinal Cord Injury Basic Pain Data Set items as self-report measures. _Spinal Cord_ 2010; 48: 230–238. Article CAS PubMed Google Scholar * Donovan WH,
Dimitrijevic MR, Dahm L, Dimitrijevic M . Neurophysiological approaches to chronic pain following spinal cord injury. _Paraplegia_ 1982; 20: 135–146. CAS PubMed Google Scholar * Siddall
PJ, Yezierski RP, Loeser JD . Pain following spinal cord injury: Clinical features, prevalence, and taxonomy. _IASP Newslett_ 2000; 3: 3–7. Google Scholar * Bryce TN, Ragnarsson KT .
Epidemiology and classification of pain after spinal cord injury. _Top Spinal Cord Inj Rehabil_ 2001; 7: 1–17. Article Google Scholar * Cardenas DD, Turner JA, Warms CA, Marshall HM .
Classification of chronic pain associated with spinal cord injuries. _Arch Phys Med Rehabil_ 2002; 83: 1708–1714. Article PubMed Google Scholar * Kirshblum SC, Burns SP, Biering-Sorensen
F, Donovan W, Graves DE, Jha A _et al_. International standards for neurological classification of spinal cord injury (Revised 2011). _J Spinal Cord Med_ 2011; 34: 535–546. Article PubMed
PubMed Central Google Scholar Download references ACKNOWLEDGEMENTS We thank the ISCoS, the ASIA and the APS Boards and the IASP NeuPSIG for endorsement. We also thank Lawrence Vogel and
Marcel Post for helpful suggestions. Pfizer Corp supported the initial work for development of the ISCIPBDS (version 1.1) with an unconditional educational grant. AUTHOR INFORMATION AUTHORS
AND AFFILIATIONS * Miami Project to Cure Paralysis, Lois Pope Life Center, Miller School of Medicine, University of Miami, Miami, FL, USA E Widerström-Noga * Department of Rehabilitation
Medicine, Miller School of Medicine, University of Miami, Miami, FL, USA E Widerström-Noga & D D Cardenas * Clinic for Spinal Cord Injuries, Glostrup University Hospital, and Faculty of
Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark F Biering-Sørensen * Department of Rehabilitation Medicine, Icahn School of Medicine at Mount Sinai, New York, NY,
USA T N Bryce * Danish Pain Research Center, Aarhus University Hospital, Aarhus, Denmark N B Finnerup * Department of Rehabilitation Medicine, University of Washington, Seattle, WA, USA M P
Jensen * Department of Physical Medicine and Rehabilitation, University of Alabama at Birmingham, Birmingham, AL, USA J S Richards * Department of Pain Management, Greenwich Hospital,
Hammond Care, Sydney, New South Wales, Australia P J Siddall * Sydney Medical School—Northern, University of Sydney, Sydney, New South Wales, Australia P J Siddall Authors * E
Widerström-Noga View author publications You can also search for this author inPubMed Google Scholar * F Biering-Sørensen View author publications You can also search for this author
inPubMed Google Scholar * T N Bryce View author publications You can also search for this author inPubMed Google Scholar * D D Cardenas View author publications You can also search for this
author inPubMed Google Scholar * N B Finnerup View author publications You can also search for this author inPubMed Google Scholar * M P Jensen View author publications You can also search
for this author inPubMed Google Scholar * J S Richards View author publications You can also search for this author inPubMed Google Scholar * P J Siddall View author publications You can
also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to E Widerström-Noga. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no conflict of
interest. APPENDIX APPENDIX RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Widerström-Noga, E., Biering-Sørensen, F., Bryce, T. _et al._ The
International Spinal Cord Injury Pain Basic Data Set (version 2.0). _Spinal Cord_ 52, 282–286 (2014). https://doi.org/10.1038/sc.2014.4 Download citation * Received: 12 November 2013 *
Revised: 11 December 2013 * Accepted: 03 January 2014 * Published: 28 January 2014 * Issue Date: April 2014 * DOI: https://doi.org/10.1038/sc.2014.4 SHARE THIS ARTICLE Anyone you share the
following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer
Nature SharedIt content-sharing initiative KEYWORDS * Spinal cord injuries * pain * pain measurement * psychometrics * pain classification * pain interference