The impact of lymphadenectomy on cancerspecific survival in patients with low-grade endometrioid carcinoma of stage T1a
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
For patients with low-grade endometrioid carcinoma of stage T1a, the role of lymphadenectomy in staging surgery remains controversial. This study aims to evaluate the impact of
lymphadenectomy on cancer-specific survival (CSS) in this patient population using a large, population-based dataset. We conducted a retrospective analysis using the Surveillance,
Epidemiology, and End Results (SEER) database, identifying 11,014 patients with stage T1a, low-grade endometrioid carcinoma from 2004 to 2015. Patients were divided into lymphadenectomy and
non-lymphadenectomy groups. Propensity score matching (PSM) was performed to balance baseline characteristics. Kaplan-Meier analysis, log-rank tests, and multivariate Cox regression were
used to assess CSS and identify independent prognostic factors. Before PSM, the non-lymphadenectomy group had higher CSS compared to the lymphadenectomy group (HR = 1.56, 95% CI: 1.16–2.10,
p = .003). After 1:1 PSM, CSS was similar between the two groups (HR = 1.09, 95% CI: 0.78–1.53, p = .605). Subgroup analyses showed no significant differences in CSS except for the subgroup
with tumor size > 2 cm, where non-lymphadenectomy was associated with better CSS (HR = 0.50, p = .035). Multivariate Cox regression analysis identified age, marital status, histological
grade, and chemotherapy as independent prognostic factors for CSS, while lymphadenectomy was not (p = .980).. Our findings suggest that lymphadenectomy does not improve CSS in patients with
low-grade endometrioid carcinoma of stage T1a.
Globally, uterine cancer ranks as the sixth most prevalent form of cancer among women and the 14th most common cancer in general. In 2018, there were more than 380,000 new diagnoses of this
disease1. The increasing prevalence of endometrial cancer is largely due to the rise in obesity rates and the aging population2. Consequently, mortality rates have been increasing by an
average of 1.9% per year, primarily because of the growing obesity problem, which is the most significant known risk factor for endometrial cancer3,4. 80% of endometrial cancers are
localized within the uterus at the time of diagnosis, often manifesting as postmenopausal bleeding5. This typical symptom facilitated early detection, which leaded to earlier treatment and
better tumor outcomes6.
For individuals with endometrial cancer, the standard surgical treatment involves a complete extrafascial hysterectomy along with the removal of both fallopian tubes and ovaries, as well as
an assessment of the pelvic and para-aortic lymph nodes7. Regarding the need for systematic lymphadenectomy, Mayo criteria (Pathological type of endometrioid carcinoma; Myographic
infiltration does not exceed 50%; Histological grade was G1 or G2; Tumor size ≤ 2 cm) have been widely used in clinical practice to judge whether patients are at low risk of lymph node
metastasis. Patients who do not meet the above criteria may be high risk of lymph node metastasis and should be considered for systemic lymphadenectomy8,9. However, these data are difficult
to accurately evaluate before the final pathological diagnosis is made, and some centers use intraoperative freezing pathology to assist decision-making, and avoid systematic lymphadenectomy
if the return results meet the above criteria10.
It is still controversial to avoid systematic lymphadenectomy in staging surgery for patients with early-staged endometrial cancer11. Therefore, based on a large amount of data from the
Surveillance, Epidemiology, and End Results (SEER) database, this study included patients with low-grade endometrioid carcinoma of stage T1a to further verify and explore the above
controversial issues in terms of cancer-specific survival (CSS).
The SEER database is a comprehensive cancer statistics database managed by the National Cancer Institute. It collects data on the incidence, prevalence, survival, and mortality rates of
cancer in each region of the United States. This study used the SEER-17 dataset from 2000 to 2021, covering approximately 26.5% of the total U.S. population. Considering SEER database is
publicly available and does not require informed patient consent, therefore, ethical approval and informed consent were waived.
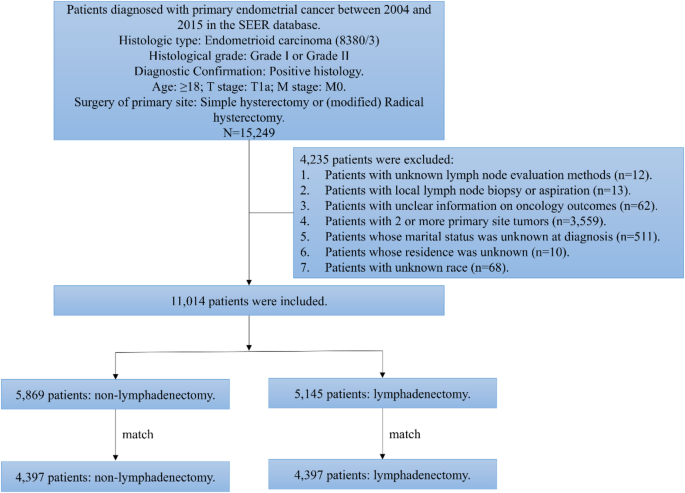
In this study, we identified primary endometrial cancer cases from 2004 to 2015 in the SEER-17 data set using the codes C54.1. All patients underwent either simple hysterectomy or (modified)
radical hysterectomy at the primary site (Surgery Codes: A400, A500, A600, A610; A620; A630; A640; A650; A660; A670). All patients had endometrioid carcinoma (8380/3), with a histological
grade of either Grade I or Grade II. The T stage of all patients was T1a and the M stage was M0. The study was limited to adults aged 18 years and older, all of whom were histologically
confirmed. During the screening process, we excluded cases with unknown lymph node evaluation methods and those with local lymph node biopsy or aspiration. In addition, we excluded patients
with unclear information on oncology outcomes, as well as patients with 2 or more primary site tumors. Last but not least, patients whose marital status was unknown at diagnosis, as well as
cases with missing information in residence and race, were not included in the final analysis. In the end, 11,014 patients were enrolled in the study. The patient selection process is shown
in Fig. 1.
Patient screening flow chart. SEER: Surveillance, Epidemiology, and End Results.
Based on the coding system of the SEER database, we obtained patients’ demographic characteristics (including age, marital status, median household income, place of residence, race and
ethnicity), oncology characteristics (including histological grade, and tumor size), and treatment measures (radiotherapy, and chemotherapy). In addition, we determined CSS based on the
patient’s final state and duration of follow-up.
In the subsequent statistical analysis, we divided the age at diagnosis into ≤ 60 years and > 60 years, and the marital status at diagnosis into married and unmarried (including single,
separated, divorced, widowed, and unmarried or domestic partner). Median household income was classified as 2 cm.
The patients were divided into non-lymphadenectomy group and lymphadenectomy group. Differences in baseline features between the two groups were determined by Pearson Chi-square test. The
tumor outcome measure we were interested in was CSS. Kaplan-Meier curves and Log-rank tests were used to assess differences in CSS between the two groups. Subsequently, to reduce the impact
of baseline differences on survival, we performed 1:1 propensity score matching (PSM). After PSM, Kaplan-Meier curves and Log-rank tests were used again to assess the effects of two groups
on CSS. In addition, subgroup analyses were performed based on predetermined variables. Finally, multivariate COX regression analysis was used to find the independent predictive factors on
CSS. All statistical analyses in this study were performed using R software (version 4.3.0). All P-values were bilateral, and the threshold of significance was set at 0.05.
The baseline characteristics of the included patients are shown in Table 1. A total of 11,014 patients were included, with a median follow-up of 127 months. Among them, 5,145 (46.7%)
patients had lymphadenectomy and 5,869 (53.3%) patients did not. There were 7,380 patients (67.0%) aged ≤ 60 years, and 3,634 patients (33.0%) aged > 60 years. In terms of demographics, most
patients were married (59.8%), white (82.3%), non-Hispanic (87.4%), had a median household income of more than 75,000 USD (53.7%), and lived in urban (88.2%). In terms of tumor
characteristics, there were 8,336 (75.7%) well differentiated (Grade I) patients, and 2,678 (24.3%) moderately differentiated (Grade II) patients. For tumor size of the primary site, 3,433
(31.2%) patients were ≤ 2 cm, 3,115 (28.3%) patients were > 2 cm, and 4,466 (40.5%) patients were unknown. In terms of treatment, 209 patients (1.9%) received radiotherapy, and 52 patients
(0.5%) received chemotherapy.
Before PSM, significant differences were observed between non-lymphadenectomy group and lymphadenectomy group in various aspects, including age (p