Use of the cytosorb adsorber in patients with acute-on-chronic liver failure
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT CytoSorb is a hemoadsorptive column used to remove high concentrations of proinflammatory cytokines in septic shock. Data on CytoSorb application in acute-on-chronic liver failure
(ACLF) is lacking. This retrospective observational study analyzed 21 ACLF patients admitted to ICUs at the Vienna General Hospital who received CytoSorb adsorber therapy between 2017 and
2023. Median ICU length of stay was 8 days (IQR: 3–13), the ICU survival rate was 23.8% (n = 5). Significant decreases in bilirubin (median peak: 20.7 mg/dL to median post-treatment: 10.8
mg/dL; − 47.8%; _p_ < 0.001), procalcitonin (1.34 to 0.74 pg/mL; − 44.6%; _p_ < 0.001), interleukin-6 (385 to 131 ng/mL; − 66.0%; _p_ = 0.0182)—but also of platelets (72 to 31 G/L; −
56.9%; _p_ = 0.0014) and fibrinogen (230 to 154 mg/dL; − 33.0%; _p_ = 0.0297) were detected. ICU survivors had a trend towards a stronger relative decrease in bilirubin (− 76.1% vs. −
48.2%), procalcitonin (− 90.6% vs. − 23.5%), and IL-6 (− 54.6% vs. − 17.8%) upon CytoSorb treatment. Moreover, no serious CytoSorb-attributed complications were detected. In conclusion, use
of CytoSorb adsorber in ACLF patients results in a significant decrease in bilirubin and proinflammatory cytokines, while platelets and fibrinogen were also lowered. Prospective trials are
warranted to investigate the impact of CytoSorb on clinical outcomes of ACLF patients with high proinflammatory cytokine levels. SIMILAR CONTENT BEING VIEWED BY OTHERS A CLINICAL STUDY OF
NON-BIOARTIFICIAL LIVER DPMAES SUPPORT SYSTEM IN HEPATITIS B-RELATED ACUTE-ON-CHRONIC LIVER FAILURE Article Open access 20 January 2024 SUCCESSFUL ELIMINATION OF BILIRUBIN IN CRITICALLY ILL
PATIENTS WITH ACUTE LIVER DYSFUNCTION USING A CYTOKINE ADSORBER AND ALBUMIN DIALYSIS: A PILOT STUDY Article Open access 13 May 2021 A MATCHED CASE-CONTROL STUDY ON THE EFFECTIVENESS OF
EXTRACORPOREAL CYTOKINE ADSORPTION IN CRITICALLY ILL PATIENTS Article Open access 18 August 2023 INTRODUCTION Acute-on-chronic liver failure (ACLF) is a syndrome that may occur in patients
with cirrhosis experiencing acute decompensation and is characterized by the development of hepatic and/or extra-hepatic organ failure(s), resulting in excessive short-term mortality1. It
has been demonstrated that systemic inflammation is the hallmark of ACLF driving disease development and progression1,2,3,4,5,6,7,8. The underlying mechanisms leading to systemic
inflammation in ACLF are only partly understood and depend on the specific precipitating event, which may be identified in up to 60% of cases7. Inflammation is associated with the release of
damage-associated (DAMPs) or pathogen-associated molecular patterns (PAMPs), resulting in oxidative stress triggering immune-mediated tissue damage, mitochondrial dysfunction, renal
hypoperfusion, and subsequently, single or multiple organ failures3,9. In line, Monteiro and colleagues recently demonstrated the impact of the inflammasome, as assessed by the
pro-inflammatory cytokines interleukin (IL)-1α and IL-1β, on ACLF outcome10. Therefore, amelioration of systemic inflammation, e.g., by clearance of pro-inflammatory cytokines, may be an
important therapeutic goal in ACLF patients in order to promote liver regeneration or as a bridging therapy to liver transplantation5,11,12. The CytoSorb adsorber is an extracorporeal blood
purification tool (hemoadsorber) that may be used together with continuous dialysis to remove excessive inflammatory mediators (i.e., cytokines), as well as to lower elevated bilirubin and
myoglobin levels13. Regarding liver-related indications, there is some data on the use of CytoSorb in patients with isolated hyperbilirubinemia and case series on liver failure14. However,
there is no data on the use of CytoSorb in the specific setting of ACLF. Previously, extracorporeal liver support devices failed to improve the prognosis of patients with ACLF15.
Extracorporeal treatment with large-volume plasma exchange—in order to eliminate pro-inflammatory cytokines—is explored as a promising treatment option in ACLF16. Moreover, a recently
published randomized, controlled clinical trial detected a significant decrease in biomarkers involved in the pathophysiological process of ACLF in patients treated with the liver dialysis
system DIALIVE compared to patients with standard medical treatment. Patients treated with the DIALIVE device showed an improvement in CLIF-C OF and CLIF-C ACLF scores but no significant
difference in 28-day mortality17. The results of a phase III study investigating the efficacy of plasma exchange in ACLF patients are still pending (APACHE, NCT03702920)18. Given the unmet
clinical need for supportive treatments in patients with ACLF, we aimed to investigate the impact of CytoSorb treatment on liver and extra-hepatic organ function and to evaluate potential
complications occurring during this treatment in critically ill ACLF patients. METHODS STUDY DESIGN AND SETTING We conducted a retrospective observational study of patients with ACLF
admitted to the ICU at a large tertiary center (Vienna General Hospital). Importantly, we did not include patients with acute liver failure (ALF) without pre-existing liver disease. All
adult (18 years and older) patients with ACLF receiving treatment with CytoSorb adsorber between January 1st, 2017, and January 1st, 2023, were included in this study. The diagnosis of ACLF
was defined according to the European Association for the Study of the Liver (EASL) CLIF criteria19. The observation period started from ICU admission (baseline) until ICU discharge or
death. We evaluated the effects of CytoSorb hemoadsorption on the clinical course, carefully screened for potential complications, and analyzed laboratory parameters directly prior to
CytoSorb application, after 24 h, and at the end of CytoSorb treatment (or last available in case of death). In addition, we included a control group comprising 10 patients with ACLF who
were all treated at the ICU during the respective time period 2017 to 2023 and received hemodialysis without the inclusion of the CytoSorb adsorber. HEMOADSORPTION WITH CYTOSORB ADSORBER All
included ACLF patients fulfilled an indication (i.e., acute kidney injury, hyperammonemia, and fluid- and acid–base disturbances) for hemodialysis during their respective ICU stay. The
decision for additional CytoSorb adsorber application was made by the treating physicians. Thereby, CytoSorb adsorber was always used in addition to standard intensive care treatment of ACLF
patients according to current EASL guidelines19. CytoSorb adsorber was always used with continuous venovenous hemodialysis (CVVHD; MultiFiltrate, Fresenius Medical Care) in prefilter
position and changed after 8–24 h. Anticoagulation during extracorporeal blood circulation was primarily conducted with citrate. In case of suspected citrate accumulation, the
anticoagulation regimen was switched to antithrombin III supplementation. According to our local standard operating procedures, citrate accumulation is rigorously monitored at least 3 times
daily in patients with liver failure using the total calcium to ionized calcium ratio20. Dialysis with low-molecular-weight heparin was not applied in our patient cohort, nor was dialysis
without anticoagulation21. Laboratory parameters including liver chemistry [bilirubin, aspartate transferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (aP), gamma-glutamyl
transferase (GGT), and ammonia], inflammation parameters [procalcitonin (PCT), interleukin-6 (IL-6), C-reactive protein (CRP)], coagulation parameters [fibrinogen, international normalized
ratio (INR)], white blood count (WBC) and platelets were collected in all patients and analyzed prior to CytoSorb application, 24 h after the commencement of CytoSorb therapy and after
discontinuation of CytoSorb therapy (or prior to death). Overall CytoSorb treatment time and all CytoSorb adsorber changes were documented. For the evaluation of potential adverse events or
complications directly associated with CytoSorb therapy, the patient's condition and laboratory changes were closely monitored during hemoadsorption in standardized time intervals. DATA
COLLECTION Data were extracted from electronic patient charts (IntelliSpace Critical Care and Anesthesia, Philips, Amsterdam, Netherlands) that are routinely used at all ICUs at the Vienna
General Hospital. The system enables prospective and digital documentation of crucial patient data, including patient characteristics (age, gender, height, weight, BMI, vital signs and
comorbidities/underlying disease), laboratory tests (blood chemistry, global tests of coagulation and blood cell count) and complete information about ICU-specific parameters like fluid
balances, medication, nutrition and extracorporeal life support (mechanical ventilation, renal replacement therapy and ECMO). In order to quantify the severity of critical illness and extent
of organ dysfunction for patients admitted to the ICU, we calculated the following scores within the first 24 h upon ICU admission: simplified acute physiology score (SAPS II)22 and
sequential organ failure assessment score (SOFA)23. In addition, CLIF-C-ACLF and CLIF-C-OF scores were calculated as ACLF-specific prognostic scores24,25. Child–Pugh-Score (CPS) was
collected using laboratory data and clinical parameters at ICU admission26,27. STATISTICAL ANALYSIS Descriptive statistical analysis was used to provide a demographic overview of our patient
cohort. Continuous variables were reported as mean ± standard deviation or median (interquartile range), while categorical variables were reported as numbers (relative proportions, %).
Differences in laboratory parameters before and after CytoSorb adsorber application were compared using the Wilcoxon test for non-parametric variables. All statistical analyses were
performed using IBM SPSS Statistics 27 (IBM, New York, NY, USA) and GraphPad Prism 8 (GraphPad Software, CA, USA). ETHICAL APPROVAL AND INFORMED CONSENT The study was conducted according to
the guidelines of the Declaration of Helsinki28, and approved by the local Ethics Committee of the Medical University of Vienna (Ethics committee number: 1924/2020). Given the retrospective
design of the study, informed consent requirement was waived by the ethics committee of the Medical University of Vienna. RESULTS PATIENT CHARACTERISTICS During the study period, 21 patients
with ACLF were admitted to the ICU and received CytoSorb adsorber therapy (Supplemental Figure S1). The baseline characteristics of our patient population are depicted in Table 1. The
individual characteristics of each patient are shown in Table 2. The median age was 50 years (IQR: 35–58), and most patients were male (n = 18; 86%). SOFA and SAPS II scores at ICU admission
were 16 (IQR: 13–19) and 59 (IQR: 53–69), respectively. The most common underlying etiology of cirrhosis was alcohol-related liver disease (ALD; n = 11), followed by primary sclerosing
cholangitis (PSC, n = 4), re-cirrhosis after LTX (n = 2), autoimmune hepatitis (AIH; n = 1), porphyria (n = 1), chronic hepatitis B (n = 1) and secondary sclerosing cholangitis (n = 1). At
the time of ICU admission, most patients presented with CPS C (n = 16), while 5 patients showed CPS B. The median CPS score was 12 (IQR: 10–14). Infections (n = 12) and gastrointestinal
bleeding events (n = 8) were the main precipitating events for the development of ACLF. The median number of organ failures at ICU admission was 4 (IQR: 4–6), corresponding to a median
CLIF-C ACLF and CLIF-C OF Score of 67 (IQR: 57–76) and 15 (IQR: 14–18), respectively. We reported a median ICU length of stay (LOS) of 8 days (IQR: 3–13) and an ICU survival rate of 23.8% (n
= 5). Additionally, we detected a 1-month survival of 23.8% (n = 5) and a 3-month survival of 19% (n = 4). Based on the CLIF-C-ACLF score, a predicted 1-month mortality of 82% and a
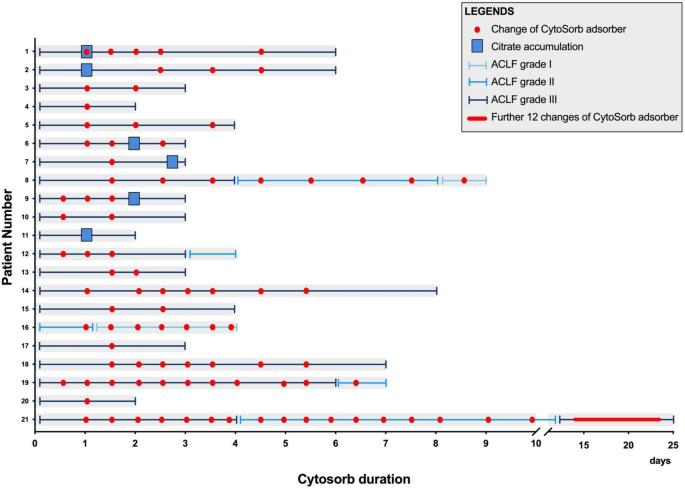
predicted 3-month mortality of 92.9% were determined. Detailed information on the individual patients’ courses during CytoSorb adsorber application is shown in Fig. 1 and Supplemental Figure
S2. The temporal relationship between CVVHD, CytoSorb application, outcome, and anticoagulation is depicted in Supplemental Table S1. All but one patient (95.2%) required vasopressor (i.e.,
noradrenaline) therapy during ICU stay. A detailed description of noradrenaline doses during CytoSorb treatment is depicted in Supplemental Table S2. In 10 patients, an increase in
noradrenalin dose was observed 6 h after the start of CytoSorb treatment. After discontinuation of CytoSorb therapy, 6 patients (28.6%) were resolved from vasopressors. In addition,
mechanical invasive ventilation (MIV) was conducted in 18 patients with a median length of MIV of 4 days (IQR: 2–8). Differences in baseline characteristics between survivors and
non-survivors are shown in Table 1. Survivors were younger (47 vs. 51 years), showed a lower CLIF-C-ACLF score at ICU admission (60 vs. 68.5), and had a longer ICU LOS (9 vs. 5.5 days).
CHANGES IN LABORATORY PARAMETERS The median number of CytoSorb applications per patient was 4 (IQR: 2.5–8), with a median CytoSorb therapy duration of 64 h (IQR: 42.5–130). We found a
significant decrease in bilirubin levels during and after CytoSorb therapy (median peak: 20.7 mg/dL to median post-treatment: 10.8 mg/dL; – 47.8%; _p_ < 0.001; Fig. 2). Interestingly,
these changes were already observed after 24 h of CytoSorb treatment (median peak: 20.7 mg/dL to median 24 h-treatment: 13.8 mg/dL; – 33.3%; _p_ < 0.001; Fig. 2a). Except for a
significant decrease in GGT levels after 24 h (median peak: 47 U/L to median post 24 h-treatment: 32 U/L; – 31.9%; _p_ = 0.0018), we did not find a clear trend for the remaining liver
chemistries. WBC, CRP, PCT, and IL-6 were monitored as surrogate parameters for systemic inflammation. While CytoSorb therapy did not affect WBC and CRP levels, we observed a significant
decline in PCT levels (median peak: 1.34 ng/mL to median 24 h-treatment: 1.09 ng/mL; – 18.4%; _p_ < 0.001) 24 h after first CytoSorb adsorber therapy (Fig. 3a). There was also a relevant
but non-significant trend regarding the decline in IL-6 levels after 24 h of CytoSorb therapy (median peak: 385 pg/mL to median 24 h-treatment: 327 pg/mL; – 15.2%; _p_ = 0.0599).
Importantly, after total CytoSorb therapy, both PCT (median peak: 1.34 ng/mL to median post-treatment: 0.74 ng/mL; – 44.9%; _p_ < 0.001) and IL-6 (median peak: 385 pg/mL to median
post-treatment: 131 ng/mL; – 66.1%; _p_ = 0.0182) showed a significant decrease (Fig. 3b). In addition, the 5 ICU survivors tended to have a stronger initial decrease in bilirubin (– 76.1%
vs. – 48.2%), procalcitonin (– 90.6% vs. – 23.5%), and IL-6 (– 54.6.3% vs. – 17.8%) upon CytoSorb treatment compared to non-survivors. In order to analyze if the aforementioned changes in
laboratory parameters were achieved by the addition of CytoSorb adsorber to CVVHD and not by conventional hemodialysis alone, we also evaluated laboratory changes in patients with ACLF and
CVVHD without inclusion of the CytoSorb adsorber. The basic characteristics of this control group are depicted in Supplemental Table S3–S4. As seen in Supplemental Table S5, CVVHD without
CytoSorb had no significant impact on the investigated laboratory parameters. In the control group, we detected a noticeable but not statistically significant decrease in median ammonia
levels after 24 h and at CVVHD discontinuation. FEASIBILITY, SAFETY, AND COMPLICATIONS OF CYTOSORB THERAPY IN ACLF PATIENTS We found a significant decrease in platelet counts during and
after CytoSorb therapy (median peak: 72 G/L to median post-treatment: 31 G/L; – 56.9%; _p_ = 0.0014; Fig. 4). These changes could already be detected 24 h after the start of CytoSorb
treatment (median pre-treatment: 72 G/L to median 24 h-treatment: 44 G/L; – 38.9%; _p_ = 0.043). Concerning global coagulation tests, we observed a significant increase in INR after 24 h of
CytoSorb therapy (median pre-treatment: 2.5 to median 24-treatment: 3.2; 28%; _p_ = 0.0215). In addition, fibrinogen levels showed a significant decrease during the course of CytoSorb
therapy (median pre-treatment: 230 mg/dL to median post-treatment: 154 mg/dL; 33%; _p_ = 0.0297). We did not observe any bleeding or other complications (i.e., allergic reactions) attributed
to treatment with the CytoSorb adsorber in our ACLF patient cohort. In all patients, the CytoSorb adsorber was combined with CVVHD using regional citrate anticoagulation by local standards.
In our ACLF cohort, citrate accumulation was suspected in 6 (28.6%) patients, and in all of these cases, citrate anticoagulation was replaced by substituting antithrombin III (Fig. 1 and
Supplemental Table S1)21. In these patients, antithrombin III anticoagulation was continued for the remaining CVVHD circuits. DISCUSSION Here we provide first observational data on the use
of the CytoSorb adsorber as supportive therapy in ACLF patients. Importantly, we detected a significant reduction of bilirubin after 24 h and at the end of CytoSorb application in all ACLF
patients. In addition, CytoSorb therapy also led to a significant decrease in PCT and IL-6 levels after CytoSorb application, indicating a potential benefit by ameliorating the systemic
proinflammatory state in ACLF. We also found a significant decrease in platelets and alterations in the plasmatic coagulation, but did not detect bleeding and other complications directly
attributed to CytoSorb use. The integration of CytoSorb in an extracorporeal circuit to modulate hyperinflammation (‘cytokine storm’) in sepsis represents a novel therapeutic approach first
introduced in 200829,30,31. CytoSorb treatment has been approved in Europe since 2011 and is authorized for use as an additional treatment for all indications associated with elevated
cytokine levels. In animal studies, CytoSorb treatment was able to reduce inflammation-related molecules such as IL-6, IL-10, and TNF- α32,33. _Brouwer _et al. demonstrated reduced 28-day
mortality in septic patients treated with CytoSorb31. Supporting data for the use of CytoSorb in the setting of ACLF are derived from patients with ALF (i.e., notably a different setting)
occurring in patients with sepsis and systemic inflammation. Importantly, systemic inflammation is a key risk factor for the development and progression of ACLF6,8. Therapy with CytoSorb
adsorber in ACLF patients is used with the rationale to ameliorate a hyperinflammatory state and thereby promote liver regeneration5,11,12. While we did not find any clear trend regarding
CRP and WBC during and after CytoSorb treatment, we detected a significant decline in PCT and IL-6 levels13. Importantly, the declines in PCT and IL-6 levels were already evident as early as
24 h after the start of CytoSorb application, i.e., in a critical early phase of ACLF. This finding argues for a direct effect of the CytoSorb adsorber on these proinflammatory parameters.
However, in our study, the reported decrease in IL-6 was rather small compared to in vitro data34. An explanation for the discrepancy between in vitro experiments and clinical application
might be the constant hyperinflammatory response during ACLF, especially at the beginning of the disease course. In this regard, the observed small decrease of IL-6 by CytoSorb therapy might
indicate a successful dampening of hyperinflammation that would have otherwise happened. Similar effects could already be seen in a study investigating the effects of CytoSorb hemoperfusion
on systemic inflammation in humans in vivo35. We also found a significant decrease in bilirubin levels during hemoadsorption, confirming data from other studies analyzing the effects of
CytoSorb in different settings14,36,37,38,39. Again, these effects could already be achieved as early as 24 h after the commencement of CytoSorb therapy. According to recent data, the impact
of CytoSorb treatment on bilirubin removal is even more effective compared to MARS13,40. However, the removal of further clinically relevant metabolites accumulating during liver failure by
the CytoSorb adsorber is still unclear and under debate. Effects on hyperammonemia have been reported mainly in ex vivo studies40,41. However, recent data from one clinical report indicate
that CytoSorb does not directly affect ammonia levels, and the elimination may be mainly achieved through simultaneously applied hemodialysis42. Interestingly, we found a more pronounced
decrease in median ammonia levels in the control group, which only received CVVHD. However, the sample size was small, and the results were not statistically significant. It is yet not clear
how CytoSorb application influences ammonia levels in patients with ACLF. Recent data suggests that the decrease in ammonia levels is a primary effect of hemodialysis, which is a
perquisition for CytoSorb use43. However, we do not think CytoSorb negatively affects serum ammonia levels. Therefore, the observed difference in the clearance of ammonia levels between the
CytoSorb group and the control group is likely due to the small sample size in both subgroups. Further studies are needed to investigate the impact of CytoSorb therapy on hyperammonemia and
encephalopathy during liver failure. Nevertheless, our findings suggest that hemoadsorption with CytoSorb might support blood detoxification during ACLF. Besides standard medical treatment,
there is considerable interest in extracorporeal liver support systems for patients with liver failure15,44. Artificial liver support devices, such as MARS, Prometheus, and single-pass
albumin dialysis (SPAD), led to an amelioration of laboratory parameters in ACLF. However, no consistent improvement in survival was found compared to standard medical treatment15,44. A
prospective, randomized controlled trial reported no benefit in laboratory chemistries and outcome in ACLF patients treated with ELAD45. Potential positive effects were reported in ALF
patients with high volume plasma exchange, while a survival benefit in ACLF patients is debated controversially15. There is a lack of data on the efficacy of CytoSorb adsorber in the
specific setting of ACLF. In a recent retrospective study of a small patient cohort with liver failure (ALF and ACLF) by _Popescu _et al.40, CytoSorb therapy was found to be equally or even
more effective in rebalancing liver functional tests in patients with liver failure compared to MARS. However, there were no differences in patient outcome40. Nevertheless, CytoSorb adsorber
is a rather cheap, easy-to-use, and readily available blood purification tool installed in conventional hemodialysis, which could also be used in smaller centers, in contrast to artificial
liver support devices, that often require significant expertise for their application38. The application of CytoSorb adsorber is generally associated with a low risk of complications46. In
our cohort of ACLF patients, platelets were significantly decreased, as reported in other studies using renal replacement therapy with CytoSorb adsorber40,47. Moreover, we detected changes
in plasmatic coagulation, including a significant decrease in fibrinogen levels and an increase in INR after the commencement of CytoSorb that may, however, also be due to liver disease
progression. We did not detect bleeding complications or other adverse effects directly associated with the use of CytoSorb adsorber therapy. In 10 patients CytoSorb application was
accompanied by increased vasopressor requirements shortly after commencement of adsorber therapy. This observation is best explained by progressive multiorgan failure and refractory shock in
ACLF grade 3 rather than a negative impact of CytoSorb adsorber on hemodynamics itself. Due to an imbalance of coagulation and risk of bleeding, regional citrate dialysis was used in all
our patients, and a switch to antithrombin III supplementation due to citrate accumulation was only rarely necessary. Nevertheless, citrate accumulation was detected in 6 patients. In our
experience, the risk for citrate accumulation is highest during the first cycle of CVVHD when the patient is still in an unstable condition. In this situation, the already limited liver
function is further compromised by circulatory/septic shock, resulting in the inability to metabolize citrate and ultimately leading to citrate accumulation20. In this regard, citrate
accumulation might also represent a negative prognostic marker for outcome in ACLF patients48. The ICU survival of our study population was rather low, with 23.8%. However, our patients were
admitted to the ICU with advanced ACLF as indicated by high CLIF-C ACLF scores and CLIF-OF scores at ICU admission corresponding to a predicted 1-month and 3-month mortality of 82% and
92.9%, respectively. 95.2% of our patients had an ACLF grade 3 before CytoSorb application. In our small study population, we observed comparable numbers with a 1-month mortality of 76.2%
and 3-month mortality of 81%. Similar outcome data concerning ACLF patients was reported in the CANONIC study (28-day = 76.7%; 90-day mortality = 79.1%)1. Overall, in patients with advanced
ACLF stages, treatment with CytoSorb adsorber might be less effective as organ failures may no longer be reversible. Therefore, close monitoring of organ function and, consequently, the
earlier application of CytoSorb adsorber in ACLF patients might represent a treatment strategy to prevent disease progression to multiorgan failure (i.e., bridge to recovery) or to enable
liver transplantation5,49,50. Indeed, liver transplantation for ACLF patients has shown very promising results, with a 1-year probability of survival after liver transplantation of 81%50.
Unfortunately, liver transplantation for ACLF patients is not established at our center. Therefore, none of our patients was even evaluated for eligibility for liver transplantation. The
present study has limitations: First, in our single center study, we only report the data of a rather small cohort, including 21 ACLF patients treated with CytoSorb adsorber. However, to our
knowledge, this is the first study to date that investigates the effects of hemoadsorption with CytoSorb in the specific setting of ACLF—while others have included patients with ALF in
other settings15,40. Second, due to the retrospective design, we had some missing laboratory values, especially for ammonia, but also for PCT and IL-6, which may therefore introduce a bias
in the interpretation of the results. Third, we acknowledge that in addition to CytoSorb therapy, patients always received standard medical treatment, including hemodialysis, according to
the EASL guidelines19. Therefore, it is unclear to what extent the laboratory changes may be allocated to hemoadsorption or standard medical treatment. However, we found significant changes
in a couple of laboratory parameters 24 h after the commencement of CytoSorb treatment, suggesting a direct effect of hemoadsorption. Fourth, due to the small number of patients in the
control group, we were not able to perform a propensity matched comparison. Future multicenter prospective trials are required to provide a more comprehensive comparison regarding the
efficacy of CVVHD + CytoSorb therapy and CVVHD alone in patients with ACLF. Nevertheless, we here present a comprehensive summary of our single center experience using CytoSorb adsorber in
ACLF patients. CONCLUSIONS Our study supports the use of CytoSorb adsorber as a feasible and easy-to-use blood purification tool with few complications in patients with ACLF. CytoSorb
treatment led to a significant decrease in important surrogate markers of systemic inflammation and supported blood detoxification by removing bilirubin in ACLF patients. Larger randomized
controlled trials are warranted to further investigate the clinical value of CytoSorb therapy in ACLF patients. DATA AVAILABILITY Data are available from the corresponding author upon
reasonable request. ABBREVIATIONS * ACLF: Acute-on-chronic liver failure * ALD: Alcoholic liver disease * ALF: Acute liver failure * ALT: Alanine aminotransferase * aP: Alkaline phosphatase
* AIH: Autoimmune hepatitis * AST: Aspartate transferase * CRP: C-reactive protein * CVVHD: Continuous venovenous hemodialysis * CPS: Child–Pugh-score * DAMP: Damage-associated molecular
patterns * EASL: European Association for the Study of the Liver * GGT: Gamma-glutamyl transferase * ICU: Intensive Care Unit * IL-6: Interleukin-6 * INR: International normalized ratio *
IQR: Interquartile range * LOS: Length of stay * LTX: Liver transplantation * MCI: Myocardial infarction * MIV: Mechanical invasive ventilation * MOF: Multi organ failure * PAMP:
Pathogen-associated molecular patterns * PCT: Procalcitonin * Pt.: Patient * PSC: Primary sclerosing cholangitis * RC: Re-cirrhosis * SAPS II: Simplified acute physiology score * SOFA:
Sequential organ failure assessment score * VP: Vasopressor * WBC: White blood count REFERENCES * Moreau, R. _et al._ Acute-on-chronic liver failure is a distinct syndrome that develops in
patients with acute decompensation of cirrhosis. _Gastroenterology_ 144, 1426–1437, 1437.e1421–1429. https://doi.org/10.1053/j.gastro.2013.02.042 (2013). * Arroyo, V. _et al._ The systemic
inflammation hypothesis: Towards a new paradigm of acute decompensation and multiorgan failure in cirrhosis. _J. Hepatol._ 74, 670–685. https://doi.org/10.1016/j.jhep.2020.11.048 (2021).
Article CAS PubMed Google Scholar * Engelmann, C., Clària, J., Szabo, G., Bosch, J. & Bernardi, M. Pathophysiology of decompensated cirrhosis: Portal hypertension, circulatory
dysfunction, inflammation, metabolism and mitochondrial dysfunction. _J. Hepatol._ 75(Suppl 1), S49-s66. https://doi.org/10.1016/j.jhep.2021.01.002 (2021). Article CAS PubMed PubMed
Central Google Scholar * Arroyo, V., Moreau, R., Jalan, R. & Ginès, P. Acute-on-chronic liver failure: A new syndrome that will re-classify cirrhosis. _J. Hepatol._ 62, S131-143.
https://doi.org/10.1016/j.jhep.2014.11.045 (2015). Article PubMed Google Scholar * Trebicka, J., Sundaram, V., Moreau, R., Jalan, R. & Arroyo, V. Liver transplantation for
acute-on-chronic liver failure: Science or fiction?. _Liver Transpl._ 26, 906–915. https://doi.org/10.1002/lt.25788 (2020). Article PubMed Google Scholar * Balcar, L. _et al._ Patterns of
acute decompensation in hospitalized patients with cirrhosis and course of acute-on-chronic liver failure. _United Eur. Gastroenterol. J._ 9, 427–437. https://doi.org/10.1002/ueg2.12089
(2021). Article CAS Google Scholar * Trebicka, J. _et al._ PREDICT identifies precipitating events associated with the clinical course of acutely decompensated cirrhosis. _J. Hepatol._
74, 1097–1108. https://doi.org/10.1016/j.jhep.2020.11.019 (2021). Article PubMed Google Scholar * Trebicka, J. _et al._ The PREDICT study uncovers three clinical courses of acutely
decompensated cirrhosis that have distinct pathophysiology. _J. Hepatol._ 73, 842–854. https://doi.org/10.1016/j.jhep.2020.06.013 (2020). Article PubMed Google Scholar * Arroyo, V.,
Moreau, R. & Jalan, R. Acute-on-chronic liver failure. _N Engl. J. Med._ 382, 2137–2145. https://doi.org/10.1056/NEJMra1914900 (2020). Article CAS PubMed Google Scholar * Monteiro,
S. _et al._ Differential inflammasome activation predisposes to acute-on-chronic liver failure in human and experimental cirrhosis with and without previous decompensation. _Gut_ 70,
379–387. https://doi.org/10.1136/gutjnl-2019-320170 (2021). Article CAS PubMed Google Scholar * Bernal, W., Karvellas, C., Saliba, F., Saner, F. H. & Meersseman, P. Intensive care
management of acute-on-chronic liver failure. _J. Hepatol._ 75(Suppl 1), S163-s177. https://doi.org/10.1016/j.jhep.2020.10.024 (2021). Article PubMed Google Scholar * Caraceni, P.,
Abraldes, J. G., Ginès, P., Newsome, P. N. & Sarin, S. K. The search for disease-modifying agents in decompensated cirrhosis: From drug repurposing to drug discovery. _J. Hepatol._
75(Suppl 1), S118-s134. https://doi.org/10.1016/j.jhep.2021.01.024 (2021). Article CAS PubMed Google Scholar * Dominik, A. & Stange, J. Similarities, differences, and potential
synergies in the mechanism of action of albumin dialysis using the MARS albumin dialysis device and the CytoSorb hemoperfusion device in the treatment of liver failure. _Blood Purif._ 50,
119–128. https://doi.org/10.1159/000508810 (2021). Article CAS PubMed Google Scholar * Ocskay, K. _et al._ Hemoadsorption in “liver indication’-analysis of 109 patients” data from the
CytoSorb international registry. _J. Clin. Med._ 10, 5182. https://doi.org/10.3390/jcm10215182 (2021). Article CAS PubMed PubMed Central Google Scholar * Ocskay, K. _et al._ Uncertainty
in the impact of liver support systems in acute-on-chronic liver failure: A systematic review and network meta-analysis. _Ann. Intensive Care_ 11, 10.
https://doi.org/10.1186/s13613-020-00795-0 (2021). Article PubMed PubMed Central Google Scholar * Maiwall, R. _et al._ Therapeutic plasma-exchange improves systemic inflammation and
survival in acute-on-chronic liver failure: A propensity-score matched study from AARC. _Liver Int._ 41, 1083–1096. https://doi.org/10.1111/liv.14806 (2021). Article CAS PubMed Google
Scholar * Agarwal, B. _et al._ Randomized, controlled clinical trial of the DIALIVE liver dialysis device versus standard of care in patients with acute-on- chronic liver failure. _J.
Hepatol._ 79, 79–92. https://doi.org/10.1016/j.jhep.2023.03.013 (2023). Article PubMed Google Scholar * Stahl, K., Bode, C. & David, S. Bridging patients with acute-on-chronic liver
failure for transplantation: plasma exchange to stabilize multiorgan failure?. _Intensive Care Med._ 49, 890–891. https://doi.org/10.1007/s00134-023-07092-x (2023). Article PubMed PubMed
Central Google Scholar * European Association for the Study of the Liver. Electronic address, e. e. e. & European Association for the Study of the, L. EASL Clinical Practice Guidelines
for the management of patients with decompensated cirrhosis. _J. Hepatol._ 69, 406–460. https://doi.org/10.1016/j.jhep.2018.03.024 (2018). * Schneider, A. G., Journois, D. & Rimmele, T.
Complications of regional citrate anticoagulation: Accumulation or overload?. _Crit. Care_ 21, 281. https://doi.org/10.1186/s13054-017-1880-1 (2017). Article PubMed PubMed Central Google
Scholar * Brunner, R., Leiss, W., Madl, C., Druml, W. & Holzinger, U. Single-dose application of antithrombin as a potential alternative anticoagulant during continuous renal
replacement therapy in critically ill patients with advanced liver cirrhosis: A retrospective data analysis. _Anesth. Analg._ 116, 527–532. https://doi.org/10.1213/ANE.0b013e31827ced39
(2013). Article CAS PubMed Google Scholar * Le Gall, J. R., Lemeshow, S. & Saulnier, F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American
multicenter study. _JAMA_ 270, 2957–2963. https://doi.org/10.1001/jama.270.24.2957 (1993). Article PubMed Google Scholar * Vincent, J. L. _et al._ The SOFA (Sepsis-related Organ Failure
Assessment) score to describe organ dysfunction/failure On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. _Intensive Care Med._
22, 707–710. https://doi.org/10.1007/BF01709751 (1996). Article CAS PubMed Google Scholar * Jalan, R. _et al._ Development and validation of a prognostic score to predict mortality in
patients with acute-on-chronic liver failure. _J. Hepatol._ 61, 1038–1047. https://doi.org/10.1016/j.jhep.2014.06.012 (2014). Article PubMed Google Scholar * Lee, M. _et al._ CLIF-SOFA
scoring system accurately predicts short-term mortality in acutely decompensated patients with alcoholic cirrhosis: A retrospective analysis. _Liver Int._ 35, 46–57.
https://doi.org/10.1111/liv.12683 (2015). Article PubMed Google Scholar * Child, C. G. & Turcotte, J. G. Surgery and portal hypertension. _Major Probl. Clin. Surg._ 1, 1–85 (1964).
CAS PubMed Google Scholar * Pugh, R. N., Murray-Lyon, I. M., Dawson, J. L., Pietroni, M. C. & Williams, R. Transection of the oesophagus for bleeding oesophageal varices. _Br. J.
Surg._ 60, 646–649. https://doi.org/10.1002/bjs.1800600817 (1973). Article CAS PubMed Google Scholar * World Medical, A. World Medical Association Declaration of Helsinki: ethical
principles for medical research involving human subjects. _JAMA_ 310, 2191–2194. https://doi.org/10.1001/jama.2013.281053 (2013). * Paul, R. _et al._ Multicentered prospective investigator
initiated study to evaluate the clinical outcomes with extracorporeal cytokine adsorption device (CytoSorb(®)) in patients with sepsis and septic shock. _World J. Crit. Care Med._ 10, 22–34.
https://doi.org/10.5492/wjccm.v10.i1.22 (2021). Article PubMed PubMed Central Google Scholar * Zuccari, S. _et al._ Changes in cytokines, haemodynamics and microcirculation in patients
with sepsis/septic shock undergoing continuous renal replacement therapy and blood purification with CytoSorb. _Blood Purif_ 49, 107–113. https://doi.org/10.1159/000502540 (2020). Article
CAS PubMed Google Scholar * Brouwer, W. P., Duran, S., Kuijper, M. & Ince, C. Hemoadsorption with CytoSorb shows a decreased observed versus expected 28-day all-cause mortality in ICU
patients with septic shock: A propensity-score-weighted retrospective study. _Crit. Care_ 23, 317. https://doi.org/10.1186/s13054-019-2588-1 (2019). Article PubMed PubMed Central Google
Scholar * Kellum, J. A., Song, M. & Venkataraman, R. Hemoadsorption removes tumor necrosis factor, interleukin-6, and interleukin-10, reduces nuclear factor-kappaB DNA binding, and
improves short-term survival in lethal endotoxemia. _Crit. Care Med._ 32, 801–805. https://doi.org/10.1097/01.ccm.0000114997.39857.69 (2004). Article CAS PubMed Google Scholar * Peng, Z.
Y., Carter, M. J. & Kellum, J. A. Effects of hemoadsorption on cytokine removal and short-term survival in septic rats. _Crit. Care Med._ 36, 1573–1577.
https://doi.org/10.1097/CCM.0b013e318170b9a7 (2008). Article CAS PubMed PubMed Central Google Scholar * Malard, B., Lambert, C. & Kellum, J. A. In vitro comparison of the adsorption
of inflammatory mediators by blood purification devices. _Intensive Care Med. Exp._ 6, 12. https://doi.org/10.1186/s40635-018-0177-2 (2018). Article PubMed PubMed Central Google Scholar
* Jansen, A., Waalders, N. J. B., van Lier, D. P. T., Kox, M. & Pickkers, P. CytoSorb hemoperfusion markedly attenuates circulating cytokine concentrations during systemic inflammation
in humans in vivo. _Crit. Care_ 27, 117. https://doi.org/10.1186/s13054-023-04391-z (2023). Article PubMed PubMed Central Google Scholar * Piwowarczyk, P. _et al._ Hemoadsorption in
isolated conjugated hyperbilirubinemia after extracorporeal membrane oxygenation support Cholestasis of sepsis: A case report and review of the literature on differential causes of jaundice
in ICU patient. _Int. J. Artif. Organs_ 42, 263–268. https://doi.org/10.1177/0391398819834012 (2019). Article CAS PubMed Google Scholar * Faltlhauser, A. & Kullmann, F. Use of
hemoadsorption in a case of severe hepatic failure and hyperbilirubinemia. _Blood Purif._ 44, 98–99. https://doi.org/10.1159/000470826 (2017). Article PubMed Google Scholar * Scharf, C.
_et al._ Successful elimination of bilirubin in critically ill patients with acute liver dysfunction using a cytokine adsorber and albumin dialysis: a pilot study. _Sci. Rep._ 11, 10190.
https://doi.org/10.1038/s41598-021-89712-4 (2021). Article ADS CAS PubMed PubMed Central Google Scholar * Dhokia, V. D., Madhavan, D., Austin, A. & Morris, C. G. Novel use of
Cytosorb haemadsorption to provide biochemical control in liver impairment. _J. Intensive Care Soc._ 20, 174–181. https://doi.org/10.1177/1751143718772789 (2019). Article CAS PubMed
Google Scholar * Popescu, M. _et al._ Artificial liver support with CytoSorb and MARS in liver failure: A retrospective propensity matched analysis. _J. Clin. Med._ 12, 2258.
https://doi.org/10.3390/jcm12062258 (2023). Article CAS PubMed PubMed Central Google Scholar * Tomescu, D., Popescu, M., David, C., Sima, R. & Dima, S. Haemoadsorption by
CytoSorb(R) in patients with acute liver failure: A case series. _Int. J. Artif. Organs_ 44, 560–564. https://doi.org/10.1177/0391398820981383 (2021). Article CAS PubMed Google Scholar *
Liebchen, U., Scharf, C., Zoller, M., Weinelt, F. & Kloft, C. No clinically relevant removal of meropenem by cytokine adsorber CytoSorb(®) in critically ill patients with sepsis or
septic shock. _Intensive Care Med._ 47, 1332–1333. https://doi.org/10.1007/s00134-021-06487-y (2021). Article CAS PubMed PubMed Central Google Scholar * Liebchen, U. _et al._ The
cytokine adsorber Cytosorb(R) does not reduce ammonia concentrations in critically ill patients with liver failure. _Intensive Care Med._ 49, 360–362.
https://doi.org/10.1007/s00134-023-06998-w (2023). Article CAS PubMed PubMed Central Google Scholar * Abbas, N., Rajoriya, N., Elsharkawy, A. M. & Chauhan, A. Acute-on-chronic liver
failure (ACLF) in 2022: Have novel treatment paradigms already arrived?. _Expert Rev. Gastroenterol. Hepatol._ 16, 639–652. https://doi.org/10.1080/17474124.2022.2097070 (2022). Article
CAS PubMed Google Scholar * Thompson, J. _et al._ Extracorporeal cellular therapy (ELAD) in severe alcoholic hepatitis: A multinational, prospective, controlled, randomized trial. _Liver
Transpl._ 24, 380–393. https://doi.org/10.1002/lt.24986 (2018). Article PubMed PubMed Central Google Scholar * Poli, E. C., Rimmele, T. & Schneider, A. G. Hemoadsorption with
CytoSorb((R)). _Intensive Care Med._ 45, 236–239. https://doi.org/10.1007/s00134-018-5464-6 (2019). Article PubMed Google Scholar * Alharthy, A. _et al._ Continuous renal replacement
therapy with the addition of CytoSorb cartridge in critically ill patients with COVID-19 plus acute kidney injury: A case-series. _Artif. Organs_ 45, E101–E112.
https://doi.org/10.1111/aor.13864 (2021). Article CAS PubMed Google Scholar * Khadzhynov, D. _et al._ Incidence and outcome of metabolic disarrangements consistent with citrate
accumulation in critically ill patients undergoing continuous venovenous hemodialysis with regional citrate anticoagulation. _J. Crit. Care_ 29, 265–271.
https://doi.org/10.1016/j.jcrc.2013.10.015 (2014). Article CAS PubMed Google Scholar * Li, X., Zhang, L., Pu, C. & Tang, S. Liver transplantation in Acute-on-Chronic liver failure:
Timing of transplantation and selection of patient population. _Front. Med. (Lausanne)_ 9, 1030336. https://doi.org/10.3389/fmed.2022.1030336 (2022). Article PubMed Google Scholar *
Belli, L. S. _et al._ Liver transplantation for patients with acute-on-chronic liver failure (ACLF) in Europe: Results of the ELITA/EF-CLIF collaborative study (ECLIS). _J. Hepatol._ 75,
610–622. https://doi.org/10.1016/j.jhep.2021.03.030 (2021). Article PubMed Google Scholar Download references AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Intensive Care Unit 13H1,
Division of Gastroenterology and Hepatology, Department of Medicine III, Medical University of Vienna, Waehringer Guertel 18-20, 1090, Vienna, Austria Patrick Haselwanter, Bernhard Scheiner,
Lorenz Balcar, Georg Semmler, Marlene Riedl-Wewalka, Monika Schmid, Thomas Reiberger, Christian Zauner & Mathias Schneeweiss-Gleixner Authors * Patrick Haselwanter View author
publications You can also search for this author inPubMed Google Scholar * Bernhard Scheiner View author publications You can also search for this author inPubMed Google Scholar * Lorenz
Balcar View author publications You can also search for this author inPubMed Google Scholar * Georg Semmler View author publications You can also search for this author inPubMed Google
Scholar * Marlene Riedl-Wewalka View author publications You can also search for this author inPubMed Google Scholar * Monika Schmid View author publications You can also search for this
author inPubMed Google Scholar * Thomas Reiberger View author publications You can also search for this author inPubMed Google Scholar * Christian Zauner View author publications You can
also search for this author inPubMed Google Scholar * Mathias Schneeweiss-Gleixner View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS Concept
of the study (P.H., B.S., T.R., C.Z., M.S-G.), data collection (P.H., M.R.-W., M.S., M.S-G.), statistical analysis (P.H., B.S., G.S., M.S-G.), drafting of the manuscript (P.H., B.S., L.B.,
T.R., M.S-G.,) and revision for important intellectual content as well as approval of the final manuscript (all authors). CORRESPONDING AUTHOR Correspondence to Mathias Schneeweiss-Gleixner.
ETHICS DECLARATIONS COMPETING INTERESTS The authors have nothing to disclose regarding the work under consideration for publication. Conflicts of interests outside the submitted work: B.S.
received travel support from AbbVie, Ipsen, and Gilead; G.S. received travel support from Gilead; T.R. received grant support from Abbvie, Boehringer-Ingelheim, Gilead, Intercept, MSD, Myr
Pharmaceuticals, Philips Healthcare, Pliant, Siemens and W. L Gore & Associates; speaking honoraria from Abbvie, Gilead, Intercept, Roche, MSD, W. L Gore & Associates;
consulting/advisory board fee from Abbvie, Astra Zeneca, Bayer, Boehringer-Ingelheim, Gilead, Intercept, MSD, Resolution Therapeutics, Siemens; and travel support from Abbvie,
Boehringer-Ingelheim, Gilead and Roche. ADDITIONAL INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional
affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License,
which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a
link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence,
unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory
regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Haselwanter, P., Scheiner, B., Balcar, L. _et al._ Use of the CytoSorb adsorber in
patients with acute-on-chronic liver failure. _Sci Rep_ 14, 11309 (2024). https://doi.org/10.1038/s41598-024-61658-3 Download citation * Received: 02 November 2023 * Accepted: 08 May 2024 *
Published: 17 May 2024 * DOI: https://doi.org/10.1038/s41598-024-61658-3 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link
Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative