A unique volatile signature distinguishes malaria infection from other conditions that cause similar symptoms
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Recent findings suggest that changes in human odors caused by malaria infection have significant potential as diagnostic biomarkers. However, uncertainty remains regarding the
specificity of such biomarkers, particularly in populations where many different pathological conditions may elicit similar symptoms. We explored the ability of volatile biomarkers to
predict malaria infection status in Kenyan schoolchildren exhibiting a range of malaria-like symptoms. Using genetic algorithm models to explore data from skin volatile collections, we were
able to identify malaria infection with 100% accuracy among children with fever and 75% accuracy among children with other symptoms. While we observed characteristic changes in volatile
patterns driven by symptomatology, our models also identified malaria-specific biomarkers with robust predictive capability even in the presence of other pathogens that elicit similar
symptoms. SIMILAR CONTENT BEING VIEWED BY OTHERS HUMAN SCENT AS A FIRST-LINE DEFENSE AGAINST DISEASE Article Open access 04 October 2023 IDENTIFICATION OF HUMAN SKIN MICROBIOME ODORANTS THAT
MANIPULATE MOSQUITO LANDING BEHAVIOR Article Open access 18 January 2024 BODY ODOR SAMPLES FROM INFANTS AND POST-PUBERTAL CHILDREN DIFFER IN THEIR VOLATILE PROFILES Article Open access 21
March 2024 INTRODUCTION The presence of disease can alter human odors, including volatile emissions from skin and breath. The potential diagnostic value of such changes in volatile chemistry
has long been recognized, and volatile-based diagnostics are being actively explored for a number of diseases, including several types of cancer1,2. However, a major challenge for the
development of volatile disease biomarkers is posed by the inherent variability of human volatile emissions, which are highly labile and can be influenced by a wide range of genetic,
physiological, and environmental factors3. In light of this variability, there is reason to speculate that volatile biomarkers might be of particular value in diagnosing diseases caused by
insect-borne pathogens, which frequently manipulate the odors of their hosts in ways that influence vector behavior and might therefore be highly conserved4,5,6. Indeed, a number of recent
studies on human malaria have identified characteristic changes in the volatile emissions from the skin and breath of infected individuals7,8,9,10,11,12. Yet, uncertainty remains about the
physiological bases of these volatile changes and the extent to which they are uniquely caused by malaria or products of pathological processes that might be shared with other disease
states. Addressing this uncertainty has important implications for understanding the diagnostic value of such biomarkers, particularly for use in human populations where numerous
pathological conditions are widespread and may give rise to similar symptomatology, as is often the case for malaria endemic regions. A number of previous studies have documented
malaria-induced changes in human skin7,8,9 and breath10,11,12 volatiles, as well as the volatile emissions of rodent malaria hosts13, while others have characterized the emissions of
_Plasmodium_ cells grown in vitro14,15,16. Effects of infection on host odors have also been reported to influence vector behavior, with several studies reporting increased mosquito
attraction to hosts harboring transmissible stages of _Plasmodium_ parasite13,17,18 and at least one showing enhanced attraction to host odor profiles in which individual compounds were
manipulated to mimic the relative up- or downregulation caused by infection13. Enhanced vector recruitment during the transmissible stage of infection is hypothesized to facilitate malaria
transmission19, suggesting that the pathogen may benefit from actively manipulating host volatiles20. To the extent that _Plasmodium_ parasites, or other vector-borne pathogens, alter host
odors in ways that consistently influence vector attraction, they may also generate unique patterns of effects on host volatile profiles—possibly tailored to the olfactory responses of
particular vector species—distinct from more general changes in volatile emissions that arise as mere byproducts of pathology. The presence of such unique signatures of infection might, in
turn, facilitate the identification of pathogen-specific biomarkers capable of reliably predicting infection status even in populations where numerous pathological conditions elicit similar
symptoms. The identification of such robust biomarkers is of particular interest for malaria, which frequently occurs in populations affected by numerous other diseases and ailments that
elicit similar symptoms, including fever, headaches, diarrhea, vomiting, etc., and might therefore plausibly be expected to have somewhat similar effects on underlying physiological
processes that also influence volatile emissions. In the case of malaria, disease progression often entails alternating asymptomatic and symptomatic phases that may recur indefinitely if not
treated. In a previous study, we reported differential up and down regulation of specific volatile organic compounds in both symptomatic and asymptomatic schoolchildren in Kenya7. Yet,
while these characteristic changes were highly predictive of malaria infection, the specific processes by which the presence of malaria parasites alter human volatiles remain almost entirely
unknown. One recent study reported that a malaria-derived isoprenoid increases the production of several monoterpenes and aldehydes in vitro21, but this does not account for the majority of
volatile alterations observed by our and other studies7,8,9,10,11,12 suggesting that the underlying mechanisms are likely to be complex. To explore the extent to which changes in the odors
of malaria infected humans are associated with the presence of symptoms, we analyzed the volatile profiles of symptomatic children, using volatile data previously collected from a large
field trial in Western Kenya7. Specifically, we compared the skin volatile profiles of symptomatic schoolchildren who tested positive for malaria to those of children presenting similar
(malaria-like) symptoms, but who tested negative for malaria. We used a genetic algorithm framework to predict malaria infection and identify volatile compounds associated with disease
status. Our goal was thus to discover which volatile changes might be specific to malaria, and which might be caused by infection with other illnesses or conditions. RESULTS AND DISCUSSION
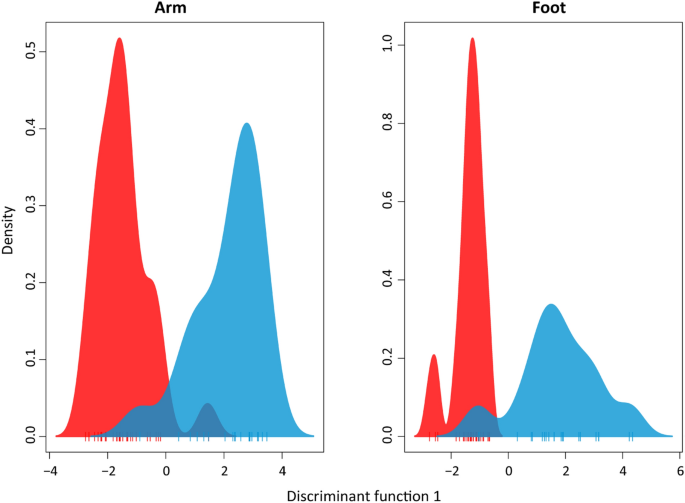
VOLATILE SIGNATURES DIFFERENTIATE SYMPTOMATIC CHILDREN WITH AND WITHOUT MALARIA INFECTION We first explored whether there was a clear signature of malaria infection among symptomatic
children. In addition to examining differences in the volatile profiles of malaria-infected and uninfected children presenting any symptom (i.e., all symptomatic children), we made similar
comparisons for non-exclusive subsets of children exhibiting the two most commonly observed symptoms in our dataset: fever and diarrhea. For each of these three symptom categories,
discriminant analysis of principal components (DAPC) revealed clear separation in the overall volatile composition between individuals with and without malaria infection (Fig. 1, S1), with a
permutational analysis of variance resulting in significant differences in both arms (pseudo_-F_1,48 = 2.96, _p_ = 0.022) and feet (pseudo_-F_1,49 = 2.91, _p_ = 0.003). These results
indicate that the effect of malaria infection on volatile profiles is apparent even when directly compared to other conditions that produce similar symptoms. We next used a genetic algorithm
predictive model trained to recognize malaria infection based on a subset of the data (70%) to predict malaria infection status in the remaining test set (30%). For children exhibiting any
symptom, this model was able to predict malaria status with 75% accuracy (Tables 1 and 2). Given that children included in this comparison likely exhibited highly variable physiological
states (i.e., different symptomatologies arising from the presence of different pathogens and various stages of disease progression) this level of predictive accuracy indicates that the
volatile signature of malaria infection is relatively robust. Our model exhibited similar accuracy (75%) in predicting malaria infection among the subset of symptomatic children with
diarrhea; for children with fever, however, the model predicted infections status with 100% accuracy (based using arm volatiles) (Tables 1 and 2). It also bears noting that only five
compounds were required to predict malaria among children with diarrhea, compared to greater numbers of compounds required for the other symptom categories. This is consistent with the
observation that few compounds show significant alteration with malaria infection status among children with diarrhea, compared to more extensive differences observed for children with fever
(Fig. 2). The higher level of predictive accuracy for children with fever may reflect distinct features of the pathology occurring in malaria-infected children. As _Plasmodium_ completes
its lifecycle within the host, fever is typically associated with the rupture of mature schizont cells and the release of merozoites that then reinvade red blood cells22. The resulting
intermittent cyclic fever may cause unique physiological effects compared to other ailments, and may also play a role in the downregulation of volatiles, including the compounds that drive
the predictive accuracy of our model (Fig. 2). Indeed, it is notable that malaria symptomatic children show decreased volatile production compared to both malaria-free febrile and
asymptomatic children (Fig. 2, S3), as fever might otherwise be presumed to cause a general upregulation of volatile emissions due to increased body temperature and sweating causing
increased evaporation of compounds from the skin. Of the eight volatile compounds selected by our model to predict malaria status from the arms of children with fever (Tables 1 and 2),
hexanal (C9), decane (C51) and octanal (C52), have been identified as predictors of malaria infection in several previous studies7,8,15,16. In the current study, these compounds were also
important predictors of infection status among children exhibiting any symptom, as well as among the subset of children with diarrhea. Hexanal and octanal are also known to serve as
host-location cues for mosquitoes, eliciting attraction or repellence depending on their concentration23,24. It is thus intriguing that the emission of these compounds appears to be
specifically influenced by the presence of malaria parasites. As we have previously speculated3,7, malaria-induced changes in volatile cues that enhance transmission probability via effects
on mosquito attraction19 might generate robust biomarkers of infection status. THE PRESENCE OF SYMPTOMS ALTERS VOLATILE PROFILES IN MALARIA-FREE CHILDREN To explore how the presence of
symptoms itself influences volatile emissions, we next used predictive models, similar to those described above, to examine differences between the volatile profiles of symptomatic and
asymptomatic children who tested negative for malaria infection. Here our models were able to predict the presence of symptoms with 60–80% accuracy across the three symptom categories
described above (fever, diarrhea, any symptom) and using either foot or arm volatiles (Table 3). Several compounds that were important predictors for the presence of symptoms in these models
were also important predictors of malaria infection status among symptomatic children in our previous analyses, including C8 (octane), C9 (hexanal) and C17 (4-hydroxy-4-methylpentan-2-one),
(Table 1). Comparing the volatile emissions of malaria-free children exhibiting any symptom to those without symptoms revealed significant downregulation of several compounds (Fig. 3), with
ethylbenzene (C20) showing the greatest downregulation in the presence of symptoms for both arm and foot volatiles. When focusing on individual symptoms, malaria-free children with diarrhea
showed no significant changes in compound levels compared to those without symptoms, whereas febrile children without malaria showed an upregulation of several foot volatile compounds (Fig.
3), in contrast to the downregulation of compounds seen in febrile children with malaria compared to malaria-free children without symptoms (Fig. S3). The only compound downregulated in
febrile children without malaria was C17 (4-hydroxy-4-methylpentan-2-one) (Fig. 3), which was further downregulated in malaria-infected children compared to febrile children without malaria
(Fig. 2). Among upregulated compounds in malaria-free febrile children, C9 (hexanal) was previously reported to be downregulated in malaria-infected vs uninfected children7. The overlap in
compounds identified as important predictors of malaria infection and of symptoms in malaria-free children (but with different patterns of up and down regulation) is intriguing and may
reflect the influences of different pathological conditions on the same underlying physiological processes. OVERLAP IN VOLATILE BIOMARKERS FOR MALARIA AND OTHER DISEASES As noted above, the
use of volatile diagnostics is under investigation or optimization for a number of diseases, including various types of cancer and pneumonia, and many studies have examined the volatiles in
breath that change dependent on disease status1,2,25. In the case of lung cancer, a large-scale trial for diagnostic detection using VOCs is currently underway26. For many other diseases,
however, significant challenges remain to be overcome prior to the implementation of large-scale trials, including the identification of a robust and reproducible set of candidate
biomarkers3, which can be complicated by the absence of standardized methods for volatile collection and analysis27. In the case of malaria, several previous studies have reported successful
prediction of infection status based on analysis of VOCs; however, there is considerable variation in the predictive compounds identified, likely owing to divergent methodologies across
studies. Two compounds, hexanal and nonanal, have consistently been found informative with respect to with malaria status, each reported in three separate studies from skin and breath
volatiles as well as in the prediction here of malaria status in symptomatic children (Table 4). Among compounds identified as predictors of malaria infection in the current study, hexanal
and nonanal, along. with decane and octanal, have previously been implicated as disease predictors in studies on other diseases in addition to malaria (Table 4). Hexanal, nonanal, octanal
and have been identified in the breath of lung and (along with decane) breast cancer patients, while nonanal has also been identified as a predictor of colorectal cancer and pneumonia2,25. A
further comparison of the key predictive compounds from this study and those identified for other diseases reveals several compounds that are specific to the differentiation of infection
status for malaria, including octane, 4-hydroxy-4-methylpentan-2-one, o-xylene and 2-ethylhexan-1-ol. This specificity may be related to the efficacy of these compounds in distinguishing
malaria infections form other conditions that give rise to similar symptoms; however, this remains speculative given that many of the other diseases for which volatile diagnostics have been
studied do not display similar symptoms. Finally, the recurrence of certain compounds such as hexanal and nonanal as predictors of multiple diseases may, again, reflect the influences of
different pathological conditions on the same underlying processes, but with disease-specific patterns of effects on volatile emissions that can give rise to distinct signatures. CONCLUSION
Volatile biomarkers hold significant promise for the development of non-invasive techniques for disease diagnosis1. However, extensive variation in human volatile emissions, including that
due to the presence of many different diseases and ailments within human populations, poses a significant challenge. While the robustness of malaria biomarkers across varying genetic and
environmental backgrounds still needs to be assessed in large-scale trials before they could enter clinical use, the current findings indicate that volatile biomarkers can identify malaria
infection even in the face of variation elicited by the presence of other symptomatic conditions. Our predictive models identified malaria cases with 100% accuracy for children with fever
and with 75% accuracy for other symptoms. We also identified specific compounds that are important predictors of malaria infection among symptomatic children, as well as compounds that are
more generally indicative of the presence of symptoms. These results suggest that, while some changes in human volatile profiles are broadly associated with the presence of symptomatic
disease, malaria elicits specific changes in key compounds that provide a unique signature of infection. METHODS ETHICS APPROVAL AND PARTICIPANT SELECTION This study was approved by The
Pennsylvania State University (IRB #41,529), ETH Zürich (EK2015-_N_-59), and the Kenya Medical Research Institute (SERU 391) and all experiments were performed in accordance with relevant
guidelines and regulations. Before sample collection, the study and consent form were explained to parents/guardians and their written informed consent was obtained. Participant exclusion
criteria included (1) receipt of antimalarial medication during the previous 2 wk; (2) chronic disease, such as HIV; (3) not signing (or having a parent sign) the consent form; and (4)
refusal of malaria treatment. SYMPTOM CATEGORIES Our analyses were performed on data derived from skin volatile samples (1 h collections from arms and feet) collected from students at 41
primary schools near Mbita Point, Kenya between 2013 and 20167. Symptoms were self-reported in an initial interview using a standardized questionnaire; symptoms indicative of malaria
included fever, abdominal pain, rash, diarrhea, vomiting and body aches. For our analysis, we sorted children into the categories (1) any symptom (2) fever, (3) diarrhea and (4)
asymptomatic. The any symptom category comprised children with fever, diarrhea, abdominal pain or vomiting; the fever and diarrhea categories were non-exclusive subsets of the any symptom
category. Abdominal pain and vomiting were not analyzed independently due to low numbers of children with these symptoms. Malaria infection status was initially assessed via rapid diagnostic
testing (SD Bioline), then confirmed by light microscopy and PCR. For the current study, children in the malaria infected category tested positive by both microscopy and PCR. The dataset
used for this study comprised volatile profiles for 114 children. Once categorized into symptoms for the below analyses, numbers of children in each category were as follows: malaria
infected children with any symptom = 29, fever = 18, diarrhea = 11. Malaria-free children with any symptom = 22, fever = 11, diarrhea = 9, asymptomatic = 16. VOLATILE DATA Arm and foot
volatiles were collected simultaneously for 1 h by enclosing the arm (from wrist to above the elbow) or foot (to below the knee) in a teflon bag, pushing filtered air through an entry port
(arm: 1.1 L/min, foot: 1.8 L/min) and pulling it through an exit port (arm: 0.8 L/min, foot: 1.1 L/min) where it was collected on an adsorbent HaySepQ filter. Compounds trapped on filters
were then eluted with 150ul dichloromethane and analyzed by GC–MS (Full methods: De Moraes 20187). STATISTICAL ANALYSES Discriminant Analysis of Principal Components (DAPC)41,42 was used to
compare the separation of healthy from malaria-infected individuals. These group differences were tested using a permutational analysis of variance (PERMANOVA) with the Euclidean similarity
on the scaled data43. We used a Genetic Algorithm (GA) to predict disease condition and to select one or more sets of compounds for each of the symptom subsets to be assessed as a potential
biomarker for malaria. Each subset was randomly split into 70% for model training and 30% for validation. Using the training set, each model was trained five times using a repeated tenfold
cross-validation. Genetic Algorithms are feature selection procedures that are conceptually based on the principle of evolution by natural selection44. They have been used as a promising
multivariate approach in the analysis of metabolomics datasets45,46. The algorithm works by evolving initial sets of variables (chromosomes) from a random population via cycles of
replication, recombination and mutation of the fittest chromosomes. The iterations were repeated for 100 generations, with a population size of 50 candidate solutions for each model and
crossover and mutation probabilities of 0.8 and 0.1, respectively. The performance of the fittest GA model was used to predict the samples in the validation set. To complement the predictive
models, a differential analysis between infection statuses was performed using the limma R package47. The GA models were formulated with the caret R package48. DATA AVAILABILITY All
relevant data reported in this paper have been deposited in ETH Zurich’s Research Collection, http://hdl.handle.net/20.500.11850/458605 (https://doi.org/10.3929/ethz-b-000458605). REFERENCES
* Buljubasic, F. & Buchbauer, G. The scent of human diseases: a review on specific volatile organic compounds as diagnostic biomarkers. _Flavour Fragr. J._ 30, 5–25.
https://doi.org/10.1002/ffj.3219 (2015). Article CAS Google Scholar * Oakley-Girvan, I. & Davis, S. W. Breath based volatile organic compounds in the detection of breast, lung, and
colorectal cancers: a systematic review. _Cancer Biomark_ 21, 29–39. https://doi.org/10.3233/cbm-170177 (2017). Article PubMed Google Scholar * Stanczyk, N. M., De Moraes, C. M. &
Mescher, M. C. Can we use human odors to diagnose malaria?. _Future Microbiol._ 14, 5–9. https://doi.org/10.2217/fmb-2018-0312 (2018). Article CAS PubMed PubMed Central Google Scholar *
Hughes, D. P., Brofeur, J., and Thomas, F. _Host Manipulation by Parasites_. (Oxford University Press, 2012). * Hurd, H. Manipulation of medically important insect vectors by their
parasites. _Annu. Rev. Entomol._ 48, 141–161. https://doi.org/10.1146/annurev.ento.48.091801.112722 (2003). Article CAS PubMed Google Scholar * Lefevre, T. & Thomas, F. Behind the
scene, something else is pulling the strings: emphasizing parasitic manipulation in vector-borne diseases. _Infect. Genet. Evolut. J. Mol. Epidemiol. Evolut. Genet. Infect. Dis._ 8, 504–519.
https://doi.org/10.1016/j.meegid.2007.05.008 (2008). Article Google Scholar * De Moraes, C. M. _et al._ Volatile biomarkers of symptomatic and asymptomatic malaria infection in humans.
_Proc Natl Acad Sci U S A_ (2018). * Robinson, A. _et al. Plasmodium_-associated changes in human odor attract mosquitoes. _Proc Natl Acad Sci U S A_ (2018). * de Boer, J. G. _et al._ Odours
of _Plasmodium falciparum-_infected participants influence mosquito-host interactions. _Sci. Rep._ 7, 9283. https://doi.org/10.1038/s41598-017-08978-9 (2017). Article ADS CAS PubMed
PubMed Central Google Scholar * Schaber, C. L. _et al._ Breathprinting reveals malaria-associated biomarkers and mosquito attractants. _J. Infect. Dis._
https://doi.org/10.1093/infdis/jiy1072 (2018). Article PubMed PubMed Central Google Scholar * Berna, A. Z. _et al._ Analysis of breath specimens for biomarkers of plasmodium falciparum
infection. _J. Infect. Dis._ 212, 1120–1128. https://doi.org/10.1093/infdis/jiv176 (2015). Article CAS PubMed PubMed Central Google Scholar * Berna, A. Z. _et al._ Diurnal variation in
expired breath volatiles in malaria-infected and healthy volunteers. _J. Breath Res._ 12, 046014. https://doi.org/10.1088/1752-7163/aadbbb (2018). Article ADS CAS PubMed PubMed Central
Google Scholar * De Moraes, C. M. _et al._ Malaria-induced changes in host odors enhance mosquito attraction. _Proc. Natl. Acad. Sci. USA_ 111, 11079–11084.
https://doi.org/10.1073/pnas.1405617111 (2014). Article ADS CAS PubMed PubMed Central Google Scholar * Kelly, M. _et al._ Malaria parasites produce volatile mosquito attractants.
_mBiol_ https://doi.org/10.1128/mBio.00235-15 (2015). Article Google Scholar * Correa, R., Coronado, L. M., Garrido, A. C., Durant-Archibold, A. A. & Spadafora, C. Volatile organic
compounds associated with _Plasmodium falciparum_ infection _in vitro_. _Parasit Vectors_ 10, 215. https://doi.org/10.1186/s13071-017-2157-x (2017). Article CAS PubMed PubMed Central
Google Scholar * Capuano, R. _et al._ Simultaneous Proton Transfer Reaction-Mass Spectrometry and electronic nose study of the volatile compounds released by _Plasmodium falciparum_
infected red blood cells in vitro. _Sci. Rep._ 9, 12360. https://doi.org/10.1038/s41598-019-48732-x (2019). Article ADS CAS PubMed PubMed Central Google Scholar * Lacroix, R.,
Mukabana, W. R., Gouagna, L. C. & Koella, J. C. Malaria infection increases attractiveness of humans to mosquitoes. _PLoS Biol._ 3, e298. https://doi.org/10.1371/journal.pbio.0030298
(2005). Article CAS PubMed PubMed Central Google Scholar * Busula, A. O. _et al._ Gametocytemia and attractiveness of _Plasmodium falciparum_–infected Kenyan children to _Anopheles
gambiae_ mosquitoes. _J. Infect. Dis._ https://doi.org/10.1093/infdis/jix214 (2017). Article PubMed Google Scholar * Cator, L. J., Lynch, P. A., Thomas, M. B. & Read, A. F.
Alterations in mosquito behaviour by malaria parasites: potential impact on force of infection. _Malar J._ 13, 11. https://doi.org/10.1186/1475-2875-13-164 (2014). Article Google Scholar *
Cator, L. J., Lynch, P. A., Read, A. F. & Thomas, M. B. Do malaria parasites manipulate mosquitoes?. _Trends Parasitol._ 28, 466–470. https://doi.org/10.1016/j.pt.2012.08.004 (2012).
Article PubMed PubMed Central Google Scholar * Emami, S. N. _et al._ A key malaria metabolite modulates vector blood seeking, feeding, and susceptibility to infection. _Science_ 355,
1076–1080. https://doi.org/10.1126/science.aah4563 (2017). Article ADS CAS PubMed Google Scholar * Crutcher, J. & Hoffman, S. in _Medical Microbiology_ (ed S. Baron) Ch. 83, (1996).
* Nyasembe, V. O., Teal, P. E., Mukabana, W. R., Tumlinson, J. H. & Torto, B. Behavioural response of the malaria vector _Anopheles gambiae_ to host plant volatiles and synthetic
blends. _Parasit Vectors_ 5, 234. https://doi.org/10.1186/1756-3305-5-234 (2012). Article PubMed PubMed Central Google Scholar * Takken, W., Knols, B. G., Takken, W., editors. _Olfaction
in vector-host interactions_. Vol. 2 (Wageningen Academic Publishers, 2010). * Pouline, M. O. _et al._ The potential role of exhaled breath analysis in the diagnostic process of pneumonia—a
systematic review. _J. Breath Res._ 12, 024001 (2018). Article Google Scholar * Lung Cancer Indication Detection. https://clinicaltrials.gov/ct2/show/NCT02612532 * Hanna, G. B., Boshier,
P. R., Markar, S. R. & Romano, A. Accuracy and methodologic challenges of volatile organic compound-based exhaled breath tests for cancer diagnosis: a systematic review and
meta-analysis. _JAMA Oncol._ 5, e182815–e182815. https://doi.org/10.1001/jamaoncol.2018.2815 (2019). Article PubMed Google Scholar * Fuchs, P., Loeseken, C., Schubert, J. K. &
Miekisch, W. Breath gas aldehydes as biomarkers of lung cancer. _Int. J. Cancer_ 126, 2663–2670. https://doi.org/10.1002/ijc.24970 (2010). Article CAS PubMed Google Scholar * Schumer, E.
M. _et al._ High sensitivity for lung cancer detection using analysis of exhaled carbonyl compounds. _J. Thorac. Cardiovasc. Surg._ 150, 1517–1524.
https://doi.org/10.1016/j.jtcvs.2015.08.092 (2015). Article CAS PubMed Google Scholar * Filipiak, W. _et al._ Release of volatile organic compounds (VOCs) from the lung cancer cell line
CALU-1 in vitro. _Cancer Cell Int._ 8, 17. https://doi.org/10.1186/1475-2867-8-17 (2008). Article CAS PubMed PubMed Central Google Scholar * Li, J. _et al._ Investigation of potential
breath biomarkers for the early diagnosis of breast cancer using gas chromatography–mass spectrometry. _Clin. Chim. Acta_ 436, 59–67. https://doi.org/10.1016/j.cca.2014.04.030 (2014).
Article ADS CAS PubMed Google Scholar * Phillips, M. _et al._ Volatile biomarkers in the breath of women with breast cancer. _J. Breath Res._ 4, 026003.
https://doi.org/10.1088/1752-7155/4/2/026003 (2010). Article ADS CAS PubMed Google Scholar * Altomare, D. F. _et al._ Exhaled volatile organic compounds identify patients with
colorectal cancer. _BJS (British Journal of Surgery)_ 100, 144–150. https://doi.org/10.1002/bjs.8942 (2013). Article CAS Google Scholar * Peng, G. _et al._ Detection of lung, breast,
colorectal, and prostate cancers from exhaled breath using a single array of nanosensors. _Br. J. Cancer_ 103, 542–551. https://doi.org/10.1038/sj.bjc.6605810 (2010). Article CAS PubMed
PubMed Central Google Scholar * Schmutzhard, J. _et al._ Pilot study: Volatile organic compounds as a diagnostic marker for head and neck tumors. _Head Neck_ 30, 743–749.
https://doi.org/10.1002/hed.20779 (2008). Article PubMed Google Scholar * Hakim, M. _et al._ Diagnosis of head-and-neck cancer from exhaled breath. _Br. J. Cancer_ 104, 1649–1655.
https://doi.org/10.1038/bjc.2011.128 (2011). Article CAS PubMed PubMed Central Google Scholar * Filipiak, W. _et al._ Molecular analysis of volatile metabolites released specifically by
_staphylococcus aureus_ and _pseudomonas aeruginosa_. _BMC Microbiol._ 12, 113. https://doi.org/10.1186/1471-2180-12-113 (2012). Article CAS PubMed PubMed Central Google Scholar *
Fowler, S. J., Basanta-Sanchez, M., Xu, Y., Goodacre, R. & Dark, P. M. Surveillance for lower airway pathogens in mechanically ventilated patients by metabolomic analysis of exhaled
breath: a case-control study. _Thorax_ 70, 320. https://doi.org/10.1136/thoraxjnl-2014-206273 (2015). Article PubMed Google Scholar * Schnabel, R. _et al._ Analysis of volatile organic
compounds in exhaled breath to diagnose ventilator-associated pneumonia. _Sci. Rep._ 5, 17179. https://doi.org/10.1038/srep17179 (2015). Article ADS CAS PubMed PubMed Central Google
Scholar * van Oort, P. _et al._ Exhaled breath metabolomics for the diagnosis of pneumonia in intubated and mechanically ventilated ICU–patients. _Europ. Respirat. J._ 50, OA4653.
https://doi.org/10.1183/1393003.congress-2017.OA4653 (2017). Article Google Scholar * Jombart, T. adegenet: a R package for the multivariate analysis of genetic markers. _Bioinformatics_
24, 1403–1405. https://doi.org/10.1093/bioinformatics/btn129 (2008). Article CAS Google Scholar * Jombart, T. & Ahmed, I. Adegenet 1.3–1: new tools for the analysis of genome-wide SNP
data. _Bioinformatics_ 27, 3070–3071. https://doi.org/10.1093/bioinformatics/btr521 (2011). Article CAS PubMed PubMed Central Google Scholar * Oksanen, J. _vegan: Community Ecology
package._ https://CRAN.R-project.org/package=vegan (2019). * Mitchell, M. _An introduction to genetic algorithms_. (MIT Press, 1996). * Goodacre, R. Making sense of the metabolome using
evolutionary computation: seeing the wood with the trees. _J. Exp. Bot._ 56, 245–254. https://doi.org/10.1093/jxb/eri043 (2004). Article CAS PubMed Google Scholar * Zou, W. &
Tolstikov, V. V. Pattern recognition and pathway analysis with genetic algorithms in mass spectrometry based metabolomics. _Algorithms_ https://doi.org/10.3390/a2020638 (2009). Article
Google Scholar * Ritchie, M. E. _et al._ limma powers differential expression analyses for RNA-sequencing and microarray studies. _Nucleic Acids Res_ 43, e47–e47.
https://doi.org/10.1093/nar/gkv007 (2015). Article CAS PubMed PubMed Central Google Scholar * Caret: Classification and regression training v. R package version 6.0–21 (CRAN: Wien,
Austria, 2014). Download references ACKNOWLEDGEMENTS We thank Caroline Wanjiku, James W. Sims, Heike S Betz, Andrew F. Read and Baldwyn Torto for the collection and analysis of the original
dataset and/or the facilitation of the project, as well as everyone involved with the project at the International Centre of Insect Physiology and Ecology’s Thomas Odhiambo campus in Mbita,
Kenya. Funding was provided by Bill and Melinda Gates Foundation Grant OPP1060415, and ETH Zürich. Predictive models were performed on the ETH Euler cluster. AUTHOR INFORMATION AUTHORS AND
AFFILIATIONS * Department of Environmental Systems Science, ETH Zürich, 8092, Zürich, Switzerland Hannier Pulido, Nina M. Stanczyk, Consuelo M. De Moraes & Mark C. Mescher Authors *
Hannier Pulido View author publications You can also search for this author inPubMed Google Scholar * Nina M. Stanczyk View author publications You can also search for this author inPubMed
Google Scholar * Consuelo M. De Moraes View author publications You can also search for this author inPubMed Google Scholar * Mark C. Mescher View author publications You can also search for
this author inPubMed Google Scholar CONTRIBUTIONS Conceived and designed the research: C.M.D.M., H.P., N.M.S., and M.C.M. Analyzed the data: H.P. Wrote the paper: N.M.S., H.P., C.M.D.M.,
and M.C.M. CORRESPONDING AUTHOR Correspondence to Mark C. Mescher. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER'S
NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION. RIGHTS AND
PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any
medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The
images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is
not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission
directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Pulido,
H., Stanczyk, N.M., De Moraes, C.M. _et al._ A unique volatile signature distinguishes malaria infection from other conditions that cause similar symptoms. _Sci Rep_ 11, 13928 (2021).
https://doi.org/10.1038/s41598-021-92962-x Download citation * Received: 04 February 2021 * Accepted: 06 May 2021 * Published: 06 July 2021 * DOI: https://doi.org/10.1038/s41598-021-92962-x
SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to
clipboard Provided by the Springer Nature SharedIt content-sharing initiative