Physical activity attenuates the associations of systemic immune-inflammation index with total and cause-specific mortality among middle-aged and older populations
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
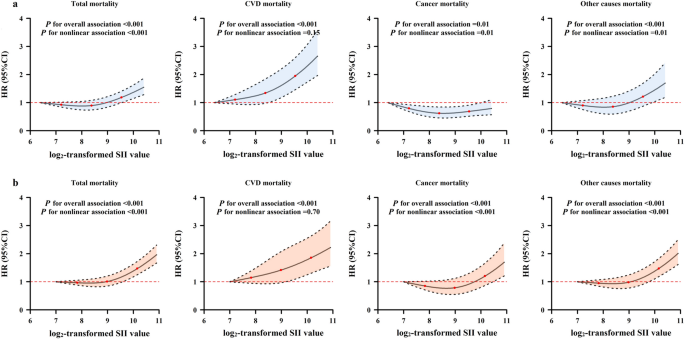
Systemic immune-inflammation index (SII) emerged as a biomarker of chronic inflammation and an independent prognostic factor for many cancers. We aimed to investigate the associations of SII
level with total and cause-specific mortality risks in the general populations, and the potential modification effects of lifestyle-related factors on the above associations. In this study,
we included 30,521 subjects from the Dongfeng-Tongji (DFTJ) cohort and 25,761 subjects from the National Health and Nutrition Examination Survey (NHANES) 1999–2014. Cox proportional hazards
regression models were used to estimate the associations of SII with mortality from all-cause, cardiovascular diseases (CVD), cancer and other causes. In the DFTJ cohort, compared to
subjects in the low SII subgroup, those within the middle and high SII subgroups had increased risks of total mortality [hazard ratio, HR (95% confidence interval, CI) = 1.12 (1.03–1.22) and
1.26 (1.16–1.36), respectively) and CVD mortality [HR (95%CI) = 1.36 (1.19–1.55) and 1.50 (1.32–1.71), respectively]; those within the high SII subgroup had a higher risk of other causes
mortality [HR (95%CI) = 1.28 (1.09–1.49)]. In the NHANES 1999–2014, subjects in the high SII subgroup had higher risks of total, CVD, cancer and other causes mortality [HR (95%CI) = 1.38
(1.27–1.49), 1.33 (1.11–1.59), 1.22 (1.04–1.45) and 1.47 (1.32–1.63), respectively]. For subjects with a high level of SII, physical activity could attenuate a separate 30% and 32% risk of
total and CVD mortality in the DFTJ cohort, and a separate 41% and 59% risk of total and CVD mortality in the NHANES 1999–2014. Our study suggested high SII level may increase total and CVD
mortality in the general populations and physical activity exerted a beneficial effect on the above associations.
Systemic chronic inflammation has been considered as an important risk factor for the development of multiple chronic diseases, including cardiovascular disease (CVD), cancer, and diabetes1,
which account for more than 50% of total deaths2. Since systemic chronic inflammation always developed in the absence of clinical manifestations, available and reliable systemic
inflammatory markers could help identify high-risk populations and develop therapeutic strategies, which were important for reducing the burden of chronic diseases. Many observational
studies have documented the associations of blood-based inflammatory markers with disease morbidity and mortality3,4,5. Elevated white blood cell (WBC) count was independently associated
with increased risks of incident CVD6, cancer4, and mortality7,8, while the roles of WBC subtypes and other blood cells such as platelets on mortality have been also investigated
individually9,10,11. As blood cells could interact with each other and then play essential roles in chronic inflammation-related diseases, the composite indices, such as
neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR), were considered to be potential prognostic factors for patients with CVD and cancer12,13,14, as well as markers
for predicting CVD incidence and mortality in the general populations15,16.
Recently, the systemic immune-inflammation index (SII), calculated based on the neutrophil, lymphocyte and platelet counts in peripheral blood, was put forward to reflect the balance of
systemic inflammation and immune status17. Previous studies implicated that an elevated level of SII was associated with poor prognosis of patients with certain malignancies, i.e.,
hepatocellular carcinoma17, colorectal cancer18, and pancreatic cancer19. Two cohort studies embedded in the Rotterdam Study found that high SII level was associated with the risks of solid
cancer and dementia20,21. One recent cohort study of 85,154 Chinese participants reported that high SII was associated with 24% increased total mortality risk22, but its association with
cause-specific mortality risk was not evaluated. Compelling evidence has suggested that unhealthy lifestyle factors, including smoking, alcohol drinking, physical inactivity, and being
overweight or obese, contributed to about 60% of deaths23, and were linked to chronic inflammation status1, which underscored the potential modification roles of these factors on the effects
of chronic inflammation.
In this study, we aimed to examine the associations of SII with total and cause-specific mortality in the general middle-aged and older populations of two large prospective cohort studies,
including the Dongfeng-Tongji (DFTJ) cohort and National Health and Nutrition Examination Survey (NHANES). We also explored the modification effects of the general characteristics [age, sex,
body mass index (BMI)] and common lifestyle factors (smoking, alcohol drinking and physical activity status) on the above associations.
Among the 30,521 participants in the DFTJ cohort [median (interquartile range, IQR) for age, 62.2 (56.2–68.0) years old], the median (IQR) of SII was 332.71 (236.91–467.61) × 109/L. There
were 3311 deaths occurring during a mean follow-up time of 8.2 years, including 1339 CVD deaths, 1081 cancer deaths, and 891 other causes deaths. Among the 25,761 participants in the NHANES
1999–2014 [median (IQR) for age, 54.5 (46.5–65.4) years old], the median (IQR) for SII was 505.14 (366.96–705.63) × 109/L. There were 4828 deaths occurring during a mean follow-up time of
7.6 years, including 1093 CVD deaths, 1032 cancer deaths, and 2703 other causes deaths. As shown in Table 1, compared to survivors, the deceased participants were more likely to be males,
elders, non-Hispanic Whites (only in the NHANES 1999–2014), smokers, less educated, physically inactive, and had a greater prevalence of hypertension, diabetes, CVD and cancer (all P