Circulating mir-141 and mir-375 are associated with treatment outcome in metastatic castration resistant prostate cancer
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Metastatic castration resistant prostate cancer (mCRPC) is associated with high mortality, where monitoring of disease activity is still a major clinical challenge. The role of
microRNAs (miRs) has been widely investigated in prostate cancer with both diagnostic and prognostic potential. The aim of this study was to investigate the relationship between circulating
miRs and treatment outcome in mCRPC patients. The relative expression of five miRs (miR-93-5p, -125b-1-5p, -141-3p, -221-3p, and miR-375-3p) was investigated in plasma samples from 84 mCRPC
patients; 40 patients were treated with docetaxel (DOC cohort) and 44 patients with abiraterone (ABI cohort). Blood was sampled at baseline before treatment start and at radiological
progression. The plasma levels of four miRs; miR-93-5p, -141-3p, -221-3p, and miR-375-3p decreased significantly after treatment initiation in patients receiving docetaxel, and for
miR-141-3p and miR-375-3p the level increased again at the time of radiological progression. In the patients treated with abiraterone, the plasma level of miR-221-3p likewise decreased
significantly after the first treatment cycle. High baseline levels of both miR-141-3p and miR-375-3p were significantly associated with a shorter time to radiological progression in both
cohorts. Additionally, high baseline levels of miR-141-3p and miR-221-3p were significantly associated with a shorter overall survival (OS) in the ABI cohort, while high levels of miR-141-3p
and miR-375-3p were significantly associated with shorter OS in the DOC cohort. Plasma levels of miR-141-3p and miR-375-3p may predict time to progression in mCRPC patients treated with
docetaxel or abiraterone. The clinical impact of these findings is dependent on validation in larger cohorts. SIMILAR CONTENT BEING VIEWED BY OTHERS VALIDATION OF THE FOUR-MIRNA BIOMARKER
PANEL _MICAP_ FOR PREDICTION OF LONG-TERM PROSTATE CANCER OUTCOME Article Open access 01 July 2020 MICRORNA-375 IS A THERAPEUTIC TARGET FOR CASTRATION-RESISTANT PROSTATE CANCER THROUGH THE
PTPN4/STAT3 AXIS Article Open access 30 August 2022 MICRORNAS AS BIOMARKERS FOR PROSTATE CANCER PROGNOSIS: A SYSTEMATIC REVIEW AND A SYSTEMATIC REANALYSIS OF PUBLIC DATA Article Open access
12 January 2022 INTRODUCTION Metastatic castration resistant prostate cancer (mCRPC) is considered the most aggressive phase of the disease with survival rarely exceeding three years1.
Virtually all advanced prostate cancer (PCa) patients will develop mCRPC within a period of about 24 months2. Although the management of mCRPC has improved considerably since 2004 by the
introduction of various agents providing improved overall survival (OS) and progression free survival (PFS), none of the options are curative3. Docetaxel and abiraterone were among the first
agents to be approved in the mCRPC setting, however with a modest increase of OS4,5. Both agents, however, recently demonstrated a marked OS improvement in de novo metastatic PCa6,7. One of
the most important challenges in daily practice is the monitoring of disease activity in mCRPC patients. Prostate-specific antigen (PSA) alone is not a reliable biomarker in this stage8, as
visceral metastases have been observed in patients without rising PSA9. A few prognostic models for mCRPC patients have been proposed over the last few years, but the efforts are still in
their infancy10,11. Hence, treatment optimization at this stage of the disease may be challenged due to lack of validated non-invasive prognostic biomarkers. MicroRNAs (miRs) are non-coding
single-stranded evolutionarily conserved RNA molecules, about 22 nucleotides in length, that regulate gene expression both at the transcriptional and post transcriptional level12. So far,
more than 2600 mature human miRs have been identified13,14, many with essential roles in physiological and pathological cellular processes, including cancer development and progression15.
For different reasons, miRs have been quite attractive as alternative biomarkers, especially in PCa. Firstly, miRs have shown to be dysregulated in PCa and may be able to distinguish between
stages of the disease16. Secondly, they can be extracted from different body fluids, including plasma17. Lastly, miRs remain stable under various storage conditions18. The purpose of this
study was to investigate the relationship between circulating miRs and treatment outcome in patients with mCRPC treated with either docetaxel or abiraterone. RESULTS PATIENT CHARACTERISTICS
We recruited 40 patients to the DOC cohort and 44 patients in the ABI cohort. The median PSA level at the stage of mCRPC in the DOC cohort was significantly higher than in the ABI cohort.
Furthermore, the distribution of metastases differed significantly between the two cohorts. In the DOC cohort the time until mCRPC development was significantly shorter than in the ABI
cohort. Due to an earlier inclusion start in the DOC cohort, the follow-up period was significantly longer compared to the ABI cohort. The clinicopathological characteristics of all patients
are presented in Table 1. The baseline plasma levels of three microRNAs, i.e. miR-93-5p, miR-125b-1-5p and miR-221-3p, differed significantly between the two cohorts (Supplementary Table
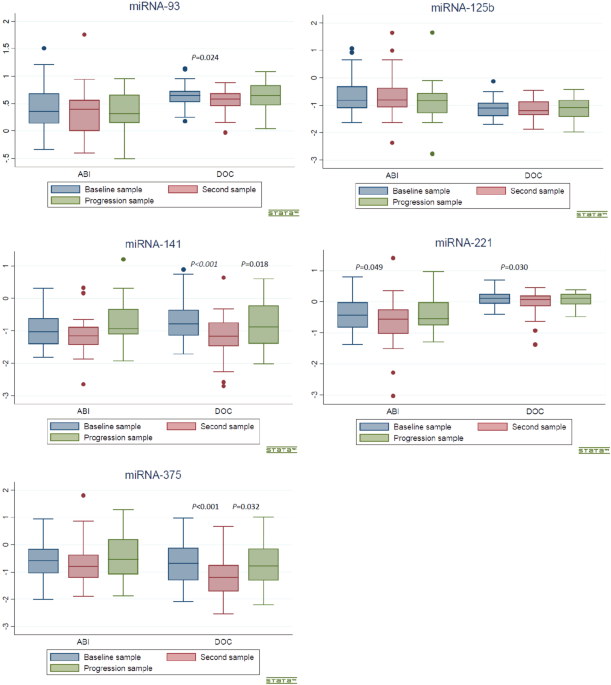
S1). CHANGES IN CIRCULATING MIRS DURING TREATMENT After the first treatment cycle, the plasma levels of miR-221-3p decreased significantly in both the ABI and the DOC cohort (z = −1.962, _p_
= 0.049 and z = −2.168, _p_ = 0.030, respectively). Furthermore, in the DOC cohort the plasma levels of miR-93-5p, −141−3p, and miR−375–3p were significantly lower than the baseline levels
(z = −2.255, _p_ = 0.024; z = −3.870, _p_ = <0.001, and z = −4.148, _p_ = <0.001 respectively) (Table 2). At progression circulating miR-141-3p and miR-375-3p increased significantly
compared to the plasma levels after the first docetaxel treatment (z = 2.368, _p_ = 0.018 and z = 2.146, _p_ = 0.032, respectively). In the ABI cohort, the plasma level of miR-125b-1-5p at
progression tended to be significantly lower compared to the level after the first abiraterone treatment (z = −1.938, _p_ = 0.053) (Table 3). The levels of circulating miRs at baseline,
after one treatment cycle, and at radiological progression in both cohorts are illustrated by boxplots in Fig. 1. ASSOCIATION BETWEEN CIRCULATING MIRS AND TREATMENT OUTCOME High plasma
baseline levels of miR-141-3p and miR-375-3p were significantly associated with a shorter time to rPFS both in the ABI cohort (HR = 3.18, _p_ = <0.01; HR = 2.17, _p_ = 0.02,
respectively), and in the DOC cohort (HR = 2.56, _p_ = <0.01; HR = 2.44, _p_ = <0.01, respectively). In the ABI cohort high levels of miR-141-3p and miR-221-3p at baseline were
significantly associated with shorter OS (HR = 3.20, _p_ = 0.02, HR = 2.36, _p_ = 0.04, respectively). In the DOC cohort, high levels of miR-141-3p and miR-375-3p were significantly
associated with shorter OS (HR = 1.77, _p_ = 0.02; HR = 2.48, _p_ = <0.01, respectively) (Table 4). The association of baseline circulating miR-141-3p and miR-375-3p with rPFS is further
illustrated by Kaplan-Meier curves in Fig. 2. Full OS and rPFS data are provided in Supplementary Table S2, Figs. S1 and S2. DISCUSSION In the present study we demonstrate the association of
miR-141-3p and miR-375-3p with treatment outcome in mCRPC patients treated with either docetaxel or abiraterone. The level of both miRs decreased after treatment initiation and increased
again at progression. Circulating levels of miRs in mCRPC patients has been assessed in previous studies19,20,21. Plasma levels of both miR-141-3p and miR-375-3p demonstrated a relative high
specificity to distinguish local PCa from mCRPC19. Cheng _et al_.20 and Nguyen _et al_.21 observed a higher level of a panel of miRs (including miR-141-3p and miR-375-3p) in blood samples
pooled from patients diagnosed with mCRPC compared with an age-matched control group or low risk PCa patients, respectively. These results were furthermore validated in serum samples
collected from another independent cohort (21 mCRPC patients versus 20 healthy controls)20. The decreased plasma level of most of the investigated miRs in this study after introduction of
both docetaxel and abiraterone and the subsequent increase at radiological progression argue for an oncogenic role in PCa. These changes of circulating miRs as a treatment response has also
been reported in previous studies22,23,24. Lin _et al_.23 documented a significant association between changes in circulating levels of six miRs (three of them are members of miR-200 family,
namely miR-200b, -200c, and miR-429) and PSA response in mCRPC patients receiving docetaxel. However these results couldn’t be validated in a larger independent mCRPC cohort receiving
docetaxel in a phase 2 study performed by the same group24. Dispite a small population size (10 mCRPC patients), a predictive value of high serum miR-21 (4/10) were proposed for those who
were resistant to docetaxel treatment22. Among the upregulated miRs, miR-141and miR-375 were among the first circulating miRs investigated in PCa25,26. The function of both miR-141-3p and
miR-375-3p in CRPC pathogenesis may be similar and interactive. SEC. 23A is a target for both miR-375-3p and the miR-200 family (miR-141-3p is one of its members), where both miRs promoted
epithelial-to-mesenchymal transition (MET) in PCa27,28,29,30. While miR-375-3p regulates MET through YAP1, and its expression shown to be suppressed by ZEB1, miR-200 family members
downregulates ZEB1 expression, and therefore may contribute to upregulation of miR-375-3p28. Interestingly, the plasma levels of miR-125b-1-5p showed a tendency towards a decrease at
progression in the ABI cohort. This observation is in concordance with our previous work31, in which the plasma level of miR-125b-1-5p decreased six months after diagnosis of local prostate
cancer in a cohort of patients undergoing active surveillance. Although some studies have indicated an oncogenic role25,32, the exact function of miR-125b-1-5p in cancer progression is not
fully understood33. In the current study a higher baseline plasma level of miR-141-3p and miR-375-3p was significantly associated with shorter rPFS in mCRPC patients regardless of treatment.
While higher levels of miR-141-3p and miR-221-3p at baseline were associated with poorer OS in patients receiving abiraterone, an unfavourable prognosis in the DOC cohort was characterised
by high levels of miR-141-3p and miR-375-3p. Previous studies have demonstrated a prognostic value of miR-375-3p in the mCRPC setting21,24,34,35,36. Nguyen _et al_. has proposed a prognostic
value of both miR-141-3p and miR-375-3p with a trend of increasing plasma levels at disease progression from low risk PCa, high risk PCa and to mCRPC21. The same results were observed by
Bryant _et al_. exploring both miRs in two different independent cohorts. In both plasma and sera (microvesicles and exosomes) circulating levels of both miR-141-3p and miR-375-3p were
significantly correlated with metastatic PCa35. Additionally, in a screening cohort of 23 mCRPC patients, high plasma level of miR-375 was associated with poor OS. This observation was
validated in a follow-up cohort of another independent 100 mCRPC patients34.Futhermore, in a phase 2 study Lin _et al_. has observed associations between baseline levels of circulating
miR-375 and poor outcome24. In contrast to our findings, Kneitz _et al_.36 found that lower expression of miR-221-3p was associated with a higher rate of cancer related death. A possible
explanation for this difference could be the patient population and material used. Kneitz _et al_. investigated the expression of miRs in paraffin-embedded prostate cancer tissue from
localized PCa patients treated with radical prostatectomy. Many studies have demonstrated a suppressed expression of miR-221-3p in PCa37,38. Additionally, miR-221-3p is strongly associated
with aggressiveness of PCa and may serve as a potential prognostic biomarker in patients diagnosed with high-risk PCa39. Interestingly, other cancers such as lung, bladder, thyroid, breast,
liver, or pancreas showed an overexpression of miR-221-3p where the tumor suppressor p57kip2, c-kit, PTEN TIMP3, and PUMA have been reported to be miR-221 targets40,41,42,43. We observed a
relative more missed/over 37 Ct values in plasma samples after treatment initiation compared with baseline samples. This was more obvious for miR-141-3p, miR-221-3p and miR-375-3p. Such
observations were not unexpected, because treatment with either abiraterone or docetaxel would probably influence the amount of detectable oncogenic miRs as it was hypothesized in our study.
However, there was a decrease of these missed/over 37 Ct values at time of prostate cancer progression (due to increase in plasma level of these two oncogenic miRs), especially for both
miR-141-3p and miR-221-3p in ABI cohort. This could be explained by the different mechanism of both abiraterone and docetaxel. Abiraterone is considered as a new agents to modulate androgen
production, and regulating effect of both miR-141-3p and miR-221-3p on androgen receptor transcription has been documented44,45. It is worth noting that the mCRPC patients in the DOC cohort
had a more aggressive disease compared to the patients in the ABI cohort. This could be observed from the relatively high PSA level and higher incidence of visceral metastases in the DOC
cohort. The site of metastases has been suggested to correlate with prognosis, visceral metastases having the worst outcome46. The serial blood sample collection from two different cohorts
and the long follow-up period are considered strengths in the present study. The solidity of our findings has also been emphasized despite the heterogeneity of the patients and different
treatments in the cohorts. However, the small size of the DOC and the ABI cohorts could be considered a limitation, therefore external validation of these results is required as the purpose
of the current study was explorative and hypothesis generating. Larger cohorts are required to validate the above results. Additionally, investigation of the treatment effect of other
options such as cabazitaxel, enzalutamide or radium-223 could explore more about the significance of miRs in the mCRPC setting. Heterogeneity of mCRPC is a well-established clinical
challenge, and patient stratification based on metastatic tissue biopsies is not routinely applicable. In a time with many treatment options robust, non-invasive biomarkers guiding the
choice of the most appropriate treatment are warranted. CONCLUSION The plasma level of miR-141-3p and miR-375-3p in mCRPC patients decreases after treatment initiation of abiraterone as well
as docetaxel and increases again at the time of radiological progression. Both miRs demonstrated a significant relationship with treatment outcome and overall survival in both cohorts.
These results add to the clinical significance of miRs as alternative and non-invasive biomarkers in prostate cancer. Validation of our results in larger cohorts will help clarify the
clinical impact. MATERIALS AND METHODS PATIENTS This study was based on plasma samples prospectively collected from two cohorts of mCRPCa patients; the docetaxel (DOC) cohort, and the
abiraterone (ABI) cohort. The patients were enrolled at the Department of Oncology, Vejle Hospital, Denmark. In total, 84 mCRPCa patients were recruited; 40 patients in the DOC cohort from
June 2012 to August 2017 and 44 in the ABI cohort from April 2014 to March 2017. All participants provided informed written consent. Seven patients in the ABI cohort had a synchronic cancer
(two with colon cancer, one with lung cancer, one with testicular and liver cancer, one with malignant melanoma, one with urothelial cancer, and with thyroid cancer). Four patients in the
DOC cohort had a synchronic cancer (two patients with adenocarcinomas of the skin, one with Hodgkin’s lymphoma and one patient with renal cancer). Detailed clinicopathological data for all
patients in both cohorts is provided in Supplementary Table S3. The study was approved by The Regional Committees on Health Research Ethics for Southern Denmark (S-20110102 and S-20130099
for DOC and ABI protocol, respectively) and The Danish Data Protection Agency according to Danish law. The Danish Registry of Tissue Utilization was screened prior to study initiation. All
methods were performed in accordance with the relevant guidelines and regulations. Patients in the DOC cohort were treated with a maximum of eight cycles of docetaxel, 75 mg/m2 every three
weeks, unless radiologic progression or unacceptable toxicity occurred earlier. The ABI cohort was treated with abiraterone tablets 1000 mg + prednisone tablets 10 mg daily until
radiological progression or unacceptable toxicity. All patients were evaluated clinically and biochemically before every treatment cycle (every 3 weeks in the DOC cohort and every 4 weeks in
the ABI cohort), and radiologically by bone scan as well as chest and abdomen computed tomography (CT) every 3 cycles. For the analysis of OS a clinical cut-off date was set for September
27, 2018. The follow-up period was defined as the time from inclusion to the clinical cut-off date. Time to mCRPC was calculated from the date of PCa diagnosis to the date of verified mCRPC.
The definition of mCRPC was based on the European Association of Urology (EAU) guidelines47. Overall survival was defined as the time from treatment start to death from any cause and
radiologic progression free survival (rPFS) as the time from treatment start to radiological progression or death, whichever occured first. Radiological progression was assessed on the basis
of the Prostate Cancer Working Group 3 (PCWG3) criteria48, while soft-tissue disease progression was evaluated by modified Response Evaluation Criteria In Solid Tumors (RECIST) 1.149.
Progression of bone metastases was evaluated by bone scans with two or more new lesions indicating progression. At clinical cut-off date there were 19 patients in the ABI cohort and 24
patients in the DOC cohort who had radiological progression. BLOOD COLLECTION AND STORAGE Three plasma samples from each patient in both cohorts were chosen for further analysis; at
baseline, just after treatment initiation, and at radiological progression. Venous blood samples were collected from all patients in both cohorts at baseline and radiological progression.
Sampling was performed by skilled phlebotomists using a minimum of venous stasis to prevent hemolysis. Whole blood was collected into 9 mL ethylenediaminetetraacetic acid (EDTA) containing
tubes (Becton-Dickinson, Franklin Lakes, NJ, USA). The samples were centrifuged at 2500 g for 10 min. and carefully transferred into cryo-tubes leaving approximately 1 mL of plasma on top of
the buffy coat and then stored at −80 °C. A second step of centrifugation at 3000 g for 30 min. was carried out after storage but prior to miR purification. To reduce the risk of hemolysis
and release of miRs from other intravascular cell compartments blood was centrifuged within 30 minutes after sampling. Also, all samples were evaluated for hemolysis by A414 measure, and
approx. 92% of all values were ≤log (abs) = 0.2, which corresponds to less than 1% hemolysis. There were 21 samples (8%) above 0.2 and below 0.5. Evaluation of them did not show any trends
towards neither higher nor lower cycle threshold (Ct) values and therefore, they were not excluded. Only one sample (0.4%) had a relatively high hemolysis index (≥0.5) and this sample was
excluded from further data analysis. SELECTED MIR TARGETS In the present study a panel of five miRs was selected; miR-93-5p, -125b-1-5p, -141-3p, -221-3p, and miR-375-3p. This choice was
based on results from our previous work31,50,51 and a comprehensive review of the literature. RNA PREPARATION AND QPCR PLASMA SAMPLES miR purification of plasma samples was performed using
the Maxwell RSC miR Tissue Kit (AS1460) verified for plasma use (Scientific Style and Format, 7th edition, 2006). 200 µl plasma was mixed with 200 µl chilled 1-Thioglycerol/Homogenization
solution and 200 µl lysis solution. After incubation for 10 min. the sample mix was loaded into the Maxwell RSC Instrument. Elution was done using 60 µl elution buffer. REVERSE TRANSCRIPTION
AND QPCR All preparations were done using the standard protocol from the QIAGEN miRCURY™ LNA™ miR PCR System. Universal cDNA synthesis was performed in duplicate using miRCURY™ LNA™ miR RT
Kit (QIAGEN Cat. No. 339340) in 10ul reaction volume using 2 ul purified RNA in each reaction. cDNA was then diluted 1:40 in water for qPCR performed in 10 ul reaction volume using miRCURY™
LNA miR Custom PCR panels (Cat. No 339330) and miRCURY™ SYBR Green Master Mix (Cat. No. 339345) supplied by QIAGEN.In brief, we used a plate setup supplied by QIAGEN with all primers as
dried pellets in individual plate wells. After universal RT the individual miR’s are detected using LNA-enhanced miR species specific primers and SYBR green. We used Roche Lightcycler 96®.
USE OF CONTROLS Each patient sample was added several exogenous controls. First, before purification, UniSp2/4/6 template mix was spiked in to assess RNA purification efficiency. Next,
Cel-miR-39 template was spiked in before RT reaction to assess the level of inhibition in this reaction. Plate-to-plate variation was eliminated using 6× UniSp3 IPC template on each plate
(each plate was commercially supplied with both template and primers for UniSp3). UniSp4 and Cel-miR-39 added templates were then amplified in qPCR using target specific LNA primers. This
control setup was part of the miRCURY™ LNA™ miR PCR System and we followed the general guideline for this protocol regarding volumes and concentrations, ie. we added 0,02 fmol UniSp4 to each
purification reaction and 0,001 fmol Cel-miR-39 to each RT reaction. In addition, on each plate we tested all miR assays using “no template controls”. For normalization of miR levels, we
used miR-17-5p and miR-191-5p, as these species had previously been established as suitable endogenous controls51. INITIAL DATA ANALYSIS Each Ct value presented in this work is a mean Ct
calculated from two qPCR results based on two individual RT reactions using RNA from the same purification. All Plate-to-plate variation controls showed very little variation (Ct mean of
20,31 and varied between plates under 0,2 Ct) for all 71 plates. The added Cel-miR-39 template was detected in all sample preparations and resulted in a mean Ct of 25.8 and a variance of
1.07 Ct. The added UniSp4 template was detected in 264 of 273 samples with a mean Ct of 31.8 and a variance of 5.4 Ct, which we conclude is more than optimal, but explainable by the sub
optimal initial sample preparation. A dataset with all raw Ct values is provided in Supplementary Table S4. STATISTICAL ANALYSIS Data are presented as means of two technical replicates per
plasma sample from each patient. Based on the Ct value, the fold change of plasma miR was calculated according to the following formula: $$\Delta
{\rm{Ct}}={\rm{mean}}\,{\rm{Ct}}\,{\rm{value}}\,{\rm{of}}\,{\rm{target}}\,{\rm{miR}}-{\rm{mean}}\,{\rm{Ct}}\,{\rm{value}}\,{\rm{of}}\,{\rm{miR}}-17\,{\rm{and}}\,{\rm{miR}}-191.$$ Results
were linearized using 2−(ΔCT), which was subsequently applied in the statistical analysis. Samples with missed Ct values were dismissed. Likewise, Ct values above 37 measurements were
excluded; however, this was not applied on samples collected after the first treatment cycle, as a decrease in miR plasma levels was expected (Supplementary Table S5a,b). Wilcoxon rank sum
test was applied for assessment of the difference in baseline levels between the DOC and ABI cohorts. The Wilcoxon signed rank sum test was used to analyse the difference between plasma miR
levels at baseline, after one treatment cycle, and at progression in both the ABI and the DOC cohort and illustrated by boxplots. The association between miR levels and OS and rPFS was
assessed using simple Cox regression (univariate analysis) and Kaplan-Meier survival curves. Proportional hazard assumption for the Cox regression model was assessed by Schoenfeldt
residuals, and log-Rank was used to test for differences between Kaplan-Meier survival curves. All analyses were performed in Stata version 15.1 (StataCorp LLC, TX, USA), and
correlations/differences were considered statistically significant with a p-value was < 0.05. REFERENCES * Mostaghel, E. A., Montgomery, B. & Nelson, P. S. Castration-resistant
prostate cancer: Targeting androgen metabolic pathways in recurrent disease. _Urologic Oncology: Seminars and Original Investigations_ 27, 251–257 (2009). Article CAS PubMed Google
Scholar * Seruga, B., Ocana, A. & Tannock, I. F. Drug resistance in metastatic castration-resistant prostate cancer. _Nature Reviews Clinical Oncology_ 8, 12–23 (2011). Article CAS
PubMed Google Scholar * Christenson, E. S. & Antonarakis, E. S. PARP inhibitors for homologous recombination-deficient prostate cancer. _Expert Opin. Emerg. Drugs_ 23, 123–133 (2018).
Article PubMed PubMed Central Google Scholar * Berthold, D. R. _et al_. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer: Updated survival in the
TAX 327 study. _J. Clin. Oncol._ 26, 242–245 (2008). Article CAS PubMed Google Scholar * Fizazi, K. _et al_. Abiraterone acetate for treatment of metastatic castration-resistant prostate
cancer: Final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. _Lancet Oncol._ 13, 983–992 (2012). Article CAS PubMed Google
Scholar * James, N. D. _et al_. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): Survival results from an adaptive,
multiarm, multistage, platform randomised controlled trial. _Lancet_ 387, 1163–1177 (2016). Article CAS PubMed PubMed Central Google Scholar * Fizazi, K. _et al_. Abiraterone plus
Prednisone in Metastatic, Castration-Sensitive Prostate Cancer. _N. Engl. J. Med._ 377, 352–360 (2017). Article CAS PubMed Google Scholar * Payne, H. & Cornford, P. Prostate-specific
antigen: An evolving role in diagnosis, monitoring, and treatment evaluation in prostate cancer. _Urologic Oncology: Seminars and Original Investigations_ 29, 593–601 (2011). Article
PubMed Google Scholar * Pezaro, C. J. _et al_. Visceral disease in castration-resistant prostate cancer. _Eur. Urol._ 65, 270–273 (2014). Article CAS PubMed Google Scholar * Armstrong,
A. J. _et al_. The development of risk groups in men with metastatic castration-resistant prostate cancer based on risk factors for PSA decline and survival. _Eur. J. Cancer_ 46, 517–525
(2010). Article CAS PubMed Google Scholar * Halabi, S. _et al_. Updated prognostic model for predicting overall survival in first-line chemotherapy for patients with metastatic
castration-resistant prostate cancer. _J. Clin. Oncol._ 32, 671–677 (2014). Article PubMed PubMed Central Google Scholar * Catalanotto, C., Cogoni, C. & Zardo, G. MicroRNA in control
of gene expression: An overview of nuclear functions. _Int_. _J_. _Mol_. _Sci_. 17 (2016). * miRBase. Available at, http://www.mirbase.org (Accessed: 18th December 2018). * Kozomara, A.,
Birgaoanu, M. & Griffiths-Jones, S. MiRBase: From microRNA sequences to function. _Nucleic Acids Res._ 47, D155–D162 (2019). Article CAS PubMed Google Scholar * Croce, C. M. Causes
and consequences of microRNA dysregulation in cancer. _Nat. Rev. Genet._ 10, 704–714 (2009). Article CAS PubMed PubMed Central Google Scholar * Chun-Jiao, S. _et al_. The potential of
microRNAs as human prostate cancer biomarkers: A meta-analysis of related studies. _J_. _Cell_. _Biochem_., https://doi.org/10.1002/jcb.26445 (2017). Article PubMed PubMed Central CAS
Google Scholar * Weber, J. A. _et al_. The microRNA spectrum in 12 body fluids. _Clin. Chem._ 56, 1733–1741 (2010). Article CAS PubMed PubMed Central Google Scholar * Egidi, M. G. _et
al_. Circulating microRNAs and Kallikreins before and after radical prostatectomy: Are they really prostate cancer markers? _Biomed Res. Int._ 2013, 241780 (2013). Article PubMed PubMed
Central CAS Google Scholar * Watahiki, Y. _et al_. Plasma miRNAs as biomarkers to identify patients with castration-resistant metastatic prostate cancer. _Int. J. Mol. Sci._ 14, 7757–7770
(2013). Article PubMed PubMed Central CAS Google Scholar * Cheng, H. H. _et al_. Circulating microRNA Profiling Identifies a Subset of Metastatic Prostate Cancer Patients with Evidence
of Cancer-Associated Hypoxia. _PLoS One_ 8, e69239 (2013). Article ADS CAS PubMed PubMed Central Google Scholar * Nguyen, H. C. N. _et al_. Expression differences of circulating
microRNAs in metastatic castration resistant prostate cancer and low-risk, localized prostate cancer. _Prostate_ 73, 346–354 (2013). Article CAS PubMed Google Scholar * Zhang, H. L. _et
al_. Serum miRNA-21: Elevated levels in patients with metastatic hormone-refractory prostate cancer and potential predictive factor for the efficacy of docetaxel-based chemotherapy.
_Prostate_ 71, 326–331 (2011). Article CAS PubMed Google Scholar * Lin, H. M. _et al_. Circulating microRNAs are associated with docetaxel chemotherapy outcome in castration-resistant
prostate cancer. _Br. J. Cancer_ 110, 2462–2471 (2014). Article CAS PubMed PubMed Central Google Scholar * Lin, H. M. _et al_. Phase 2 study of circulating microRNA biomarkers in
castration-resistant prostate cancer. _Br. J. Cancer_ 116, 1002–1011 (2017). Article CAS PubMed PubMed Central Google Scholar * Mitchell, P. S. _et al_. Circulating microRNAs as stable
blood-based markers for cancer detection. _Proc. Natl. Acad. Sci._ 105, 10513–10518 (2008). Article ADS CAS PubMed PubMed Central Google Scholar * Brase, J. C., Wuttig, D., Kuner, R.
& Sültmann, H. Serum microRNAs as non-invasive biomarkers for cancer. _Molecular Cancer_ 9, 306 (2010). Article CAS PubMed PubMed Central Google Scholar * Szczyrba, J. _et al_.
Downregulation of Sec. 23A Protein by miRNA-375 in Prostate Carcinoma. _Mol. Cancer Res._ 9, 791–800 (2011). Article CAS PubMed Google Scholar * Selth, L. A. _et al_. A ZEB1-miR-375-YAP1
pathway regulates epithelial plasticity in prostate cancer. _Oncogene_ 36, 24–34 (2017). Article CAS PubMed Google Scholar * Griffiths-Jones, S., Saini, H. K., Van Dongen, S. &
Enright, A. J. miRBase: Tools for microRNA genomics. _Nucleic Acids Res._ 36, D154–8 (2008). Article CAS PubMed Google Scholar * Gregory, P. A. _et al_. The miR-200 family and miR-205
regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. _Nat. Cell Biol._ 10, 593–601 (2008). Article CAS PubMed Google Scholar * Zedan, A., Hansen, T., Assenholt, J.,
Madsen, J. & Osther, P. S. Circulating miRNAs in localized/locally advanced prostate cancer patients after radical prostatectomy and radiotherapy. _Prostate_ pros. 23748,
https://doi.org/10.1002/pros.23748 (2018). * Singh, P. K. _et al_. Serum microRNA expression patterns that predict early treatment failure in prostate cancer patients. _Oncotarget_ 5, 824–40
(2014). PubMed PubMed Central Google Scholar * Banzhaf-Strathmann, J. & Edbauer, D. Good guy or bad guy: The opposing roles of microRNA 125b in cancer. _Cell Commun. Signal._ 12,
1–13 (2014). Article CAS Google Scholar * Huang, X. _et al_. Exosomal miR-1290 and miR-375 as prognostic markers in castration-resistant prostate cancer. _Eur. Urol._ 67, 33–41 (2015).
Article CAS PubMed Google Scholar * Bryant, R. J. _et al_. Changes in circulating microRNA levels associated with prostate cancer. _Br. J. Cancer_ 106, 768–774 (2012). Article CAS
PubMed PubMed Central Google Scholar * Kneitz, B. _et al_. Survival in patients with high-risk prostate cancer is predicted by mir-221, which regulates proliferation, apoptosis, and
invasion of prostate cancer cells by inhibiting IRF2 and SOCS3. _Cancer Res._ 74, 2591–2603 (2014). Article CAS PubMed Google Scholar * Porkka, K. P. _et al_. MicroRNA expression
profiling in prostate cancer. _Cancer Res._ 67, 6130–6135 (2007). Article CAS PubMed Google Scholar * Ozen, M., Creighton, C. J., Ozdemir, M. & Ittmann, M. Widespread deregulation of
microRNA expression in human prostate cancer. _Oncogene_ 27, 1788–1793 (2008). Article CAS PubMed Google Scholar * Spahn, M. _et al_. Expression of microRNA-221 is progressively reduced
in aggressive prostate cancer and metastasis and predicts clinical recurrence. _Int. J. Cancer_ 127, 394–403 (2010). CAS PubMed Google Scholar * Fu, X. _et al_. Clinical significance of
miR-221 and its inverse correlation with p27 Kip1 in hepatocellular carcinoma. _Mol. Biol. Rep._ 38, 3029–3035 (2011). Article CAS PubMed Google Scholar * Igoucheva, O. & Alexeev, V.
MicroRNA-dependent regulation of cKit in cutaneous melanoma. _Biochem. Biophys. Res. Commun._ 379, 790–794 (2009). Article CAS PubMed Google Scholar * Chun-zhi, Z. _et al_. MicroRNA-221
and microRNA-222 regulate gastric carcinoma cell proliferation and radioresistance by targeting PTEN. _BMC Cancer_ 10, 367 (2010). Article PubMed PubMed Central CAS Google Scholar *
Garofalo, M. _et al_. miR-221&222 Regulate TRAIL Resistance and Enhance Tumorigenicity through PTEN and TIMP3 Downregulation. _Cancer Cell_ 16, 498–509 (2009). Article CAS PubMed
PubMed Central Google Scholar * Xiao, J. _et al_. MiR-141 modulates androgen receptor transcriptional activity in human prostate cancer cells through targeting the small heterodimer
partner protein. _Prostate_ 72, 1514–1522 (2012). Article CAS PubMed Google Scholar * Gui, B., Hsieh, C. L., Kantoff, P. W., Kibel, A. S. & Jia, L. Androgen receptor-mediated
downregulation of microRNA-221 and -222 in castration-resistant prostate cancer. _PLoS One_ 12 (2017). * Guinney, J. _et al_. Prediction of overall survival for patients with metastatic
castration-resistant prostate cancer: development of a prognostic model through a crowdsourced challenge with open clinical trial data. _Lancet Oncol._ 18, 132–142 (2017). Article PubMed
Google Scholar * Cornford, P. _et al_. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part II: Treatment of Relapsing, Metastatic, and Castration-Resistant Prostate Cancer. _Eur. Urol._ 71,
630–642 (2017). Article PubMed Google Scholar * Scher, H. I. _et al_. Trial design and objectives for castration-resistant prostate cancer: Updated recommendations from the prostate
cancer clinical trials working group 3. _J. Clin. Oncol._ 34, 1402–1418 (2016). Article PubMed PubMed Central Google Scholar * Eisenhauer, E. A. _et al_. New response evaluation criteria
in solid tumours: Revised RECIST guideline (version 1.1). _Eur. J. Cancer_ 45, 228–247 (2009). Article CAS PubMed Google Scholar * Zedan, A. H. _et al_. Heterogeneity of miRNA
expression in localized prostate cancer with clinicopathological correlations. _PLoS One_ 12, 1–17 (2017). Article CAS Google Scholar * Zedan, A. H., Hansen, T. F. & Jo, P. microRNA
expression in tumour tissue and plasma in patients with newly diagnosed metastatic prostate cancer. _Tumor Biol._ 40, 1–11 (2018). Article CAS Google Scholar Download references
ACKNOWLEDGEMENTS Many thanks to Jeanet Jørgensen, Marianne M. Hansen, and Lone Frischknecht for their excellent technical assistance. Special thanks to Karin Larsen for linguistic editing of
the manuscript. We would also like to thank OPEN, Odense Patient Data Explorative Network, Odense University Hospital, Odense, Denmark for data management. This work was supported by the
Research Council of Lillebaelt Hospital and the Japanese-Swedish Research Foundation. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Urological Research Centre, Department of Urology, Vejle
Hospital, Vejle, Denmark A. H. Zedan & P. J. S. Osther * Department of Oncology, Vejle Hospital, Vejle, Denmark A. H. Zedan & T. F. Hansen * Department of Biochemistry and Clinical
Immunology, Vejle Hospital, Vejle, Denmark J. Assenholt & J. S. Madsen * Institute of Regional Health Research, University of Southern Denmark, Odense, Denmark A. H. Zedan, P. J. S.
Osther, J. S. Madsen & T. F. Hansen Authors * A. H. Zedan View author publications You can also search for this author inPubMed Google Scholar * P. J. S. Osther View author publications
You can also search for this author inPubMed Google Scholar * J. Assenholt View author publications You can also search for this author inPubMed Google Scholar * J. S. Madsen View author
publications You can also search for this author inPubMed Google Scholar * T. F. Hansen View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS
A.H.Z. wrote the main manuscript text and prepared figures. All authors; P.J.S.O., J.A., J.S.M. and T.F.H. reviewed the manuscript. CORRESPONDING AUTHOR Correspondence to A. H. Zedan. ETHICS
DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in
published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY FIGURES S1 AND S2. SUPPLEMENTARY DATASET 1. SUPPLEMENTARY DATASET 2. SUPPLEMENTARY DATASET 3.
SUPPLEMENTARY DATASET 4. SUPPLEMENTARY INFORMATION 5A SUPPLEMENTARY INFORMATION 5B RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0
International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the
source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative
Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by
statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Zedan, A.H., Osther, P.J.S., Assenholt, J. _et al._ Circulating miR-141 and miR-375
are associated with treatment outcome in metastatic castration resistant prostate cancer. _Sci Rep_ 10, 227 (2020). https://doi.org/10.1038/s41598-019-57101-7 Download citation * Received:
03 July 2019 * Accepted: 20 December 2019 * Published: 14 January 2020 * DOI: https://doi.org/10.1038/s41598-019-57101-7 SHARE THIS ARTICLE Anyone you share the following link with will be
able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing
initiative