Fast eating is a strong risk factor for new-onset diabetes among the japanese general population
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Although many studies that have examined the relationship of type and amount of food and the frequency of eating with new onset of diabetes, there are few reports on the
relationship between how meals are eaten, such as skipping breakfast, snacking or food ingestion speed, and the onset of diabetes. We investigated the relationship between eating speed, as
well as other eating habits such as snacking and skip breakfast, and new onset of diabetes in a nation-wide Japanese cohort. We obtained data from the nation-wide annual health check program
in Japan. In 197,825 participants without diabetes in 2008, questionnaires recorded data on the diet habits (eating speed, snack after supper or before sleep, and skipping breakfast) and
unadjusted and multivariable-adjusted logistic regression models were used to measure the odds ratio of new-onset diabetes mellitus in a 3-year follow up. The proportion of fast eaters,
those who snack after supper, snack before sleep, and skip breakfast was higher in the new-onset diabetes group than in the group who did not develop diabetes mellitus. As compared with the
non-fast eater group, fast eaters were generally younger, had higher BMI, had more weight gain from 20 years onwards, and experienced frequent weight fluctuations of ≥3 kg within 1 year. The
risk of fast eaters developing diabetes mellitus remained even after correction for multiple factors including age, body weight, rate of weight change, blood pressure, smoking, and alcohol
consumption. No other eating habits were independent predictors for onset of diabetes mellitus. Results show that fast eating is a sole predisposing factor among eating habits for new-onset
diabetes. Future studies were warranted to evaluate whether avoidance of fast eating is beneficial for prevention of diabetes mellitus. SIMILAR CONTENT BEING VIEWED BY OTHERS EATING BEFORE
BED AND NEW-ONSET HYPERTENSION IN A JAPANESE POPULATION: THE IKI CITY EPIDEMIOLOGICAL STUDY OF ATHEROSCLEROSIS AND CHRONIC KIDNEY DISEASE Article 22 September 2021 MEAL TIMING ACROSS THE DAY
MODULATES DAILY ENERGY INTAKE IN ADULT PATIENTS WITH TYPE 2 DIABETES Article 06 April 2022 ASSOCIATION BETWEEN FAST EATING SPEED AND METABOLIC DYSFUNCTION-ASSOCIATED STEATOTIC LIVER
DISEASE: A MULTICENTER CROSS-SECTIONAL STUDY AND META-ANALYSIS Article Open access 14 August 2024 INTRODUCTION Many previous studies clarified the influence of type and amount of food and
eating frequency on new onset diabetes1,2. There are also reports concerning effects of skipping breakfast and/or snacking on onset of diabetes3,4,5. However, reports on eating speed are
scarce. Sakurai _et al_. investigated the association between eating speed and the incidence of type 2 diabetes in 2,050 Japanese men employees of a metal products factory6. As compared to
slow eating speed, medium (1.68, 95% CI 0.93–3.02) and fast (1.97, 1.10–3.55) eating speed showed increased hazard ratios for new onset of diabetes (p for trend = 0.030). In a Lithuanian
case-control study included 234 cases with newly diagnosed type 2 diabetes, fast eaters showed an increased risk of type 2 diabetes as compared to slow eaters (odds ratio 2.52; 95% CI
1.56–4.06, p < 0.001)7. However, the assumption is limited by small numbers of subjects, inclusion bias and lack of information for other confounding eating habits. We investigated the
effects of eating speed, as well as other eating habits such as snacking and skip breakfast on new onset of diabetes in a Japanese nation-wide large cohort. RESULTS GENERAL CHARACTERISTICS
General characteristics are shown in Table 1. The average age of the participants was 63.7 years, and 38.0% of participants were men. There were 7032/198187 (3.54%) patients who were not
diabetic in 2008 and who developed diabetes between 2009 and 2011. Among fast eaters, the number of patients who developed diabetes mellitus was 30.9% compared with 26.1% who did not develop
diabetes mellitus. Among patients who snack after supper, 12.9% developed diabetes mellitus whereas 12.9% did not. Among patients who snack before sleep, 17.2% developed diabetes mellitus
compared with 15.0% who did not, and 12.9% of patients who skipped breakfast developed diabetes mellitus compared with 12.4% who did not. Significant differences were found in all
categories, and being a fast eater was the most significant risk factor for new-onset diabetes mellitus. CHARACTERISTICS OF FAST EATERS We compared the characteristics at baseline for fast
eaters with those for moderate + slow eaters (non-fast eaters) (Table 2). Fast eaters were generally younger (61.6 years vs 64.1 years), men (41.6% vs 36.8%), with higher BMI (24.2 vs 22.5
kg/m2). Fast eaters more frequently gained weight of >10 kg (40.8% vs 27.7%) and frequent fluctuations of ≥3 kg or more in one year (26.9 vs 17.5%). At baseline, in men, the average BMI
in fast eaters 24.1 kg/m2 vs 23.4 kg/m2 in non-fast eaters indicate + BMI 0.7 kg/m2 difference (P < 0.01). In women, the average BMI in fast eaters 23.4 kg/m2 vs 22.2 kg/m2 in non-fast
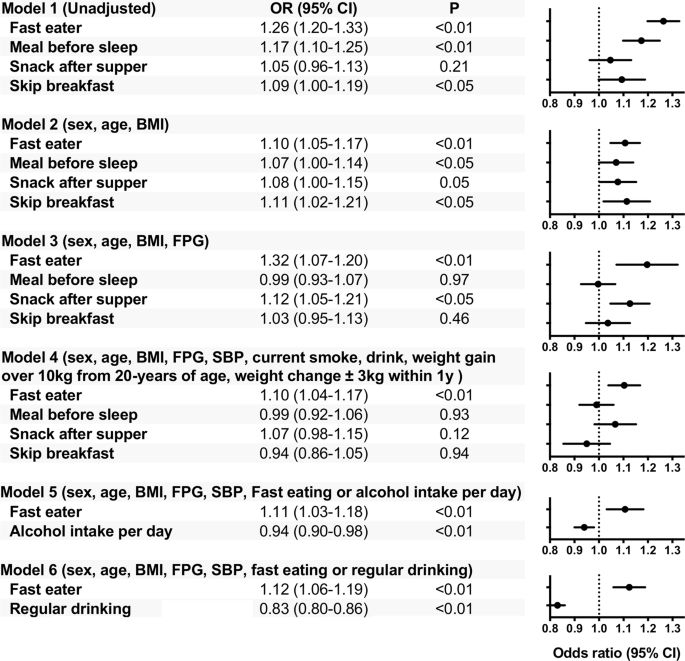
eaters indicate + BMI 1.2 kg/m2 (_P_ < 0.01). ODDS RATIO OF NEW DIABETES ONSET BY LOGISTIC REGRESSION ANALYSIS The odds ratio (OR) for onset of diabetes due to difference in eating habits
was examined by logistic regression analysis. Being a fast eater les to a significantly increased risk of diabetes mellitus (OR 1.26, 95% confidence interval [CI] 1.20–1.33, P < 0.01),
as did snacking before sleep (OR 1.17, 95% CI 1.10–1.25, P < 0.01), and skipping breakfast (OR 1.09, 95% CI 1.00–1.19, P < 0.05) (Model 1). In Model 3, snacking before sleep and
skipping breakfast had no significant differences. There was no difference in patients who snacked after supper with regard to unadjusted OR; however, it was identified as significant
following multivariate risk correction (Model 3). In Model 4, even if “change in body weight from 20 years old was 10 kg or more” and “a change in weight over 1 year of ≥3 kg” were included
as adjustment factors, fast eaters was an independent factor for diabetes onset. Snacking before sleep, snacking after supper, and skipping breakfast were not independent factors. Because
alcohol drinking might be mutually correlated with eating habits, we compiled degree of the alcohol consumption or presence of regular drinking on the OR calculation as follows. In the model
compiling alcohol intake per day (Model 5). Results indicated that fast eating and alcohol consumption was independently and inversely associated with diabetes onset. In the model compiling
presence or absence of regular (everyday) drinking (Model 6). Results indicated that fast eating and regular (everyday) drinking was independently and inversely associated with diabetes
onset. DISCUSSION This study obtained three major findings. First, the proportion of fast eaters, those who snack after supper, snack before sleep, and skip breakfast was higher in the
new-onset diabetes group than in the group who did not develop diabetes mellitus (Table 1). Second, the fast eaters were younger, had higher BMI, had more weight gain from 20 years onwards,
and experienced frequent weight fluctuations of ≥3 kg within 1 year as compared with the non-fast eater group (Table 2). Third, the risk of fast eaters developing diabetes mellitus remained
significant after correction for multiple factors including age, body weight, rate of weight change, blood pressure, smoking, and alcohol consumption. Other major eating habits were not
independent predictors for onset of diabetes mellitus. This study showed for the first time that fast eating is a sole predisposing factor among major eating habits for new-onset diabetes in
a large cohort. EATING HABITS AND ONSET OF DIABETES MELLITUS It is well known that breakfast skipping and frequent snacking are related to onset of diabetes with an increase in
obesity3,4,5. In our cohort, fast eaters were prevalent in the group of diabetes onset as well as those who snack after supper and before sleep, and skip breakfast (Table 1). Agreed to
earlier reports6,7, our large cohort study showed that fast eating is a determinant of new-onset diabetes mellitus. We further clarified the effects of eating speed were observed
independently of obesity and other diabetes-prone eating habits. CHARACTERISTICS OF FAST EATERS The fast eaters in our population were younger men with higher BMI and waist circumference,
lower HDL and higher triglycerides. Ohkuma _et al_. examined the relationship between eating speed and BMI in a meta-analysis of 15 observational studies, showing that BMI is higher in fast
eaters by an average of 1.78 kg/m2 (95% confidence interval [CI], 1.53–2.04 kg/m2) as compared to slow eaters8. Our fast eaters also showed +1.70 kg/m2 BMI as compared to non-fast eaters at
baseline. On the other hand, fast eaters also showed a higher weight gain. In longitudinal studies, body weight gains were: fast eaters+4.49 kg vs non-fast eaters +3.08 kg after 7 years) in
USA fire service personnel9 and fast eaters +1.9 kg vs medium and slow eaters +0.7 kg after 8 years in a Japanese company health-checkup10. In our study, fast eaters vs non-fast eaters
average weight gains from 2008 to 2011 were comparable in overall participants (−0.13 kg vs −0.20 kg, not significant). However, when fast eaters were divided into diabetes onset+ and
onset−, the change in body weight was statistically significant: in the diabetes onset group, body weight was 63.7 kg at baseline vs 64.8 kg at onset (+1.1 kg, _P_ < 0.01); in the
non-onset group, body weight was 60.2 kg at baseline vs 60.0 kg at last observation (2011) (−0.2 kg, _P_ < 0.01). FAST EATERS AND NEW-ONSET DIABETES Until now, information about the
relationship between eating speed and onset of diabetes has been limited6,7. Radzeviciene showed that the OR of fast eaters for new-onset diabetes was 2.52 among 234 Lithuanian with
new-onset diabetes cases and 468 non-diabetic controls7. Sakurai _et al_. reported that the OR of fast eaters was 1.97 (1.10–3.55) compared with slow eaters in Japanese men employees with an
average age of 45.9 years (35–55). However, when adjusted for BMI, there was no significant difference6. This study showed that fast eating is a sole independent determinant among major
eating habits such as snacking before sleep, snacking after supper, and skipping breakfast for the development of diabetes mellitus. It has been reported that late-night snacks, snacks,
skipping breakfast, or overeating are independent factors for diabetes onset4,5. However, in this large-scale study with heterogenous populations in terms of gender, age, area and jobs,
there was no significant difference when correction was made for confounding factors including snacking before sleep, snacking after supper, or skipping breakfast (Fig. 1, Models 3, 4),
suggesting that fast eaters are exceptionally in a high-risk group for the development of new-onset diabetes. POSSIBLE MECHANISM OF DIABETES ONSET BY FAST EATING Although the mechanism of
diabetes onset in fast eaters cannot be elucidated in the present study, previous studies have suggested the underlying mechanism(s). It can be discussed as obesity-dependent and
-independent mechanisms. OBESITY-DEPENDENT MECHANISMS It has been reported that workplace stress can increase the likelihood of fast eating11. Job stress is often accompanied by a change in
eating behaviors including fast eating, eating beyond the point of a full stomach12, surrogate meals or overeating, and increased calorie intake13, which were speculated in causes of obesity
in Japanese men and women14. In Japan, men were more likely to be employed on full-time than women; 22.78 million men vs 10.78 million women in full-time employment
(http://www.stat.go.jp/english/index.html). There is a large difference in obesity rate between men and women in Japan (BMI ≥ 25.0 kg/m2 28.9% of men vs 17.6% of women); the rate of obesity
was also higher among men in our study (men 27.3% vs women 19.9%)15. Fast eaters in this study were mainly middle-aged and elderly men engaged in work, where job stress might have led to
obesity. The proportion of fast eaters was 28.8% in men and 24.9% in women (Table 3). Taken above, prevalence of fast eaters and obesity can be increased by job stress more habitually in
men. The incidence of diabetes was 5.4% among men with fast eating vs 4.5% for total men. The proportion of women fast eaters who developed diabetes was 3.3% vs 2.6% for all women
participants. At baseline, BMI was higher in fast eaters both in men and women, but the difference in BMI between fast eaters and non-fast eaters lower in men (+0.7 kg/m2) than in women
(+1.2 kg/m2). Fast eaters in men might be more vulnerable to diabetes even with a small increase in BMI. Effects of eating speed on the risk of obesity and diabetes has also been reported in
Japanese men16. OBESITY-INDEPENDENT MECHANISMS As indicated by Model 4 in Fig. 1, diabetes occurs among fast-eaters irrespective of increases in body weight. First, eating faster reduces
energy consumption after meals17. Second, when the time for mastication is reduced, glucose and insulin concentrations are significantly higher between 90 and 240 minutes after
mastication18. Third, in soft-fed rats, postprandial hyperglycemia and hyperinsulinemia decreased levels of IRS2 expression in the liver and Akt phosphorylation was observed, which may lead
to increased risk of diabetes19. Because alcohol drinking might be mutually correlated with eating habits, we compiled degree of the alcohol consumption or regular drinking on the OR
calculation. In the model compiling alcohol or regular (everyday) drinking, fast eater was associated with onset of diabetes independently of the alcohol consumption and presence of regular
drinking. There are limitations to this study. First, in this Japanese nation-wide health examination system, ~51.91 million people aged between 40 and 74 years who should have undergone
health examination between March 2008 and April 2009; however, only 20.05 million people (37.4%) underwent the examination and only parts of all participants could be evaluated by our study
because of fails of contracts with all local governments. This heterogeneity may bias the results. Second, because of the age limit, the onset of diabetes before age 39 years remains
unknown. As such, this analysis is not relevant for juvenile-onset type 2 diabetes. Third, the outcomes based on self-reported data about eating habits. The Questionnaire on eating speed was
“How fast do you eat compared to others around same ages? (Faster, Normal, Slower)”. Although the judgement of eating behavior is subjective, this self-reported eating speed has been
validated for clinical utility20 and can be useful to prevent obesity in the Japanese “Specific Health Check and Guidance System (SHCG)”21, supporting our notice. Fourth, the observation
period was relatively short. Fifth, our criteria for definition of diabetes, fasting plasma glucose level ≥126 mg/dL or HbA1c levels ≥6.5%, may underestimate onset of diabetes. As reported
in a Japanese population22, the HbA1c cutoff of 6.0% had appropriate sensitivity and specificity for diabetes screening, suggesting that HbA1c ≥ 6.5% may be inadequate as a screening tool
for diabetes. CONCLUSIONS In conclusion, fast eating is a sole independent risk factor among major eating habits predisposing to the onset of diabetes. Future studies were warranted to
evaluate precise phenotypes of fast eaters and also to evaluate whether avoidance of fast eating is beneficial for prevention of diabetes mellitus. METHODS PARTICIPANTS The research is not a
clinical trial and therefore does not need to be registered. We used data from the annual health check program known as the Japanese “Specific Health Check and Guidance System
(SHCG)”23,24,25,26, launched by the Ministry of Health, Labour and Welfare (MHLW), in 2008. The SHCG aimed to gather data from Japanese people aged between 40 and 74 years; the estimated
number of subjects included in the database was 51,919,920. The current study was performed as a part of the ongoing project “Design of the comprehensive healthcare system for chronic kidney
disease (CKD) based on the individual risk assessment by Specific Health Checkups”. Twenty-seven of 47 prefectural governments in Japan agreed to participate in this project. One was
excluded due to missing follow-up data, leaving 27 prefectures (Hokkaido, Miyagi, Yamagata, Fukushima, Ibaraki, Tochigi, Tokyo, Saitama, Chiba, Kanagawa, Niigata, Nagano, Ishikawa, Fukui,
Gifu, Osaka, Hyogo, Okayama, Tokushima, Kochi, Fukuoka, Saga, Nagasaki, Oita, Kumamoto, Miyazaki, and Okinawa). The SHCG data recorded between 2008 and 2011 was sent to and verified by an
independent data center - the non-profit organization (NPO) ‘Japan Clinical Support Unit’ (Tokyo, Japan)23,24,25,26. The community approval was obtained from prefecture representatives. All
procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee at which the studies were
conducted (Fukushima Medical University; IRB Approval Number #1485, #2771) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The research was
not a clinical trial and therefore did not need to be registered. Our analyses not pre-specified are considered exploratory. Among 303,654 participants without diabetes mellitus in 2008
(Supplemental Figure), we excluded participants who visited only once in 2008 and those with incomplete data, such as sex, age, body mass index (BMI), systolic blood pressure (SBP),
diastolic blood pressure (DBP), fasting plasma glucose levels, glycated hemoglobin (HbA1c). We selected 197,825 participants without diabetes mellitus (see definition below) in 2008.
MEASUREMENTS Trained staff measured the height, body weight, blood pressure, and waist circumference of each subject. Questionnaires recorded data on the following; smoking status (current
smoker or not); drinking habits (every day, sometimes, rarely or never); diet habits (eating speed, snack after supper or before sleep, and skipping breakfast); regular exercise (walking
>1 hour/day, rarely or never); anti-hypertensive drug use; anti-diabetic drug use; lipid-lowering drug use. Questionnaires about diet habit were: Do you skip breakfast ≥three days per
week? (Yes or No), Do you have an evening meal within two hours before bedtime ≥three days per week? (Yes or No), Do you eat a snack after your evening meal (fourth meal) ≥three days per
week? (Yes or No), How fast do you eat compared to others around same ages? (Faster, Normal, Slower). Blood samples were collected after an overnight fast and were assayed within 24 hours
with automatic clinical chemical analyzers. When required, HbA1c was corrected in line with national glycohemoglobin standardization program equivalent values, calculated using the following
formula: HbA1c (%) = HbA1c (Japan Diabetes Society) (%) +0.4% 0.13. DEFINITION OF DIABETES MELLITUS, HYPERTENSION AND DYSLIPIDEMIA For this study, a participant was considered to have
diabetes mellitus when the fasting plasma glucose level was ≥126 mg/dL, when HbA1c levels were ≥6.5% (48 mmol/mol), or if the participant had self-reported the use of anti-hyperglycemic
drugs in 2008. Participants were considered to have new-onset diabetes mellitus if they met the above criteria in 2009, 2010, or 2011. Participants were considered hypertensive if their SBP
was ≥140 mmHg, if their DBP was ≥90 mmHg, or if they had self-reported the use of antihypertensive drugs. Participants were considered to have dyslipidemia if high-density lipoprotein
(HDL)-C levels were <40 mg/dL (1.0 mmol/L), if low-density lipoprotein (LDL)-C levels were ≥140 mg/dL (3.6 mmol/L), if triglyceride (TG) levels were ≥150 mg/dL (1.7 mmol/L), or if they
had self-reported the use of lipid-lowering drugs. STATISTICAL ANALYSES A t-test or chi-square test was used to compare the group means (Tables 1 and 2). Unadjusted and
multivariable-adjusted logistic regression models were used to estimate the association between new-onset diabetes mellitus and diet habits over 1–3 years of follow-up. In the first step, we
carried out unadjusted analyses (Fig. 1, Model 1). In the second step, we adjusted for age, sex, and BMI (Model 2). In the third step, we further adjusted for fasting plasma glucose (Model
3). In the fourth step, we further adjusted for current smoking status, drinking habits, weight gain (over 10 kg from the age of 20 years and weight change ≥3 kg within 1 year) (Model 4). In
the fifth steps, model compiling alcohol intake per day as stratified (Model 5): alcohol consumption: 1, under 20 g; 2, 20 g to less than 40 g; 3, 40 g to less than 60 g; 4, over 60 g. In
the sixths steps, presence or absence of regular (everyday) drinking (Model 6): 1, rare or none: 2, sometimes; 3, everyday. All analyses were performed using SPSS software (version 24.0;
SPSS, Chicago, IL, USA). ETHICS APPROVAL AND CONSENT TO PARTICIPATE All procedures performed in studies involving human participants were in accordance with the ethical standards of the
institutional and/or national research committee at which the studies were conducted (Fukushima Medical University; IRB Approval Number #1485, #2771) and with the 1964 Helsinki declaration
and its later amendments or comparable ethical standards. This study was conducted according also to the Ethical Guidelines for Medical and Health Research Involving Human Subjects enacted
by MHLW of Japan [http://www.mhlw.go.jp/file/06-Seisakujouhou-10600000-Daijinkanboukouseikagakuka/0000069410.pdf and
http://www.mhlw.go.jp/file/06-Seisakujouhou-10600000-Daijinkanbou-kouseikagakuka/0000080278.pdf]. CONSENT FOR PUBLICATION The investigators shall not necessarily be required to obtain
informed consent, but we made public information concerning this study on the web [http://www.fmu.ac.jp/univ/sangaku/data/koukai _2/2771.pdf] and ensured the opportunities for the research
subjects to refuse utilizing their personal information. DATA AVAILABILITY The datasets used and analyzed during the current study are available from the corresponding author on reasonable
request. REFERENCES * Fung, T. T., Schulze, M., Manson, J. E., Willett, W. C. & Hu, F. B. Dietary patterns, meat intake, and the risk of type 2 diabetes in women. _Arch Intern Med._ 164,
2235–40 (2004). Article Google Scholar * van Dam, R. M., Rimm, E. B., Willett, W. C., Stampfer, M. J. & Hu, F. B. Dietary patterns and risk for type 2 diabetes mellitus in U.S. men.
_Ann Intern Med._ 136, 201–9 (2002). Article Google Scholar * Mekary, R. A. _et al_. Eating patterns and type 2 diabetes risk in older women: breakfast consumption and eating frequency.
_Am J Clin Nutr._ 98, 436–43 (2013). Article CAS Google Scholar * Odegaard, A. O. _et al_. Breakfast frequency and development of metabolic risk. _Diabetes Care._ 36, 3100–6 (2013).
Article Google Scholar * Uemura, M. _et al_. Breakfast Skipping is Positively Associated With Incidence of Type 2 Diabetes Mellitus: Evidence From the Aichi Workers’ Cohort Study. _J
Epidemiol._ 25, 351–8 (2015). Article Google Scholar * Sakurai, M. _et al_. Self-reported speed of eating and 7-year risk of type 2 diabetes mellitus in middle-aged Japanese men.
_Metabolism._ 61, 1566–71 (2012). Article CAS Google Scholar * Radzeviciene, L. & Ostrauskas, R. Fast eating and the risk of type 2 diabetes mellitus: a case-control study. _Clin
Nutr._ 32, 232–5 (2013). Article CAS Google Scholar * Ohkuma, T. _et al_. Association between eating rate and obesity: a systematic review and meta-analysis. _Int J Obes (Lond)._ 39,
1589–96 (2015). Article CAS Google Scholar * Gerace, T. A. & George, V. A. Predictors of weight increases over 7 years in fire fighters and paramedics. _Prev Med._ 25, 593–600 (1996).
Article CAS Google Scholar * Tanihara, S. _et al_. Retrospective longitudinal study on the relationship between 8-year weight change and current eating speed. _Appetite._ 57, 179–83
(2011). Article Google Scholar * Nishitani, N. & Sakakibara, H. Relationship of obesity to job stress and eating behavior in male Japanese workers. _Int J Obes (Lond)._ 30, 528–33
(2006). Article CAS Google Scholar * Takaki, J. _et al_. Interactive effects of job stress and body mass index on over-eating. _J Occup Health._ 52, 66–73 (2010). Article Google Scholar
* Wardle, J., Steptoe, A., Oliver, G. & Lipsey, Z. Stress, dietary restraint and food intake. _J Psychosom Res._ 48, 195–202 (2000). Article CAS Google Scholar * Fujishiro, K.,
Lividoti Hibert, E., Schernhammer, E. & Rich-Edwards, J. W. Shift work, job strain and changes in the body mass index among women: a prospective study. _Occup Environ Med._ 74, 410–6
(2017). Article Google Scholar * Ng, M. _et al_. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the
Global Burden of Disease Study 2013. _Lancet._ 384, 766–81 (2014). Article Google Scholar * Ohkuma, T. _et al_. Impact of eating rate on obesity and cardiovascular risk factors according
to glucose tolerance status: the Fukuoka Diabetes Registry and the Hisayama Study. _Diabetologia._ 56, 70–7 (2013). Article CAS Google Scholar * Hamada, Y., Kashima, H. & Hayashi, N.
The number of chews and meal duration affect diet-induced thermogenesis and splanchnic circulation. _Obesity (Silver Spring)._ 22, E62–9 (2014). Article CAS Google Scholar * Mattes, R. D.
& Considine, R. V. Oral processing effort, appetite and acute energy intake in lean and obese adults. _Physiol Behav._ 120, 173–81 (2013). Article CAS Google Scholar * Bae, C. R. _et
al_. Possible involvement of food texture in insulin resistance and energy metabolism in male rats. _J Endocrinol._ 222, 61–72 (2014). Article CAS Google Scholar * Tayama, J., Ogawa, S.,
Takeoka, A., Kobayashi, M. & Shirabe, S. Item response theory-based validation of a short form of the Eating Behavior Scale for Japanese adults. _Medicine._ 96, e8334–e (2017). Article
Google Scholar * Nagahama, S. _et al_. Self-reported eating rate and metabolic syndrome in Japanese people: cross-sectional study. _BMJ open._ 4, e005241–e (2014). Article Google Scholar
* Shimodaira, M., Okaniwa, S., Hanyu, N. & Nakayama, T. Optimal Hemoglobin A1c Levels for Screening of Diabetes and Prediabetes in the Japanese Population. _J Diabetes Res._ 2015,
932057 (2015). Article Google Scholar * Iseki, K. _et al_. Risk factor profiles based on estimated glomerular filtration rate and dipstick proteinuria among participants of the Specific
Health Check and Guidance System in Japan 2008. _Clin Exp Nephrol._ 16, 244–9 (2012). Article CAS Google Scholar * Wakasugi, M. _et al_. Association between combined lifestyle factors and
non-restorative sleep in Japan: a cross-sectional study based on a Japanese health database. _PLoS One._ 9, e108718 (2014). Article ADS Google Scholar * Yano, Y. _et al_. Long-Term Blood
Pressure Variability, New-Onset Diabetes Mellitus, and New-Onset Chronic Kidney Disease in the Japanese General Population. _Hypertension._ 66, 30–6 (2015). Article CAS Google Scholar *
Hasegawa, K. _et al_. Control Status of Atherosclerotic Cardiovascular Risk Factors Among Japanese High-Risk Subjects:Analyses of a Japanese Health Check Database from 2008 to 2011. _J
Atheroscler Thromb._ 23, 991–1003 (2016). Article CAS Google Scholar Download references ACKNOWLEDGEMENTS This study was supported by a Health and Labor Sciences Research Grant for the
“Design of the comprehensive health care system for chronic kidney disease (CKD) based on the individual risk assessment by Specific Health Check” from the Ministry of Health. AUTHOR
INFORMATION AUTHORS AND AFFILIATIONS * Department of Diabetes, Endocrinology and Metabolism, School of Medicine, Fukushima Medical University, Fukushima, Japan Akihiro Kudo, Hiroaki Satoh
& Michio Shimabukuro * Steering Committee of Research on Design of the Comprehensive Health Care System for Chronic Kidney Disease (CKD) Based on the Individual Risk Assessment by
Specific Health Check, Fukushima, Japan Koichi Asahi, Kunitoshi Iseki, Toshiki Moriyama, Kunihiro Yamagata, Kazuhiko Tsuruya, Shouichi Fujimoto, Ichiei Narita, Tsuneo Konta, Masahide Kondo,
Yugo Shibagaki, Masato Kasahara & Tsuyoshi Watanabe Authors * Akihiro Kudo View author publications You can also search for this author inPubMed Google Scholar * Koichi Asahi View author
publications You can also search for this author inPubMed Google Scholar * Hiroaki Satoh View author publications You can also search for this author inPubMed Google Scholar * Kunitoshi
Iseki View author publications You can also search for this author inPubMed Google Scholar * Toshiki Moriyama View author publications You can also search for this author inPubMed Google
Scholar * Kunihiro Yamagata View author publications You can also search for this author inPubMed Google Scholar * Kazuhiko Tsuruya View author publications You can also search for this
author inPubMed Google Scholar * Shouichi Fujimoto View author publications You can also search for this author inPubMed Google Scholar * Ichiei Narita View author publications You can also
search for this author inPubMed Google Scholar * Tsuneo Konta View author publications You can also search for this author inPubMed Google Scholar * Masahide Kondo View author publications
You can also search for this author inPubMed Google Scholar * Yugo Shibagaki View author publications You can also search for this author inPubMed Google Scholar * Masato Kasahara View
author publications You can also search for this author inPubMed Google Scholar * Tsuyoshi Watanabe View author publications You can also search for this author inPubMed Google Scholar *
Michio Shimabukuro View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS A.K. and M.S. developed the concept, researched the data, and wrote the
manuscript. K.A., H.S., K.I., T.M., K.Y., K.T., S.F., I.N., T.K., M.Ko., Y.S., M.Ka. and T.W. contributed to discussion and reviewed the manuscript. K.A., K.I. and T.W. had full access to
all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. CORRESPONDING AUTHOR Correspondence to Michio Shimabukuro. ETHICS
DECLARATIONS COMPETING INTERESTS This work was supported by Health and Labor Sciences Research Grants: 1) Research on the Positioning of Chronic Kidney Disease (CKD) in Specific Health Check
and Guidance in Japan, 2) Study on the Appropriate States of Specific Health Checkups and Specific Health Guidance for Prevention of CKD Progression, and 3) Design of a Comprehensive Health
Care System for CKD Based on the Individual Risk Assessment by Specific Health Checkups from the Ministry of Health, Labor and Welfare of Japan (KA, KI, TM, KY, KT, SF, IN, TK, MKo, YS,
MKa, and TW), and 4) JSPS Grant-in-Aid for Scientific Research (C) #17K00924 (AK and MS) and #16K01823 (MS). The authors have no non-financial competing interests as defined by Nature
Research, or other interests that might be perceived to influence the interpretation of the article. ADDITIONAL INFORMATION PUBLISHER’S NOTE: Springer Nature remains neutral with regard to
jurisdictional claims in published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTAL FIGURES: FLOW CHART OF PARTICIPANTS RIGHTS AND PERMISSIONS OPEN ACCESS This
article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as
you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party
material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s
Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Kudo, A., Asahi, K., Satoh, H. _et al._ Fast
eating is a strong risk factor for new-onset diabetes among the Japanese general population. _Sci Rep_ 9, 8210 (2019). https://doi.org/10.1038/s41598-019-44477-9 Download citation *
Received: 22 October 2018 * Accepted: 15 May 2019 * Published: 03 June 2019 * DOI: https://doi.org/10.1038/s41598-019-44477-9 SHARE THIS ARTICLE Anyone you share the following link with will
be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt
content-sharing initiative