In situ bioprinting of autologous skin cells accelerates wound healing of extensive excisional full-thickness wounds
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT The early treatment and rapid closure of acute or chronic wounds is essential for normal healing and prevention of hypertrophic scarring. The use of split thickness autografts is
often limited by the availability of a suitable area of healthy donor skin to harvest. Cellular and non-cellular biological skin-equivalents are commonly used as an alternative treatment
option for these patients, however these treatments usually involve multiple surgical procedures and associated with high costs of production and repeated wound treatment. Here we describe a
novel design and a proof-of-concept validation of a mobile skin bioprinting system that provides rapid on-site management of extensive wounds. Integrated imaging technology facilitated the
precise delivery of either autologous or allogeneic dermal fibroblasts and epidermal keratinocytes directly into an injured area, replicating the layered skin structure. Excisional wounds
bioprinted with layered autologous dermal fibroblasts and epidermal keratinocytes in a hydrogel carrier showed rapid wound closure, reduced contraction and accelerated re-epithelialization.
These regenerated tissues had a dermal structure and composition similar to healthy skin, with extensive collagen deposition arranged in large, organized fibers, extensive mature vascular
formation and proliferating keratinocytes. SIMILAR CONTENT BEING VIEWED BY OTHERS UTILIZATION OF PATTERNED BIOPRINTING FOR HETEROGENEOUS AND PHYSIOLOGICALLY REPRESENTATIVE RECONSTRUCTED
EPIDERMAL SKIN MODELS Article Open access 18 March 2021 MULTI-FACETED ENHANCEMENT OF FULL-THICKNESS SKIN WOUND HEALING BY TREATMENT WITH AUTOLOGOUS MICRO SKIN TISSUE COLUMNS Article Open
access 18 January 2021 UTILIZATION OF EX VIVO TISSUE MODEL TO STUDY SKIN REGENERATION FOLLOWING MICRONEEDLE STIMULI Article Open access 27 October 2022 INTRODUCTION Chronic wounds such as
diabetic, venous and pressure ulcers and burn wounds represent a burden to patients and surgeons, affecting over 7 million patients in the United States with an annual treatment expenditure
of $25 billion. Chronic, large or non-healing wounds are especially costly because they often require multiple treatments; for example, a single diabetic foot ulcer can cost approximately
$50,000 to treat1. Full thickness skin injuries are a major source of mortality and morbidity for civilians, with an estimated 500,000 civilian burns treated in the United States each
year2,3. For military personnel, burn injuries account for 10–30% of combat casualties in conventional warfare4. The early excision and the proper coverage of wounds are vital steps in
increasing the survivability of patients with extensive burn injuries. Patients who suffer from these types of wounds respond best when rapid treatments are available that result in closure
and protection of the wounds as fast as possible. Early treatment of wounds is crucial to prevent wounds from worsening with time and causing further tissue damage and long-term hypertrophic
scarring. Patients who receive delayed treatments, or under-performing treatments, often are subject to extensive scarring that can result in long-term physiological defects such as
disfigurements and loss of range of motion. Split thickness autografts are regarded as the “gold standard” technique for treating severe wounds5. However, the adequate coverage of wounds is
often a challenge particularly when there is limited availability of healthy donor skin to harvest. Allografts are an option, but risk immune rejection of the graft6. These limitations have
led to the development of dermal substitutes, which are most often comprised of a synthetic or biological scaffold with, or without the inclusion of cells. Although such materials result in
improved wound healing7,8,9 they are costly to produce and result in relatively poor cosmetic outcomes. Tissue engineering approaches have led to more complex biological skin equivalents as
an alternative option to autografts10,11,12. The inclusion of both major skin cell types (keratinocytes and fibroblasts) in a single graft has been shown to improve skin regeneration in burn
wounds13,14 and promote closure of chronic diabetic foot ulcers, when compared with standard therapies15,16. Unfortunately, these skin substitutes are also hard to produce with custom sizes
and dimensions so lack the ability to adequately cover wounds with varying depth or topography. Cellular therapy is a promising alternative to biological skin-equivalents. A successful
cell-based technique could rapidly cover wounds and accelerate healing using living components. Epidermal keratinocytes and dermal fibroblasts can be easily isolated from a small biopsy of
uninjured skin tissue17 and applied to the wound using a manually seeded matrix or with cell spraying methods18,19,20. Rapid wound coverage has been achieved through transplantation of a
suspension of either freshly harvested or culture expanded keratinocytes at the time of wound debridement rather than the use of a coherent sheet of cells21,22,23. Additionally, it has been
shown that delivery of cells to the wound using techniques such as cell spraying results in faster healing and better cosmetic outcomes than those repaired with non-cellular
substitutes24,25. Unfortunately, the low delivery precision of current seeding and spraying technologies prevents the accurate delivery of specific cell types to the required target sites.
As a result, these current techniques cannot generate the complex skin structure that would be required to obtain functional and aesthetically acceptable results. In contrast to manual cell
seeding or cell spraying, bioprinting has the capability to deliver cells to specific target sites using layer-by-layer freeform fabrication, and it has been applied in numerous
applications26. Inkjet printers (also known as drop-on-demand printing) are the most commonly used type of printers for both non-biological and biological applications. Controlled volumes of
liquid are delivered to pre-defined locations using use thermal27,28 or acoustic29 forces to eject drops of liquid from the cartridge onto a substrate. Cartridges can deliver a wide variety
of biological materials, including cells, with high viability. In this study, we describe the design and a proof-of-concept validation of a novel mobile skin bioprinting system. The system
integrates imaging technology to determine the topography of a wound with precise _in-situ_ delivery of cells to tailor the technology to individual patient’s needs. Our device prints skin
cells directly into an injured wound, delivering dermal fibroblasts and epidermal keratinocytes to specific locations of the wound, replicating the layered skin structure, and accelerating
the formation of normal skin structure and function. RESULTS SKIN BIOPRINTER DESIGN AND CONSTRUCTION Tissue engineering has had initial successes with building a number of tissues
clinically, however, challenges still exist in developing and translating complex tissue systems that require coordinated and systemic function. Based on the shortcomings of the current
technologies and therapies of wound treatments, we established design criteria for an _in situ_ skin bioprinting system. The bioprinting system is: (1) portable and capable of being quickly
transported, (2) able to identify and measure a wide range of wound sizes and topologies accurately, (3) capable of delivering multiple cell types to precise spatial orientation tailored to
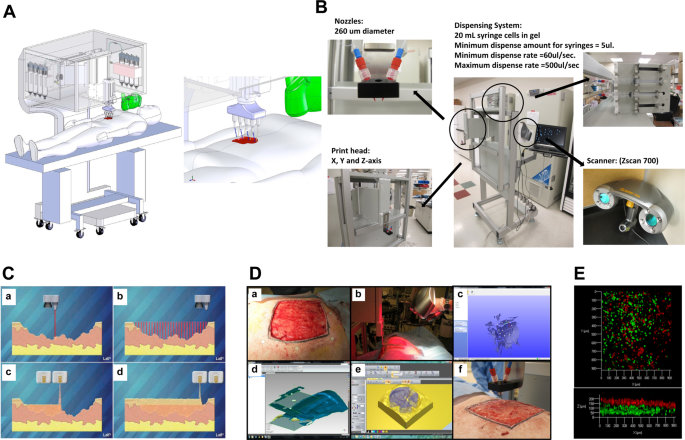
a individual wound, (4) easily sterilized, and (5) is easily operated and maintained with relatively low cost. A schematic demonstrating scale, design and components of the bioprinter system
is shown in Fig. 1A. The main components of the system consist of a hand-held 3D wound scanner, and a print-head with an XYZ movement system containing eight 260 µm diameter nozzles, each
driven by an independent dispensing motor. All components are mounted on a frame small enough to be mobile in the operating room (Fig. 1B). The dimensions of the system are 79 cm wide
(patient head to toe direction) by 77 cm deep (cross patient direction). When the robotic arm is fully extended, it hands out over the base an additional 50 cm so the full reach is 127 cm,
which is large enough to cover the torso of an average patient but small enough to easily pass through most doorframes. The skin bioprinter system is equipped with locks that engage with the
base of the patient table to prevent movement while printing cells. Once the system is in position over the patient these locks restrain the mobility of the system during the printing
process to ensure high delivery precision. The XYZ axes contribute to delivery precision by using a plotting system capable of 100 µm movements. In addition, the Z-axis allows the delivery
system to maintain the set distance from the surface of the wound to accommodate the curvature of patient’s body. Reconstructing skin wounds can be tailored to an individual patient by
combining a wound scanning system with the cartridge-based delivery system (Fig. 1C). To print a skin construct that exactly matches a patient’s wound, the current prototype incorporates a
real-time 3D laser scanner, ZScanner™ Z700 scanner (3DSystems, Rock Hill, SC), utilizing markers that are placed around the wound area used as reference points (Fig. 1D). The hand-held
scanner is easy to use and allows for easy maneuverability. The scanner offers the ability to capture the entire wound in one continuous scan. Once the scan is complete, the wound data is
compiled to form a model of the wound. The scanned wound area is then processed using Geomagic Studio software (Morrisville, NC) orient the model to standard coordinates so the import into
Artcam is ideal. Scanned data is in the form of an STL file that has been outputted from Geomagic and inputted to Artcam® 3D software to obtain the full volume and the nozzle path needed to
print the fill volume. The wound depth is then split into layers on the Z axis to determine which layers correspond to the dermis and epidermis (Fig. 1E). Each layer is overlaid with a
series of XY lines that cover the entire wound area. These lines are used in conjunction with the cartridge-based delivery system to determine a path for the printer. The skin cell delivery
system is controlled by a custom software employing a three-tiered architecture design based on the Microsoft.NET Framework 2.0 (Microsoft Corp®. Redmond, WA) and written in C++. The
three-tiered architecture handles three areas of communication: between the user and the software, among the software components, and between the software and the file system. This design
structure allows every component to be quickly and easily altered as necessary without affecting the other components. The cartridge-based delivery system is similar to that used in
traditional inkjet printing. The pressure-based delivery system uses three components: a delivery mechanism, the material reservoirs and a pressure source. The delivery system is based on
cartridges that can contain any material that can be delivered through the print-head nozzles, with each nozzle connecting to a separate cartridge. For the skin delivery system the contents
of each cartridge are embedded in a matrix composed of fibrinogen and collagen. Separate atomizing nozzles simultaneously deposit thrombin on the fibrinogen matrix to produce fibrin. Each
cell type is loaded into an individual cartridge in the same way different color inks would be contained in different cartridges. For our clinical printer, design updates were performed to
incorporate a more controllable piston-driven pressure mechanism. For the air-pressure system, air from the pressure source fills the reservoir and drives the material in the reservoir into
the delivery mechanism as it is needed. The system is pressurized with 6.89 kPa of compressed air using a two-stage control valve. The piston-driven pressure delivery was achieved with
individual syringe pumps, and was able to achieve identical pressures but with more control over ramping and depressurization. Both systems resulted in identical functional outcomes.
Together, these components provide a powerful new tool for treatment of large wounds. BIOPRINTING PROCEDURE The sterilization, preparation and bioprinting procedures are easy and quick to
perform. The system is designed to be covered with a sterile drape. The print-head is detachable and able to be autoclaved. Sterilization of tubing was performed by connecting cartridges of
70% ethanol followed by nano-filtered autoclaved water to clear the residual ethanol. A sterilization command directs the printer to automatically flush the delivery system with ethanol for
3 minutes followed by a sterile water flush for 1 minute. The user can choose to print using one of three different methods. First, the laser scanner can be used as previously described to
create a wound map for printing. Second, the user can define a series of bitmap images where each non-black pixel corresponds to a cell drop, and the color of the pixel corresponds to the
cell type to print. This method allows the user to create complex structures using any cell type in any configuration. Finally, a list of available cell types loaded in the printer is
provided to the user by the print-head configuration. In each method, the user defines the spacing between drops, and this is only limited by the resolution of the motors in the plotting
system. A laser sight guided the user to the upper-left corner of the wound and the distance from the laser to the first inkjet valve was used as a calibration that ensured accurate and
repeatable delivery of cells. The fibrin/collagen hydrogel carrier used in this study provides suitable support to maintain cellular viability, rapid crosslinking, and accurate depositing to
facilitate the formation of multicellular, multi-layered skin constructs. In these studies the integrated scanning system enabled us to rapidly measure and convert wound size, depth and
topology into a two layered format comprising of a lower fibroblast layer with an upper keratinocyte layer. BIOPRINTER VALIDATION IN A MURINE FULL-THICKNESS WOUND MODEL We first validated
the _in situ_ skin bioprinting system using a murine full thickness excisional wound model. In the 36 female outbred athymic nude (Nu/nu) mice used in this study, the mortality rate was 0%
and no wound infection or major skin irritation was noted on any mouse at any time point. Gross examination revealed that every printed skin construct appeared to form an epithelial coverage
over the wound at 1 week (Fig. 2A). This epithelium became more organized with time until the wound was completely covered. Organization into fully-formed skin required approximately 10–14
days post-printing. Wounds treated using _in-situ_ skin bioprinting demonstrated faster wound closure compared to untreated and matrix-treated group (Fig. 2B). In the printed group, the
wound area at 1 week post-surgery was 66% of the original wound area. In contrast, the wounds in the control groups remained at 95% of their original wound size at the same time point (n =
12, p ≤ 0.001). At 2 weeks, the wounds treated with printed cells were only 15% of the original size, while the wounds in the control groups were 40% of the original size (n = 8, p ≤ 0.05).
Overall, printed skin cells were able to close the entire wound by 3 weeks post-surgery compared to 5 weeks for both negative controls. Immunohistochemistry for human cells showed that human
fibroblasts and keratinocytes were present within the dermis and epidermis of the wound 3 weeks and 6 weeks after printing, together with endogenous cells (Fig. 2C). Control groups did not
show any staining for human cells. Histological examination of retrieved skin constructs revealed high cellularity of printed wounds one week after printing (Fig. 2D). This was expected, as
our system delivers approximately 500 cells per drop using the current prototype. This histological finding supports the observation of epithelialization of the bioprinted wounds, and
indicates that cells were present in the wound, perhaps forming an immature epidermal barrier. At week 3 and week 6 post-printing we observed the presence of a defined epidermis and
organized dermis consisting of aligned blue stained collagen fibers. This finding is consistent with the accelerated wound closure and re-epithelialization. In matrix-printed wounds, the
deposited hydrogel was visible within the wound area one week after printing, but as expected, lacked cellularity. At week 3 after treatment, matrix only-treated wounds showed increased
cellularity, suggesting migration of endogenous cells, however these wounds lacked a defined epidermis and showed minimal dermal organization. At week 6 after treatment matrix-only treated
wounds started to show epidermis formation and a more defined dermis with increased prominence of blue stained collagen fibers. Untreated wounds lacked both the cellularity and material
thickness observed in the other two groups at week one, but appeared similar to matrix only-treated wounds at week 3 and 6 In all printed constructs the dermis contained a highly organized
deep reticular layer and a less-organized papillary layer. The major three layers of the skin were present. All groups showed complete wound closure and healing by the end of week 6.
BIOPRINTER VALIDATION IN A PORCINE FULL-THICKNESS WOUND MODEL An overview of the porcine model study design is shown in Supplementary Fig. S1. All wounds formed granulation tissue by week 1
following excision, with greater levels of granulation appearing in the matrix, allogeneic and autologous cell-treated wounds (Fig. 3A). By week 2 we observed granulation tissue still
apparent in the allogeneic and autologous cell-treated wounds, but to a lesser extent in the matrix-treated wounds. At this time, we also observed the beginning of contraction in the
untreated wounds, with tattoo borders beginning to reduce in size and curve inwards, presenting a typical contractile wound shape. Autologous cell-treated wounds appeared to form a thin
epithelium over the majority of the wound area by 2 weeks, which then thickened and became white opaque from 4 weeks onwards. Interestingly, these opaque, white areas of epithelium
originated from small patches within the wound area, and grew throughout the time-course of the experiment, suggesting that these epithelial patches did not originate from the tissue edge
but rather from autologous cells applied with the bioprinter. During weeks 2 to 4, autologous cell-treated wounds contracted very little, while all other treatments appeared to contract
significantly, becoming reduced in total size, but also losing the square shape and becoming rectangular with pointed corners, suggesting contraction toward the center of the wounds. These
trends continued between weeks 4–8, with autologous cell-treated wounds showing increased opaque, white-appearing epithelium, while maintaining tissue shape and size. In contrast other
groups continued to contract, with little epithelium forming primarily from the edges of the wound. Between weeks 6 and 8 it appeared that all wounds had reached their final contracted size.
Wound size was measured for each wound once per week and recorded as area in centimeters squared (cm2) (Fig. 3B). One week following surgery, most wounds maintained their original size,
however, contraction did occur in the untreated wounds, resulting in a decrease in wound size to a mean of 87.75 ± 15.25 cm2 (p < 0.05). From this time-point onwards, untreated wounds
were statistically indistinguishable in size from matrix, and allogeneic cell-treated wounds, although the trend was for a smaller wound size at weeks 1 to 3. From week 2, 3, 4 and 5
autologous cell-treated wounds closed rapidly, and open wound area as significantly smaller than all other groups. Specifically measuring: 16.14 ± 15.29 cm2 at week 2 (p < 0.001 vs all
groups), 3.40 ± 4.64 cm2 at week 3 (p < 0.001 vs all groups), 1.46 ± 2.09 cm2 at week 4 (p < 0.001 vs all groups), and 0.00 ± 0.00 cm2 at week 5 (p < 0.05 vs all groups). From this
point onwards other treatments also trended in this direction, with no statistical differences between groups. These data suggest that the _in situ_ bioprinting of autologous cells resulted
in approximately 3-week acceleration in wound closure compared to other treatments. Wound contraction was measured for each wound at the wound tattoo border once per week and expressed as a
percentage of the original wound tattoo area (Fig. 3C). One week after treatment, all wounds other than untreated expanded in size, resulting in a negative contraction value. Untreated
wounds only showed minimal expansion. This effect is observed in many of our excisional wound models, and represents a combination of sagging or stretching of the wound area following full
thickness excision, with some contribution from swelling and granulation. By week 2, this trend was reversed with all groups showing positive contraction (shrinking), without statistically
significant differences between groups. At week 3 autologous cell-treated wounds were significantly less contracted than untreated wounds (14.33 ± 5.99% vs 34.3233 ± 10.24%, p < 0.05),
and at week 4 autologous cell-treated wounds were significantly less contracted than matrix-treated wounds (20.00 ± 8.96% vs 39.91 ± 12.42%, p < 0.05). However compared to
allogeneic-treated wounds there were no statistical differences at these time-points, although the obvious trend for the duration of the study was reduced contraction in autologous
cell-treated wounds. From weeks 5 to 8, autologous cell-treated wounds showed significantly less contraction than both untreated and matrix-treated wounds (week 5, p < 0.05; week 6–8, p
< 0.01) and also less contraction than allogeneic cell-treated wounds (p < 0.05). These data suggest that bioprinting autologous cells to full thickness wounds resulted in
approximately 50% reduction in wound contraction compared to other treatments over the time-course of the study. Wound re-epithelialization was expressed as a percentage of total area within
the tattoo border covered by epithelium (Fig. 3D). No epithelialization was recorded at week 0 or week 1 for any group. As early as week 2, autologous cell-treated wounds showed
significantly greater percentage of re-epithelialization compared to all groups between weeks 2 and 5. Specifically measuring: 86.83 ± 13.30% at week 2 (p < 0.001 vs all groups), 93.73 ±
7.12% at week 3 (p < 0.001 vs all groups), 97.24 ± 4.23% at week 4 (p < 0.001 vs all groups), and 97.00 ± 6.71% at week 5 (p < 0.001 vs all groups). At week 6, autologous
cell-treated wounds showed significantly greater percentage of re-epithelialization than both untreated and matrix-treated wounds (98.57 ± 3.50%, p < 0.05), but this was not significantly
different to allogeneic cell-treated wounds (92.11 ± 6.17%). Similar to the wound closure data, from this point onwards, autologous cell-treated wounds showed complete wound closure and
re-epithelialization and other treatments trended in this direction, with no statistical differences between groups. These data show that bioprinting autologous cells to full thickness
wounds resulted in rapid epithelialization of the wounds, representing a 4–5 week acceleration in wound re-epithelialization compared to other treatments. PORCINE WOUND HISTOLOGICAL ANALYSES
Microscopic examination identified increasing degrees of tissue regeneration, epithelialization and maturation as wound healing progressed through the weeks (Fig. 4). All wounds progressed
through an initial formation of granulation tissue on the surface followed by a thin discontinuous layer of squamous epithelium that eventually became continuous and covered the entire
wound. Wounds receiving bioprinted autologous cells showed early epithelialization with almost complete coverage of the wound at 2 weeks. By week 4, autologous bioprinted wounds showed the
formation of rete peg epithelial projections into the dermis, as well as the presence of keratinized stratified squamous epithelium. In contrast, allogeneic cell and matrix-treated wounds
did not show the presence of epithelialization or keratinized stratified squamous epithelium until week 6. Untreated wound healing appeared even more delayed, with only an immature
epithelium present at week 6, which still lacked the mature-appearing rete peg epithelial projections and keratinized stratified squamous epithelium at week 8. Wounds treated with bioprinted
autologous cells showed early formation of a loosely organized papillary layer above a denser, thicker layer of reticular dermis. The papillary dermis appeared to consist of coarse bundles
of larger loose fibers arranged parallel to the epidermis, while the reticular dermis contained larger blood vessels and closely interlaced smaller fibers. The structure of the tissue
appeared mature and complete at 8 weeks with nicely woven dermal collagen and regularly distributed vasculature. Allogeneic cell and matrix-treated wounds showed the continued presence of
granulation tissue 2 weeks after treatment, progressing to a dermis consisting of a densely packed fibroblastic proliferation lacking distinction between the papillary and reticular dermal
layers at week 4. By weeks 6 and 8 the dermis in these groups appeared similar to the autologous cell-treated group in appearance, matching the wound healing progression time frame observed
for the epidermis. Untreated wounds generally lacked the granulation tissue formation observed histologically for other groups, showing only a densely packed dermis and lacking blood vessel
formation. This continued until week 6, where the dermis matured at a similar, but slower progression than seen with other groups. It is well known that the more prolonged the inflammatory
phase of wound healing is, there is more likelihood of generating a non-functional scar. Therefore, we focused on assessing the degree and types of inflammation histologically. A pathologist
blinded to the treatment groups scored acute and chronic inflammation in H&E stained sections using the grading criteria shown in Supplementary Fig. S2. Acute inflammation was most
abundant in week 2 samples of all groups and decreased over the wound healing progression (Table 1). Acute inflammation was mostly superficial and appeared to be inversely related to the
degree of epithelialization. It was very prominent in all groups at 2 weeks (score of 3) except for the autologous cell-treated wounds, which only showed mild acute inflammation (score of
1). Acute inflammation was mostly absent or very mild by the 8th week in all groups. Chronic inflammation was present in all wounds and it was mainly in the deeper aspects of the wound. It
persisted throughout the study duration and did not appear to affect maturation and re-epithelialization of the wound. Granulomatous inflammation and foreign body giant cells were noted in
the deeper aspects in some of the grafts with no noticeable association with any specific treatment type. To evaluate the formation and maturation of wound vasculature, CD31 immuno-staining
was performed at weeks 4 and 8 of wound regeneration (Fig. 5A). Concurring with our observations of early granulation tissue formation in the autologous cell-treated wounds, we identified a
higher density of CD31-positive blood vessels throughout the dermis of these wounds, with only minimal, small blood vessels sparsely distributed throughout the dermis of the other groups. By
week 8, the overall number of small blood vessels appeared to decrease in autologous cell-treated wounds, and instead we observed larger mature vessels throughout the dermis. In contrast,
untreated wounds showed large numbers of small, immature blood vessels, suggesting that these tissues were undergoing delayed wound healing, appearing similar to autologous cell-treated
wounds at week 4. Matrix and allogeneic cell-treated wounds lacked the high density of small blood vessels observed in the week 4 autologous, and week 8 untreated wounds, and instead showed
a reduced number of mature blood vessels. Masson’s trichrome staining of tissue sections at week 4 highlighted a dermis composition with densely packed nuclei, potentially due to
inflammatory cells, and generally lacking organized collagen fibers (Fig. 5B). This was most prominent in the untreated and matrix treated groups. Allogeneic and autologous cell-treated
groups showed more diffuse nuclei distributed in a background of organized collagen fibers. At week 8, the concentration of cell nuclei was significantly reduced in all groups, however
patches of concentrated cells were still present in the dermis of the untreated, matrix-treated and allogeneic cell-treated groups. These were still present but fewer in number in autologous
cell-treated groups. Blue stained collagen fibers were most prominent in matrix-treated and autologous cell-treated wounds. Interestingly this was not observed to the same extent in
allogeneic cell-treated wounds. Collagen fibers present in the autologous cell-treated wounds appeared much larger and organized than observed in other groups, supporting histological
observations that the dermis of these wounds appeared more mature than for other treatments. Fibroblastic differentiation into myofibroblasts plays a major role in the formation of wound
granulation tissue early in wound healing, and persists in contractile wounds, such as hypertrophic scars. To evaluate the presence of myofibroblasts in the healing wounds, we performed
immuno-histochemistry for α-smooth muscle actin (αSMA) at weeks 4 and 8 (Fig. 5C). αSMA-positive cells were largely absent from untreated and matrix-treated wounds at week 4, while the
allogeneic and autologous cell-treated wounds showed moderate staining in the papillary region of the dermis. This staining was more prominent in the autologous cell-treated wounds. At week
8, the untreated and matrix-treated wounds showed significantly greater numbers of αSMA-positive cells, distributed throughout the dermis, and surrounding the sparse blood vessels,
suggesting the presence of large numbers of contractile myofibroblasts at this time-point. In the allogeneic and autologous cell-treated wounds, αSMA staining was primarily located around
the larger mature blood vessels, supporting observations of increased blood vessel formation and maturation in these tissues. Ki67 immuno-staining was performed at weeks 4 and 8 to evaluate
the presence of proliferating cells within the wounds (Fig. 5D). At week 4, untreated, matrix and allogeneic cell-treated wounds showed the greatest number of proliferating cells, primarily
located throughout the dermis, potentially activated myofibroblasts, and at the wound surface, which had not yet formed an immature epidermis. Autologous cell-treated wounds showed fewer
overall proliferating cells at week 4, however these cells were mostly present immediately underlying the developing epidermis, suggesting that rather than proliferating myofibroblasts,
these cells were keratinocytes contributing to epidermis formation and maturation. At week 8, the untreated, matrix and allogeneic cell-treated wounds showed a similar staining pattern to
that observed in the week 4 autologous cell-treated wounds, while the week 8 autologous cell-treated wounds showed an even greater number of proliferating cells in the underlying epidermis
area. SKIN BIOPRINTING COMPARISON WITH CELL SPRAYING We evaluated the efficacy of our bioprinting technique and compared to a cell spraying technique, which is becoming commonly applied in
the clinic for treatment of wounds using autologous skin cells. Specifically, we compared our _in situ_ skin bioprinting system using the printing parameters described above, to the FibriJet
biomaterial delivery device using the same materials, concentrations, volumes and application timing for both techniques. Similar to our previous studies, both groups formed granulation
tissue by 2 weeks followed by rapid wound closure through a combination of contraction and re-epithelialization, resulting in total wound closure (Supplementary Fig. S3A). Although the
bioprinted wounds appeared to show more rapid wound closure, reduced contraction and increased re-epithelialization, there were no statistical differences for these parameters at any
time-points (data not shown). This suggests that for these parameters, our bioprinting system is equally as effective as the currently available clinical cell spraying technologies.
Interestingly, histological analysis of the wounds at each time-point showed that the bioprinted wounds resulted in earlier epithelialization with almost complete wound coverage at 2 weeks,
while the cell sprayed wounds did not show the formation of epidermis until week 4 (Supplementary Fig. S3B). In fact, the epidermis of the cell spray groups did not thicken and showed signs
of maturation such as presence of keratinized stratified squamous epithelium until 6 weeks. Wounds treated with the bioprinted cells showed early formation of a papillary layer consisting of
coarse bundles of larger loose fibers, distinct from a dense, thicker layer of reticular dermis containing larger blood vessels and closely interlaced smaller fibers. In contrast, wounds
treated with the sprayed cells showed a dermis consisting of a densely packed organization lacking a distinction between the papillary and reticular dermal layers at week 2, which eventually
matured to form a more distinct and mature dermis similar to bioprinted wounds by week 4. Trichrome staining supported these observations, confirming that the bioprinted wounds showed
accelerated formation of epidermis and more mature dermis tissue at weeks (Supplementary Fig. S3C). Collagen fibers stained in blue were more prominent in the bioprinted wounds at week 4,
compared to wounds treated with the sprayed cells. By week 6, both groups had similar appearance with a defined epidermis and organized dermis, consisting of aligned collagen fibers.
DISCUSSION This study describes the proof-of-concept validation of a mobile _in situ_ skin bioprinting system with integrated imaging technology to provide rapid on-site management of full
thickness wounds. We found that treatment with autologous fibroblasts and keratinocytes, delivered directly to specific locations of the wound based on wound size and topology, resulted in
the acceleration of wound healing and the formation of normal skin _in situ_. Other groups have similarly demonstrated that bioprinting can be a useful tool for the fabrication of skin
tissue substitutes for wound healing. Lee _et al_. demonstrated the use of a solid freeform robotic system with noncontact dispensers capable of distributing keratinocytes and fibroblasts at
a high cell density at high resolutions30. This bioprinted skin tissue was morphologically and biologically representative of native human skin tissue. Another group used the laser-assisted
bioprinting to fabricate a 3D arrangement of fibroblasts and keratinocytes as a multicellular graft analogous to native skin archetype31. These skin constructs appeared to demonstrate
tissue formation following implantation into a nude mouse model32. Yet, another group has developed a modified extrusion bioprinter to deposit a combination of human plasma, human
fibroblasts, calcium chloride and human keratinocytes. The bioprinted construct was polymerized and grafted onto immunodeficient mice for up to eight weeks after which it was
indistinguishable from bilayered dermo-epidermal equivalents33. Our bioprinter system has combined an inkjet based bioprinter technology capable of rapidly depositing materials and cells
with high precision, with wound scanning imaging technology to specifically measure wound topology, and allow the precise and accurate delivery of appropriate cell types to specific areas of
the wound represents a significant advance in personalized wound treatment approaches. In this study, we first performed proof-of-concept studies using the murine model to demonstrate our
system was able to provide immediate and proper coverage of wounds. We then demonstrated the capabilities of our system to deliver allogeneic or autologous dermal fibroblasts and epidermal
keratinocytes within a biological hydrogel to large full thickness wound in the porcine model. Wound treatment using our bioprinting system resulted in the quick and proper coverage of the
wounds, which is crucial for maintaining homeostasis, wound closure, epithelialization and scar prevention. We demonstrated a proof-of-concept of our system by printing a bilayered skin
construct consisting of human fibroblasts and keratinocytes directly onto a full-thickness skin defect on a nude mouse. These studies demonstrated the capabilities of our bioprinting system
to deliver appropriate cell types and concentrations in a layered manner. Evaluation of the wound area over a 6-week period showed rapid closure of the wound in the printed mice compared to
the untreated and matrix controls. Although murine wound healing studies represented a cost-effective and rapid proof-of-concept for our skin bioprinting system, significant differences in
murine and human skin healing rates and mechanisms necessitated a more suitable porcine wound model for further evaluation. In our porcine studies, wounds treated with autologous fibroblasts
and keratinocytes performed better in every outcome evaluated. Autologous cell-treated wounds showed accelerated wound closure, reduced wound contraction and increased re-epithelialization.
These wounds also showed an acceleration of health skin formation and maturation, with histological evaluation showing increased formation of granulation tissue followed by the development
and maturation of a complete epidermis. Pathologic examination correlated very well with gross appearance of the wounds, with rapid formation of new epithelium. It also reinforced the common
understanding that granulation tissue formation is an essential first step in wound healing [30]. These tissues showed a dermal structure and composition similar to healthy skin, with
extensive collagen deposition arranged in large, organized fibers, extensive mature vascular formation and high numbers of proliferating keratinocytes. These factors all support the
conclusion that this treatment results in the acceleration of wound healing through the formation of healthy and functional skin _in situ_. These effects were not observed for the other
treatment groups, with matrix only-treated wounds and allogeneic cell-treated wounds appearing similar to untreated wounds. While some minor differences were observed for some outcome
measures, such as formation of granulation tissue and dermal collagen deposition, these differences did not seem to significantly impact wound healing or skin development. Based on these
findings, it appears that the biomaterials used to deliver cells to the wound did not contribute, negatively or positively, to wound development. Similarly, the inclusion of allogeneic cells
did not appear to provide any benefit to wound closure or healing. While this is not unexpected, as eventual rejection of cells is likely to occur in immune-competent animals, it does
highlight a limitation of this method for treating patients with skin burns or wounds covering the majority of the body, and where biopsy sites may not be available. Additionally, while a
short period of culture and expansion of autologous cells has been shown to be advantageous for wound healing applications21, many wounds require rapid treatment which may prevent the
ability to culture the isolated cells, reducing cell number and efficacy of the treatment. This is of key importance, as our preliminary studies suggests that wound healing time is directly
proportional to the number of autologous cell delivered to the wound (unpublished data). Strategies to overcome this limitation may include the development of HLA-matched skin cell banks,
the use of stem cells with potential immune-privileged status, or novel methods to increase cell isolation efficiency and functional activation prior to printing. This study was mainly
focused on the rate of wound healing and the ability to cover large wound areas. The efficacy of our bioprinting technique was compared to a cell spraying technique commonly used in the
clinic, where cells are retrieved from a blend of autologous tissues and sprayed as a mixture. Other than the different methods by which the materials and cells are delivered to the wounds,
the main difference between these two techniques is that the bioprinting approach delivers epidermal and dermal cells that are dispensed separately in a layer-by-layer fashion, rather than
an unorganized mixture of both cell types. We acknowledge that a common clinical application of cell spraying often involves the delivery of autologous cells without culture expansion in a
point-of-care clinical setting, however in order to facilitate a direct comparison of the bioprinting and cell spraying, we used culture expanded cells as used in previous bioprinting
studies, as well as maintained identical biomaterial and cell concentration, volumes and treatment protocols. In this comparative study, we did not observe significant differences between
the two techniques in regard to measurements of wound closure, contraction or re-epithelialization. The bioprinted wounds appeared to show accelerated closure, increased epithelialization
and reduced contraction. However, where we observed noticeable differences was in the early formation of a defined epidermis and mature dermis layers. This observation may be explained by
one or more influencing factors. First, it is likely that the cell-spraying device may have exposed cells to an instant, high-pressure and flow rate at the spray nozzle, negatively affecting
their viability and function. A more likely explanation for this observation is that the _in situ_ bioprinting system enables the dermal fibroblasts and epidermal keratinocytes to be
dispensed in a spatial orientation that matches the architecture of the wound. Such a system may provide multiple layers with more cell types specific to each skin level (epidermis, dermis,
fatty subcutis, hypodermis) to promote integration and formation of vascular and neural networks for the regeneration of functional skin. Further studies are necessary to elucidate the
reasons for these observed differences, however these data suggest that our skin bioprinting technology has the potential to improve wound treatments compared to currently used cell delivery
technologies. The duration of the study does not allow for assessment of long-term skin function and cosmetic results. However, given the significantly reduced wound contraction and the
histomorphologic evidence of well-organized tissue with proper vascularity and limited inflammation, we would expect reasonable cosmetic results on the long term. Additionally, the short
time-period for cell isolation and culture limited our ability to perform suitable cell tracking experiments. Lentivirus-labeling of isolated primary cells with a long-lasting fluorophore
was not feasible due to the need for selection of labeled cells, which would further decrease cell yield. The use of membrane-bound fluorescent dyes were found to fade rapidly due to _in
situ_ cell proliferation, limiting their usefulness for the 8 week time course of this experiment. Unfortunately, these limitations do not allow us to conclusively determine whether
bioprinted cells were cleared from the wounds, or what proportion of the regenerated skin consist of bioprinted cells. However, it is clear from these studies that _in situ_ bioprinting of
autologous cells resulted in the rapid formation of new skin, preventing contraction and accelerating the formation of healthy tissue structure and function. Our future studies will utilize
this printing system to investigate the delivery of other biomaterials and cell types to further accelerate wound healing, reduce the requirement for biopsies and cell culture, and
potentially provide an off-the-shelf cartridge that can be used to rapidly treat patients either whether they are in civilian hospitals or military field hospitals. The inclusion of
additional skin cell types is currently being evaluated, with the inclusion of melanocytes, adipose cells, and hair follicle cells promising to provide the rapid formation of skin tissue
with superior functional and cosmetic outcomes. This technology has a wide application, and its application will be expanded to not only treat full-thickness wounds, but also for other types
of wounds such as burns and ulcers, and even for deep tissue injuries. MATERIALS AND METHODS EXPERIMENTAL DESIGN This study was designed as a controlled laboratory experiment for the
proof-of-concept validation of a mobile _in situ_ skin bioprinting system with integrated imaging technology to provide rapid on-site management of full thickness wounds. Sample sizes for
each of the experiments were calculated using power analysis to ensure appropriate study power for our anticipated differences in means and standard deviations. For mouse studies 36 female
outbred athymic nude (Nu/nu) mice, divided into three groups of 12 animals in each treatment group (n = 4 per time-point). For porcine studies, six animals were used for the bioprinting
study (n = 6 per treatment). Data collection was performed at predetermined time-points as described below. Outliers were defined as data-points that were greater than two standard
deviations from the mean, and none were identified in these studies. Study endpoints were defined prior to study commencement and included improved wound closure, re-epithelialization and
contraction as primary endpoints, and healthy, mature skin formation as determined by histology as a secondary endpoint. MATERIALS Fibrinogen from bovine plasma Type I-S, 65–85% protein
(≥75% of protein is clottable) and thrombin from bovine plasma lyophilized powder, 40–300 NIH units/mg protein were purchased from Sigma Aldrich (St. Louis, MO). Collagen I from rat-tail was
purchased from BD Biosciences (San Jose, CA). All other reagents were of chemical grade. MURINE WOUND CREATION, BIOPRINTING, AND BANDAGING The efficacy of the skin delivery system prototype
to deliver viable skin cells directly onto wounds and replace the missing dermis and epidermis was evaluated by creating a 3 × 2.5 cm (L × W) full-thickness excisional skin defect on the
dorsa of 36 female outbred athymic nude (Nu/nu) mice (Charles River Laboratories, Wilmington, MA). This study and all animal procedures were performed according to the protocols approved by
the Wake Forest University Health Sciences Animal Care and Use Committee. All experiments were performed in accordance with Animal Care and Use Committee guidelines and regulations. The skin
was cleaned with iodine and then sterilized with alcohol swaps. The borders of the wounds were marked on the back of the mouse using sterile marker and ruler. The skin was removed
surgically using surgical scalpel blade and defect represents a wound of approximately 50% skin surface area on each mouse. Mice were divided into three groups of 12 animals in each
treatment group, with each group euthanized for evaluation at either 1 week, 3 weeks or 6 weeks (n = 4). The first group received no treatment and only standard wound dressing was applied to
cover the wounds (untreated), the second group received fibrin and collagen solution alone (matrix), and the third group was treated by printing a layer of human fibroblasts followed by
another layer of human keratinocytes (printed). The hydrogel carrier consists of a mixture of 25 mg/ml fibrinogen and 1.1 mg/ml collagen. The pH was adjusted to 7.2 and the solution was
syringe filtered using 0.2 µm filter. For the matrix group, the first layer was constructed by printing 0.5 ml of fibrinogen/collagen solution without cells followed immediately by printing
0.5 ml of 20 IU/mL thrombin (extracted from bovine plasma, Sigma Aldrich, St. Louis, MO) to crosslink the fibrinogen and form a fibrin gel. The thrombin was allowed to react before a second
layer was printed in the same fashion. Drops were printed at 1 mm interval. For the printed group, 1.875 × 106 fibroblasts were suspended in 0.5 mL of fibrinogen/collagen solution and
printed directly onto the wound followed by printing of an equal amount of thrombin. After 15 minutes, 3.75 × 106 keratinocytes suspended in 0.5 mL of fibrinogen/collagen solution was
printed on the top of the fibroblast layer. Equal amount of thrombin was printed to form a gel layer. Fibroblasts and keratinocytes were printed at 1:2 cell ratio to mimic the cellular
density of in the dermis and the epidermis in the native human skin. After printing of every layer, any remaining cell residue in the printing system was flushed out with water and the
system was sterilized using ethanol. Each wound from the three was bandaged by applying triple antibiotic ointment and covered with sterile gauze and surgical tape to prevent bandage damage
by the mouse. Dressing was changed every 3 days or as needed under isoflurane anesthesia. Animals were monitored for 6 weeks. MURINE WOUND ANALYSES Gross photographic images of wounds were
taken every week for 6 weeks. Pictures were taken using digital Kodak camera with 8.2 megapixel lens and a sterile ruler. Wound size measurements were evaluated from these pictures using
ImageJ software (National Institute of Health). Wound size was measured by using ImageJ to determine the area of open wound and expressed as percentage of the original wound size. Skin
samples retrieved from the mice were fixed in 10% phosphate-buffered formalin overnight at room temperature. Samples were dehydrated in a graded series of ethanol concentrations, embedded in
paraffin, and cut into 5 µm sections. Anti-human nuclear antigen slides were washed using buffer consisting of 0.1% saponin in PBS. These slides were incubated in a 1:40 dilution of primary
antibody with 0.1% saponin for 60 minutes followed by incubation in a 1:200 dilution of biotin-conjugated horse anti-mouse IgG secondary antibody with 0.1% saponin for 30 minutes. Biotin
was labeled with horseradish peroxidase/streptavidin for 30 minutes and visualized with NovaRed. Masson’s trichrome staining was performed to evaluate presence of muscle, collagen fibers,
fibrin, and erythrocytes. Briefly, slides were brought to water before submersion in Bouin’s solution, 60 °C for 1 hour, and then Weigert’s hematoxylin for 10 minutes. Sections were then
stained for 5 minutes in Biebrich scarlet, rinsed in distilled water and placed in phosphotungstic/phosphomolybdic acid for 10 minutes. Sections were then directly transferred into Aniline
blue for 5 minutes, rinsed and then 1% Acetic acid for 1 minute before dehydrating, clearing and cover slipping. PORCINE FULL-THICKNESS EXCISIONAL WOUND CREATION, AND BIOPRINTING Specific
Pathogen Free (SPF) Yorkshire pigs weighed approximately 40–50 kg at the start of each study. This study and all animal procedures were performed according to the protocols approved by the
Wake Forest University Health Sciences Animal Care and Use Committee. All experiments were performed in accordance with Animal Care and Use Committee guidelines and regulations. Six animals
were used for the bioprinting study. Animals were sedated with 0.05 mg/kg IM dexmedetomidine and maintained on inhaled isoflurane. They received SC bupivicaine at each wound site.
Post-operative analgesics included a transdermal fentanyl patch, famotidine (0.5 mg/kg PO), and carprofen (4 mg/kg PO) for three days. The anesthetized pigs had their backs depilated by
shaving. The animals were tattooed with four 10 × 10 cm tattoos on the dorsum to denote the area of the excisional wound. The dorsal skin was cleaned and sterilized with β-iodine and 70%
alcohol. For the creation of the defect, 4 areas of skin wound were created by removing 10 × 10 cm of full thickness skin in the central back along the thoracic and lumbar area. Incisions
were made along the wound edges with a surgical blade to the panniculus carnosus layer and the overlying skin was excised. After wounds were excised, 10 million fibroblasts were mixed with 6
ml of the fibrinogen/collagen solution as described above and loaded to the skin bioprinter. Thrombin was printed on the top of fibrinogen/collagen solution to form a gel layer. A second
layer of keratinocytes was printed on the top of the first layer in the same fashion. Allogeneic fibroblasts and keratinocytes were printed on one wound. Autologous fibroblasts and
keratinocytes were printed on a second wound. For matrix only wounds, a total of 12 ml of fibrinogen/collagen solution without cells was printed in two layers in the same fashion described
above. One wound remained untreated other than standard bandaging practices used for all wounds. GROSS EVALUATION OF PORCINE WOUND HEALING Gross photographic images of wound were taken every
week for 8 weeks. Pictures were taken using digital Kodak camera with 8.2 megapixel lens and a sterile ruler. Wound size, contracture and re-epithelialization measurements were evaluated
from these pictures using ImageJ software (National Institute of Health). Wound size and epithelialization was measured by using ImageJ to determine the area of open wound, and epithelium,
which was identified by color and texture of the healing wound. Generally open wounds were dark red and shiny, and epithelium ranged from light red and opaque/matte (due to a thin epidermis
covering) to white/pink and opaque/matte (due to thicker, mature epidermis). Areas of the wound biopsied for histological analysis were excluded from image analysis, and corrected in total
area calculations. Wound size was expressed as percentage of the original wound size and wound re-epithelialization was expressed as percentage of re-epithelialized area compared to the
total remaining wound size. Contraction was measured at each of the time-points by measuring the area inside the tattooed square using the software ImageJ and expressed relative to original
tattoo size. Wound contraction as expressed as percentage of the original tattoo size. PORCINE HISTOLOGICAL ANALYSES Five-millimeter full thickness punch biopsies were taken from the center
and the edge of every treatment wound at week 2, 4, 6 and 8 of the study to evaluate wound healing and skin reconstruction. Skin biopsies skin tissues fixed overnight in 10% neutral buffered
formalin. Biopsies were then washed in PBS 3 times for 30 minutes per wash, after which the samples were transferred to 30% sucrose for an overnight incubation at 4 °C. Biopsies were then
sliced in half, with half processed for paraffin embedding and half flash frozen in OCT blocks in liquid nitrogen. A cryotome or microtome (Leica) was used to generate 4–6 µm sections
comprised of the both center and edge portions of the regenerating wounds. Sections were stained with hematoxylin and eosin for histology, and slides were imaged under light microscopy.
Examination criteria included degree of epidermal formation and extent of epithelialization, dermal organization, evaluation of acute and chronic inflammation. Inflammation was evaluated by
a pathologist blinded to the treatment groups, using a scale to describe specific levels of acute and chronic inflammation. Masson’s trichrome staining was performed to evaluate presence of
muscle/keratin, collagen fibers, and nucleated cells. Briefly, slides were brought to water before submersion in Bouin’s solution, 60 °C for 1 hour, and then Weigert’s hematoxylin for 10
minutes. Sections were then stained for 5 minutes in Biebrich scarlet, rinsed in distilled water and placed in phosphotungstic/phosphomolybdic acid for 10 minutes. Sections were then
directly transferred into Aniline blue for 5 minutes, rinsed and then 1% Acetic acid for 1 minute before dehydrating, clearing and cover slipping. Immunohistochemical (IHC) staining for
CD31, α-smooth muscle actin (αSMA) and Ki67 was performed to assess vascularization, myofibroblast differentiation and cellular proliferation, respectively. For IHC, all incubations were
carried out at room temperature unless otherwise stated. Slides were warmed at 60 °C for 1 hr to increase bonding to the slides. Antigen retrieval was performed on all slides and achieved
with incubation in Proteinase K (Dako, Carpinteria, CA) for 5 min. Sections were permeabilized by incubation in 0.1% Triton-X for 5 min. Non-specific antibody binding was blocked by
incubation in Protein Block Solution (Abcam) for 15 min. Sections were incubated for 60 min in a humidified chamber with the primary antibodies CD31/PECAM-1 (1:200, Cat. # MAB33871, R&D
Systems), αSMA (1:100, Cat. # ab5694, Abcam), or Ki67 (1:100, Cat. # ab833, Abcam) in antibody diluent (Abcam). Following primary incubation, slides were washed 3 times in PBS for 5 min.
Sections were then incubated for 60 min with a biotinylated secondary antibody and peroxidase-labeled streptavidin (LSAB+ System HRP, Dako, Denmark). Stained cells were visualized using the
liquid DAB substrate with hematoxylin counterstain. STATISTICAL ANALYSES Statistical analysis of wound healing data was performed using GraphPad Prism and involved a two-way ANOVA with
comparisons between each treatment with each time-point. For multiple comparisons, a Tukey test was used and a significance and confidence interval of 0.05 and 95% respectively. All data is
presented as mean ± standard deviation (n = 4 for mouse studies and n = 6 for porcine studies). DATA AND MATERIALS AVAILABILITY All materials and reagents are listed in the Supplementary
Materials. Further inquiries should be directed to the corresponding author at [email protected]. REFERENCES * Beckrich, K. & Aronovitch, S. A. Hospital-acquired pressure ulcers: a
comparison of costs in medical vs. surgical patients. _Nurs Econ_ 17, 263–271 (1999). CAS PubMed Google Scholar * Brigham, P. A. & McLoughlin, E. Burn incidence and medical care use
in the United States: estimates, trends, and data sources. _J Burn Care Rehabil_ 17, 95–107 (1996). Article CAS Google Scholar * Miller, S. F. _et al_. National burn repository 2007
report: a synopsis of the 2007 call for data. _J Burn Care Res_ 29, 862–870, discussion 871 (2008). * Thomas, S. J., Kramer, G. C. & Herndon, D. N. Burns: military options and tactical
solutions. _J Trauma_ 54, S207–218 (2003). PubMed Google Scholar * Jones, I., Currie, L. & Martin, R. A guide to biological skin substitutes. _Br J Plast Surg_ 55, 185–193 (2002).
Article CAS Google Scholar * Morrow, T. Wound healing promoted with living-skin substitutes. _Manag Care_ 13, 62–63 (2004). PubMed Google Scholar * Gerding, R. L. _et al_. Outpatient
management of partial-thickness burns: Biobrane versus 1% silver sulfadiazine. _Ann Emerg Med_ 19, 121–124 (1990). Article CAS Google Scholar * Lal, S. _et al_. Biobrane improves wound
healing in burned children without increased risk of infection. _Shock_ 14, 314–318; discussion 318-319 (2000). * Lesher, A. P. _et al_. Effectiveness of Biobrane for treatment of
partial-thickness burns in children. _J Pediatr Surg_ 46, 1759–1763 (2011). Article Google Scholar * Purdue, G. F. _et al_. A multicenter clinical trial of a biosynthetic skin replacement,
Dermagraft-TC, compared with cryopreserved human cadaver skin for temporary coverage of excised burn wounds. _J Burn Care Rehabil_ 18, 52–57 (1997). Article CAS Google Scholar *
Heimbach, D. _et al_. Artificial dermis for major burns. A multi-center randomized clinical trial. _Ann Surg_ 208, 313–320 (1988). Article CAS Google Scholar * Wainwright, D. J. Use of an
acellular allograft dermal matrix (AlloDerm) in the management of full-thickness burns. _Burns: journal of the International Society for Burn Injuries_ 21, 243–248 (1995). Article CAS
Google Scholar * Hayes, D. W. Jr., Webb, G. E., Mandracchia, V. J. & John, K. J. Full-thickness burn of the foot: successful treatment with Apligraf. A case report. _Clin Podiatr Med
Surg_ 18, 179–188 (2001). PubMed Google Scholar * Waymack, P., Duff, R. G. & Sabolinski, M. The effect of a tissue engineered bilayered living skin analog, over meshed split-thickness
autografts on the healing of excised burn wounds. The Apligraf Burn Study Group. _Burns: journal of the International Society for Burn Injuries_ 26, 609–619 (2000). Article CAS Google
Scholar * Ho, C., Tran, K., Hux, M., Sibbald, G. & Campbell, K. Artificial skin grafts in chronic wound care: A meta-analysis of clinical efficacy and a review of cost-effectiveness
(2005). * Brem, H., Balledux, J., Bloom, T., Kerstein, M. D. & Hollier, L. Healing of diabetic foot ulcers and pressure ulcers with human skin equivalent: a new paradigm in wound
healing. _Arch Surg_ 135, 627–634 (2000). Article CAS Google Scholar * Normand, J. & Karasek, M. A. A method for the isolation and serial propagation of keratinocytes, endothelial
cells, and fibroblasts from a single punch biopsy of human skin. _In Vitro Cell Dev Biol Anim_ 31, 447–455 (1995). Article CAS Google Scholar * Hansbrough, J. F., Boyce, S. T., Cooper, M.
L. & Foreman, T. J. Burn wound closure with cultured autologous keratinocytes and fibroblasts attached to a collagen-glycosaminoglycan substrate. _JAMA_ 262, 2125–2130 (1989). Article
CAS Google Scholar * Kirsner, R. S. _et al_. Spray-applied cell therapy with human allogeneic fibroblasts and keratinocytes for the treatment of chronic venous leg ulcers: a phase 2,
multicentre, double-blind, randomised, placebo-controlled trial. _Lancet_ 380, 977–985 (2012). Article Google Scholar * Wood, F. M., Kolybaba, M. L. & Allen, P. The use of cultured
epithelial autograft in the treatment of major burn injuries: a critical review of the literature. _Burns: journal of the International Society for Burn Injuries_ 32, 395–401 (2006). Article
CAS Google Scholar * Butler, C. E., Yannas, I. V., Compton, C. C., Correia, C. A. & Orgill, D. P. Comparison of cultured and uncultured keratinocytes seeded into a collagen-GAG
matrix for skin replacements. _Br J Plast Surg_ 52, 127–132 (1999). Article CAS Google Scholar * Grinnell, F. Wound repair, keratinocyte activation and integrin modulation. _J Cell Sci_
101(Pt 1), 1–5 (1992). CAS PubMed Google Scholar * Sun, T. _et al_. Developments in xenobiotic-free culture of human keratinocytes for clinical use. _Wound Repair Regen_ 12, 626–634
(2004). Article Google Scholar * Navarro, F. A. _et al_. Sprayed keratinocyte suspensions accelerate epidermal coverage in a porcine microwound model. _J Burn Care Rehabil_ 21, 513–518
(2000). Article CAS Google Scholar * Gravante, G. _et al_. A randomized trial comparing ReCell system of epidermal cells delivery versus classic skin grafts for the treatment of deep
partial thickness burns. _Burns: journal of the International Society for Burn Injuries_ 33, 966–972 (2007). Article CAS Google Scholar * Murphy, S. V. & Atala, A. 3D bioprinting of
tissues and organs. _Nat Biotechnol_ 32, 773–785 (2014). Article CAS Google Scholar * Cui, X., Boland, T., D’Lima, D. D. & Lotz, M. K. Thermal inkjet printing in tissue engineering
and regenerative medicine. _Recent Pat Drug Deliv Formul_ 6, 149–155 (2012). Article CAS Google Scholar * Xu, T. _et al_. Complex heterogeneous tissue constructs containing multiple cell
types prepared by inkjet printing technology. _Biomaterials_ 34, 130–139 (2013). Article Google Scholar * Okamoto, T., Suzuki, T. & Yamamoto, N. Microarray fabrication with covalent
attachment of DNA using bubble jet technology. _Nat Biotechnol_ 18, 438–441 (2000). Article CAS Google Scholar * Lee, V. _et al_. Design and fabrication of human skin by three-dimensional
bioprinting. _Tissue Engineering Part C: Methods_ 20, 473–484 (2013). Article Google Scholar * Koch, L. _et al_. Skin tissue generation by laser cell printing. _Biotechnology and
bioengineering_ 109, 1855–1863 (2012). Article CAS Google Scholar * Michael, S. _et al_. Tissue engineered skin substitutes created by laser-assisted bioprinting form skin-like structures
in the dorsal skin fold chamber in mice. _PloS one_ 8, e57741 (2013). Article ADS CAS Google Scholar * Cubo, N., Garcia, M., del Cañizo, J. F., Velasco, D. & Jorcano, J. L. 3D
bioprinting of functional human skin: production and _in vivo_ analysis. _Biofabrication_ 9, 015006 (2016). Article ADS Google Scholar Download references ACKNOWLEDGEMENTS We would like
to thank the WFIRM surgical core facility, in particular Cara Clouse, Tammy Cockerham, Tiffany Bledsoe, Adam Wilson and Sandy Sink. We also thank Paul Robertson (Next Medical Design) and
Kevin Rackers, the contract developers of the printer. This research was funded by the Telemedicine and Advanced Technology Research Center and the Armed Forces Institute for Regenerative
Medicine. AUTHOR INFORMATION Author notes * Mohammed Albanna, Kyle W. Binder and Sean V. Murphy contributed equally. AUTHORS AND AFFILIATIONS * Wake Forest Institute for Regenerative
Medicine, Wake Forest School of Medicine, Medical Center Boulevard, Winston-Salem, NC, 27157, USA Mohammed Albanna, Kyle W. Binder, Sean V. Murphy, Jaehyun Kim, Weixin Zhao, Josh Tan, Idris
B. El-Amin, Dennis D. Dice, Julie Marco, Jason Green, Tao Xu, Aleksander Skardal, John D. Jackson, Anthony Atala & James J. Yoo * Department of Pathology, Wake Forest School of Medicine,
Medical Center Boulevard, Winston-Salem, NC, 27157, USA Shadi A. Qasem * Jiangsu Key Laboratory of Neuroregeneration, Nantong University, Nantong, China Weixin Zhao * Department of Surgery,
Wake Forest School of Medicine, Medical Center Boulevard, Winston-Salem, NC, 27157, USA James H. Holmes * Virginia Tech-Wake Forest School of Biomedical Engineering and Sciences, Wake
Forest School of Medicine, Winston-Salem, NC, 27157, USA Sean V. Murphy & Aleksander Skardal Authors * Mohammed Albanna View author publications You can also search for this author
inPubMed Google Scholar * Kyle W. Binder View author publications You can also search for this author inPubMed Google Scholar * Sean V. Murphy View author publications You can also search
for this author inPubMed Google Scholar * Jaehyun Kim View author publications You can also search for this author inPubMed Google Scholar * Shadi A. Qasem View author publications You can
also search for this author inPubMed Google Scholar * Weixin Zhao View author publications You can also search for this author inPubMed Google Scholar * Josh Tan View author publications You
can also search for this author inPubMed Google Scholar * Idris B. El-Amin View author publications You can also search for this author inPubMed Google Scholar * Dennis D. Dice View author
publications You can also search for this author inPubMed Google Scholar * Julie Marco View author publications You can also search for this author inPubMed Google Scholar * Jason Green View
author publications You can also search for this author inPubMed Google Scholar * Tao Xu View author publications You can also search for this author inPubMed Google Scholar * Aleksander
Skardal View author publications You can also search for this author inPubMed Google Scholar * James H. Holmes View author publications You can also search for this author inPubMed Google
Scholar * John D. Jackson View author publications You can also search for this author inPubMed Google Scholar * Anthony Atala View author publications You can also search for this author
inPubMed Google Scholar * James J. Yoo View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS S.V.M., M.A., K.W.B., J.K., J.D.J., A.A., J.J.Y.
Conception and design. S.V.M., M.A., K.W.B., J.K., J.M., J.G., S.A.Q., W.Z., J.T., I.B.E., D.D.D., J.M., J.G., E.A.G., T.X., A.S. Collection and/or assembly of data. S.V.M., M.A., K.W.B.,
J.K., S.A.Q., J.H.H., J.D.J., A.A., J.J.Y. Data analysis and interpretation. S.V.M., M.A., K.W.B., J.K., J.M., J.G., Manuscript writing and editing. S.V.M., M.A., K.W.B., J.K., S.A.Q., W.Z.,
J.T., I.B.E., D.D.D., A.S., J.H.H., J.D.J., A.A., J.J.Y. Final approval of manuscript. A.A., J.J.Y., Financial support. CORRESPONDING AUTHOR Correspondence to Sean V. Murphy. ETHICS
DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE: Springer Nature remains neutral with regard to jurisdictional claims in
published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY MATERIAL RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons
Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original
author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the
article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use
is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Albanna, M., Binder, K.W., Murphy, S.V. _et al._ _In Situ_ Bioprinting of
Autologous Skin Cells Accelerates Wound Healing of Extensive Excisional Full-Thickness Wounds. _Sci Rep_ 9, 1856 (2019). https://doi.org/10.1038/s41598-018-38366-w Download citation *
Received: 26 July 2018 * Accepted: 19 December 2018 * Published: 12 February 2019 * DOI: https://doi.org/10.1038/s41598-018-38366-w SHARE THIS ARTICLE Anyone you share the following link
with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt
content-sharing initiative