The size of spontaneous pneumothorax is a predictor of unsuccessful catheter drainage
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Small-bore thoracic catheter drainage is recommended for a first large or symptomatic episode of primary spontaneous pneumothorax (PSP). However, one-third of these patients require
a second procedure because of treatment failure. We investigated the factors associated with unsuccessful pigtail catheter drainage in the management of PSP. In this retrospective study,
using a prospectively collected database, we enrolled 253 consecutive patients with PSP who underwent pigtail catheter drainage as initial treatment, from December 2006 to June 2011. The
chest radiograph was reviewed in each case and pneumothorax size was estimated according to Light’s index. Other demographic factors and laboratory data were collected via chart review.
Pigtail catheter drainage was successful in 71.9% (182/253) of cases. Treatment failure rates were 42.9%, 25.9%, and 15.5% in patients with pneumothorax sizes of >62.6%, 38–62.6%, and
<38%, respectively (tertiles). An alternative cut-off point of 92.5% lung collapse was defined using a classification and regression tree method. According to the multivariate analysis, a
large-size pneumothorax (_p_ = 0.009) was the only significant predictor of initial pigtail catheter drainage treatment failure in patients with PSP. Early surgical treatment could be
considered for those patients with a large-sized pneumothorax. SIMILAR CONTENT BEING VIEWED BY OTHERS TRENDS IN RECURRENCE OF PRIMARY SPONTANEOUS PNEUMOTHORAX IN YOUNG POPULATION AFTER
TREATMENT FOR FIRST EPISODE BASED ON A NATIONWIDE POPULATION DATA Article Open access 18 August 2023 RECOMMENDATION FOR MANAGEMENT OF PATIENTS WITH THEIR FIRST EPISODE OF PRIMARY SPONTANEOUS
PNEUMOTHORAX, USING VIDEO-ASSISTED THORACOSCOPIC SURGERY OR CONSERVATIVE TREATMENT Article Open access 25 May 2021 THE UNNECESSARY WORKUPS AND ADMISSIONS OF ADOLESCENTS AND YOUNG ADULTS
WITH SPONTANEOUS PNEUMOMEDIASTINUM Article Open access 24 February 2024 INTRODUCTION Primary spontaneous pneumothorax (PSP) is defined as the trapping of air in the pleural cavity of
patients without underlying lung disease or thoracic trauma. PSP usually affects young and tall male patients, often adolescents with a slim build. The global incidence is 7.4–18/1,000,000
men per year and 1.2–6/1,000,000 women per year1, 2. The optimal treatment for patients presenting with a first episode of PSP is controversial and existing guidelines vary3,4,5. The British
Thoracic Society (BTS) 2010 pleural disease guidelines recommended needle aspiration (14–16 G) or small-bore (<14 French, 4.7-mm diameter) thoracic catheter drainage as the first-line
treatment for patients with a large PSP3. However, the results of simple aspiration are not satisfactory for a large portion of patients. First, the success rate of needle aspiration varies
widely in the literature, ranging from 38%–85%6,7,8,9,10,11,12,13,14,15; second, almost one-third of patients need an additional invasive procedure6. Therefore, several modified strategies,
including thoracostomy with chest tube or pigtail catheter, chemical pleurodesis with sclerosing agents, or video-assisted thoracic surgery are generally required16, 17. The issue of initial
treatment failure in PSP is important. An appropriately selected treatment strategy leads to a better outcome and less waste of medical resources. In some patients with a high risk of
treatment failure, physicians may choose a more efficient management approach than simple aspiration. Since 1985, several studies focused on this issue, and reported several factors
associated with treatment failure with simple aspiration. These factors included age >50 y, pre-existing lung disease, a large volume of aspiration, and pneumothorax size6, 10, 12, 18,
19. Harvey _et al._ reported a significant difference in the amount of air aspirated between successfully treated patients and those who showed treatment failure6. In a retrospective study
with 91 cases, Chan _et al._ reported that treatment was more likely to fail in patients with a large pneumothorax (>40%)10. However, these studies were limited by their retrospective
nature, small study populations (<100 cases), and heterogeneous patient populations. Furthermore, there have been no previous studies discussing the factors affecting initial treatment
failure after catheter drainage. The aim of our study was to investigate the risk factors associated with treatment failure of PSP treated with a small-bore (8-French) pigtail catheter for
thoracic drainage as the initial treatment based on a prospectively collected, single-center database in a large homogenous patient population. RESULTS CHARACTERISTICS OF PATIENTS From 2006
to 2011, a total of 253 patients were enrolled into the study and underwent trans-thoracic pigtail catheter insertion and drainage. Overall, 182 patients were successfully treated by this
method (71.9%; success group) and 71 patients were considered treatment failures (28.1%; failure group). The failure group included 60 cases with persistent air-leaks at 72 hours after the
procedure and 11 cases who showed an enlarging pneumothorax on serial chest radiographs after the pigtail catheter was removed. In these 11 cases, the catheters were all removed once there
were no ongoing air-leaks. Table 1 demonstrates the clinical features of the two groups. We carefully recorded every patient’s clinical data with a thorough chart review. Both groups were
composed of younger adults (mean age: 22.5 ± 5.5 y) with a slim body shape (body mass index [BMI] = 19.3 ± 2.3 kg/m2). A smoking history did not affect the outcome of treatment (_p_ =
0.641). In our study, more patients had a pneumothorax affecting the left side (147/253, 58.10%), but there was no significant difference in treatment outcome based on the side of the
pneumothorax (_p_ = 0.943). There were no significant differences in hemoglobin, white blood cell (WBC) count, and renal or hepatic function between the successfully treated patients and
those with treatment failure. SIZE OF PNEUMOTHORAX AND TREATMENT OUTCOMES In our study, the only factor that had a significant impact on the treatment outcome was the size of the
pneumothorax. The treatment failure group had a significantly larger-sized lung collapse than the successfully treated group (60 ± 0.23% vs. 51 ± 0.21%, _p_ = 0.004). Table 2 shows the
relationship between pneumothorax size and treatment outcome. We split the 253 patients into tertiles according to their initial pneumothorax size, as determined by chest radiography. Based
on these measurements, the size of the pneumothorax was classified into three categories based on the severity of lung collapse: massive (>62.6%), moderate (38–62.6%), and mild (<38%)
collapse. In patients with a mild collapse, the treatment success rate was 84.52%; while in patients with a massive collapse, the success rate was 57.15%. Further analysis revealed a trend
showing that, the larger the size of the lung collapse, the more likely it was that treatment would fail. We also created an alternative statistical model using the classification and
regression tree (CART) method. In this model, all patients were divided into two groups according to the cut-off point of 92.5% lung collapse. Table 3 shows the multivariate logistic
regression analysis of the risk factors. Massive collapse (>92.5%) was associated with a higher risk of treatment failure than in other cases, with an OR of 4.23 (95% confidence interval
= 1.43–12.47, _p_ = 0.0091). Other factors, including age, BMI, and smoking status were not associated risk factors. There were no major complications associated with the pigtail catheter
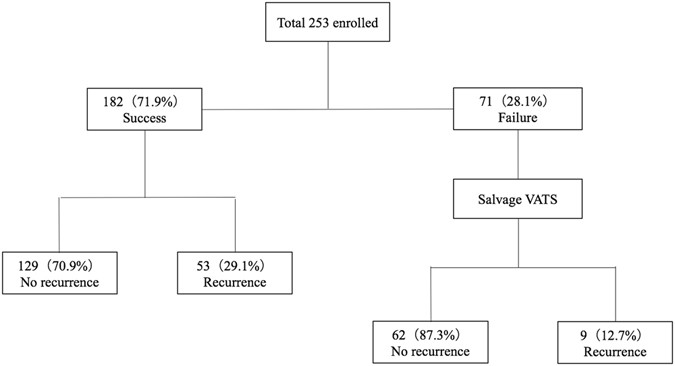
insertion, such as hemothorax, lung penetrating injury caused by the pigtail catheter, or other solid organ injury. LONG-TERM FOLLOW-UP OUTCOMES The long-term follow-up outcomes of the 253
patients were recorded after chart review and phone interview, with a mean follow-up period of 90.9 ± 14.6 (range: 60–114) months. Figure 1 summarizes the results of the long-term follow-up.
The recurrence rate in the success group was 29.1% (53/182 cases). The 71 patients with initial treatment failure underwent salvage video-assisted thoracoscopic surgery (VATS, described in
the Methods section). The recurrence rate of the patients who received salvage VATS was 12.7% (9/71 cases). Among the patients who underwent salvage VATS, pathological examination revealed
that 85.9% (61/71) had bullae, and 12.7% (9/71) had blebs. One case showed emphysematous changes without formation of bullae or blebs. DISCUSSION Pneumothorax remains a challenging disease
with a lack of optimal treatment guidelines, especially for those patients experiencing a first episode or “large”-sized pneumothorax. The currently available guidelines, including those set
out by the British Thoracic Society (BTS), the American College of Chest Physicians (ACCP), and the Belgian Society of Pulmonology (BSP), all differ in their recommendations for treatment
of a large-sized PSP3,4,5. The initial treatment strategies include conservative treatment, simple aspiration, and intercostal pleural drainage with a small-bore pigtail catheter or
traditional large-bore catheter3,4,5, 16, 17. Traditional conservative treatment includes bed rest, supplemental high flow oxygen, and analgesics. Both bed rest and high-flow oxygen
supplementation improve trans-thoracic air reabsorption20, 21. When conservative treatment fails, or is not suitable, invasive treatment, such as the placement of trans-thoracic drains
should be considered. Both the BTS and ACCP guidelines recommend simple aspiration or small-bore trans-thoracic drainage as the initial treatment for PSP3, 4. The role of trans-thoracic
drainage in PSP is to remove excess intrapleural air and promote apposition of the visceral and parietal pleura, initiating the process of healing of the lung defect. A retrospective study
by Chan _et al._ used a homogenous population of 91 PSP patients treated with simple aspiration, and revealed that treatment failure was associated with a pneumothorax with a size ≥40%10.
However, that study had several limitations, including its retrospective design, the lack of a universal protocol for estimating pneumothorax size, and a low rate of successful treatment
(50.5%). Our study is the largest study of patients undergoing initial PSP treatment to date, and is based on a prospectively collected, single-center database with a homogenous patient
population. We employed the Light index, which is an easily implemented method, for the estimation of pneumothorax size. Our study observed that a large-sized pneumothorax is the only factor
associated with treatment failure. Patients with a larger pneumothorax are more likely to experience treatment failure. We recommend trans-thoracic drainage with a small-sized
trans-thoracic pigtail catheter instead of simple aspiration in PSP patients with a small pneumothorax. We routinely connect the pigtail catheter to a water-sealed bottle, which acts as a
single-bottle underwater seal chest drainage system, thereby providing continuous trans-thoracic air drainage. The effect of drainage can be augmented with low-pressure negative suction
(usually −10 to −20 cmH2O)22. Patient safety is always a concern, and pigtail catheter insertion is easy to perform and less invasive than other procedures23. Additionally, unlike simple
aspiration, insertion of the pigtail catheter does not require repeat procedures. The complications of pigtail catheter insertion are few, especially in young and medically uncomplicated
populations24, 25. With continuous monitoring of the trans-thoracic space, we can monitor when air-leaking resolves and can respond immediately to any emergency conditions, such as a delayed
hemothorax. We acknowledge that there are limitations to this study. First, it is difficult to measure the pneumothorax volume accurately from chest radiographs, which are two-dimensional
images, because the pleural cavity is a three-dimensional structure. However, chest radiography is the most common and accessible method to diagnose PSP in most institutes. Therefore, we
decided to use chest radiography, rather than chest computed tomography, to estimate the size of the pneumothorax. On the other hand, this means that our findings might be helpful in
settings where computed tomography is not readily available. Second, because our institute lacked the appropriate equipment, we did not record the volume of the air-leaks in this study. A
large volume of aspirated air may be related to the size of the pneumothorax, and the BTS guidelines use 2.5 L as the limit for simple aspiration because of the likely presence of persistent
air leak. Finally, our study is a retrospective-based analysis similar to other existing literature. Further prospective randomized clinical trials with larger study populations are
necessary. We reported our experience with a large cohort of 253 PSP patients who underwent pigtail catheter drainage, and concluded that the size of the pneumothorax is the only prognostic
factor associated with treatment outcome in PSP. Trans-thoracic pigtail catheter drainage has several advantages over simple aspiration. In addition, with the advances in thoracoscopic
surgery over the past decade, VATS has become a safe intervention for PSP as the first-line surgical intervention or salvage strategy26,27,28. Early thoracoscopic procedures can be
considered as a first-line treatment for patients with a large pneumothorax. METHODS STUDY DESIGN AND PATIENTS This study was based on the retrospective analysis of a prospectively collected
database. From December 2006 through June 2011, a total of 253 patients with a diagnosis of primary pneumothorax matching the eligibility criteria (described in the next section) were
recorded in the database of the National Taiwan University Hospital, a university teaching hospital in Taipei, Taiwan. The enrolled patients were first treated with trans-thoracic drainage
by pigtail catheter. The trans-thoracic pigtail catheter (8-French, 2.67-mm diameter) was inserted into the side affected by the pneumothorax and patients were categorized into treatment
failure and treatment success groups. Treatment failure was defined by the two following conditions: (1) persistent air leaks 72 hours after the procedure or (2) an enlarging pneumothorax on
serial chest radiographs after pigtail catheter removal under the condition of no ongoing airleaks. Treatment success was defined as no detectable pneumothorax after the pigtail catheter
was removed and a disease-free status maintained for more than one month after catheter removal. Patient characteristics including age, gender, smoking status (current smokers and
ever-smokers were classified as “smokers”, and never-smokers were classified as “nonsmokers”), and side of the pneumothorax at initial assessment were recorded. Clinical parameters,
including hemoglobin, WBC count, and renal and hepatic function, were collected from the patient charts. The Research Ethics Committee of the National Taiwan University Hospital approved
this study. Written informed consent was obtained from all subjects before the procedure, and all procedures and methods were performed in accordance with relevant guidelines and
regulations. ELIGIBILITY CRITERIA Patients were considered eligible for inclusion in the study if: (1) they had their first episode of spontaneous pneumothorax, and (2) the first chest
radiograph after the episode revealed that the rim of air in the thorax was >2 cm, compatible with the definition of a large-sized PSP according to the BTS 2010 criteria3. Additional
inclusion criteria included age between 15 and 40 years, with adequate hematological function (hemoglobin >10 g/dL, absolute neutrophil count >1.5 × 109/L, and platelets >100 ×
109/L), and normal renal and hepatic functions (serum creatinine <1 × ULN, serum glutamic-pyruvic transaminase and serum glutamic-oxaloacetic transaminase <2.5 × the upper limits of
normal). Patients were excluded if they (1) had underlying pulmonary disease, such as a congenital anomaly or lung fibrosis, (2) had an emergency condition requiring chest tube thoracostomy
or surgical exploration, such as hemothorax or tension pneumothorax, (3) had a history of previous pneumothorax, (4) had a history of an ipsilateral thoracic operation, (5) were pregnant or
lactating, or (6) had a serious concomitant illness or medical condition. ESTIMATION OF PNEUMOTHORAX SIZE We carefully reviewed the first chest radiograph that confirmed the diagnosis of
pneumothorax in every patient. Chest radiographs were retrospectively reviewed by two of the principal investigators (T-M Tsai, M-W Lin, H-C Liao, and C-Y Liu). The investigators were
blinded to the patient outcomes, and their decision was recorded after they reached a consensus. We used the Light index25, a measurement modality generally accepted in Europe, for the
estimation of pneumothorax size. The Light index is based on the proportional relationship between the diameters of a collapsed lung and its hemithorax. The estimated pneumothorax percentage
= (1 − L3/H3) × 100; where H = hemithorax diameter and L = diameter of the collapsed lung (Fig. 2). INSERTION OF THE THORACIC PIGTAIL CATHETER Once the patient was enrolled, thoracic
drainage was immediately performed as follows. All procedures were performed by board-certified thoracic surgeons in our institute. Patients were first seated in a semi-supine position and,
after skin disinfection and field preparation, a small-bore pigtail catheter (8-French; Bioteque Corporation, I-Lan, Taiwan) was introduced into the first or second intercostal space, at the
midclavicular line, after providing local anesthesia with 2% lidocaine. After the catheter had entered the pleural space, it was fixed to the skin using sterile adhesive tape and connected
via a three-way valve to a 50-ml syringe. Air was manually aspirated until a resistance was felt and aspiration ceased. The pigtail catheter was then connected to a single-bottle
underwater-seal chest-drainage system: a rigid straw is inserted into a sterile chest bottle containing saline solution, with its tip 2-cm below the level of the solution, and the other end
of this rigid straw is connected to the pigtail catheter placed in the pleural cavity. Another rigid straw is inserted into the bottle and connected to a negative pressure suction (−10
cmH2O) device to control the drainage of the pleural cavity. Chest radiographs were obtained once before the procedure and daily after the procedure in all patients to assess treatment
results. OPERATIVE TECHNIQUES OF SALVAGE VATS VATS is a better modality than chest tube drainage for the management of unsuccessful aspiration of a PSP26. At our institution, the general
practical guidelines indicate salvage VATS for patients with recurrence or initial treatment failure of PSP. The procedure is performed in the standard fashion under general anesthesia with
double-lumen endotracheal tube intubation, with the patient in a lateral decubitus position with the ipsilateral lung deflated. We use three thoracoscopic ports: one 12-mm and two 3-mm in
diameter. A 10-mm 30-degree telescope (Karl Storz, Tuttlingen, Germany) is inserted through the 12-mm port at the 6th or 7th intercostal space, along the middle axillary line. The two 3-mm
ports are located in the 3rd or 4th intercostal space, at the anterior and posterior axillary line, respectively. The two 3-mm ports are used as working ports, allowing us to release the
pleural adhesions using electrocautery and identify the blebs. Once the blebs are identified, they are held with a 3-mm grasp, and excised with a 45-mm endoscopic stapler through the
inspection of another independent 3-mm 30-degree mini-telescope. If no blebs can be identified, blind apical stapling is done at the most suspicious area. To complete the mechanical
pleurodesis, the entire apical parietal surface is abraded by inserting a dissector with a diathermy scratch pad through the 12-mm port. Finally, a chest tube (28-French) is placed in the
apex area through the 12-mm port site. The surgical specimens are sent for routine pathological examination. STATISTICAL ANALYSIS The results were expressed as mean ± standard deviation for
continuous variables and frequency (%) for categorical variables. Differences between the failure group and the success group were compared with a two-sample _t_-test for continuous
variables, and with the chi-square test or Fisher’s exact test for dichotomous variables. Initially, we divided the patients into tertiles according to their initial pneumothorax size, and
performed a univariate analysis of the potential risk factors. To further test the robustness of our data, we created an alternative statistical model using the classification and regression
tree method. Using this model, we divided all the patients into two groups by a single cut-off point of lung collapse percentage (92.5%) and performed a multivariate logistic regression
analysis. The potential risk factors (_p_ < 0.05) in the univariate analysis and some potential clinical confounding factors were included in the multivariate logistic regression model.
All statistical analyses were performed using the SAS 9.4 and R 3.3.1 software. Statistical significance was set at _p_ < 0.05. REFERENCES * Melton, L. J. 3rd, Hepper, N. G. G. &
Offord, K. P. Incidence of spontaneous pneumothorax in Olmsted County, Minnesota: 1950 to 1974. _Am. Rev. Respir. Dis._ 120, 1379–1382 (1979). PubMed Google Scholar * Sahn, S. A. &
Heffner, J. E. Primary care: spontaneous pneumothorax. _N. Engl. J. Med._ 342, 868–874 (2000). Article CAS PubMed Google Scholar * MacDuff, A., Arnold, A. & Harvey, J., BTS Pleural
Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. _Thorax_ 65 (Supple 2), ii18–31 (2010). PubMed Google Scholar *
Baumann, M. H. _et al._ Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. _Chest_ 119, 590–602 (2001). Article CAS PubMed Google
Scholar * De Leyn, P. _et al._ Guidelines Belgian Society of Pulmonology: guidelines on the management of spontaneous pneumothorax. _Acta. Chir. Belg._ 105, 265–267 (2005). Article ADS
PubMed Google Scholar * Harvey, J. & Prescott, R. J. Simple aspiration versus intercostal tube drainage for spontaneous pneumothorax in patients with normal lungs. _Br. Med. J_ 309,
1338–1339 (1994). Article CAS Google Scholar * Andrivet, P., Djedaini, K., Teboul, J. L., Brouchard, L. & Dreyfuss, D. Spontaneous pneumothorax. Comparison of thoracic drainage vs
immediate or delayed needle aspiration. _Chest_ 108, 335–339 (1995). Article CAS PubMed Google Scholar * Kelly, A. M. Review of management of primary spontaneous pneumothorax: Is the
best evidence clearer 15 years on? _Emerg. Med. Australas_ 19, 303–308 (2007). Article PubMed Google Scholar * Packham, S. & Jaiswal, P. Spontaneous pneumothorax: use of aspiration
and outcomes of management by respiratory and general physicians. _Postgrad. Med. J._ 79, 345–7 (2003). Article CAS PubMed PubMed Central Google Scholar * Chan, S. S. & Lam, P. K.
Simple aspiration as initial treatment for primary spontaneous pneumothorax: results of 91 consecutive cases. _J. Emerg. Med._ 28, 133–138 (2005). Article PubMed Google Scholar * Mendis,
D., El-Shanawany, T., Mathur, A. & Redington, A. E. Management of spontaneous pneumothorax: are British Thoracic Society guidelines being followed? _Postgrad. Med. J._ 78, 80–84 (2002).
Article CAS PubMed PubMed Central Google Scholar * Ng, A. W., Chan, K. W. & Lee, S. K. Simple aspiration of pneumothorax. _Singapore Med. J._ 35, 50–52 (1994). CAS PubMed Google
Scholar * Markos, J., McConigle, P. & Phillips, M. J. Pneumothorax: treatment by small-lumen catheter aspiration. _Aust. NZ. J. Med_ 20, 775–781 (1990). Article CAS Google Scholar *
Noppen, M., Alexander, P., Driesen, P., Slabbynck, H. & Verstraiten, A. Manual aspiration versus chest tube drainage in first episodes of primary spontaneous pneumothorax: a multicenter,
prospective, randomized pilot study. _Am. J. Respir. Crit. Care Med._ 165, 1240–1244 (2002). Article PubMed Google Scholar * Ayed, A. K., Chandrasekaran, C. & Sukumar, M. Aspiration
versus tube drainage in primary spontaneous pneumothorax: a randomized study. _Eur. Respir. J._ 27, 477–482 (2006). Article CAS PubMed Google Scholar * Chen, J. S. _et al._ Intrapleural
minocycline following simple aspiration for initial treatment of primary spontaneous pneumothorax. _Respir. Med._ 102, 1004–1010 (2008). Article PubMed Google Scholar * Chen, J. S. _et
al._ Salvage for unsuccessful aspiration of primary pneumothorax: thoracoscopic surgery or chest tube drainage? _Ann. Thorac. Surg._ 85, 1908–1913 (2008). Article PubMed Google Scholar *
Archer, G. J., Hamilton, A. A., Upadhyay, R., Finlay, M. & Grace, P. M. Results of simple aspiration of pneumothoraces. _Br. J. Dis. Chest_ 79, 177–182 (1985). Article CAS PubMed
Google Scholar * Soulsby, T. British Thoracic Society guidelines for the management of spontaneous pneumothorax: do we comply with them and do they work? _J. Accid. Emerg. Med_ 15, 317–321
(1998). Article CAS PubMed PubMed Central Google Scholar * Kircher, L. T. Jr. & Swartzel, R. L. Spontaneous pneumothorax and its treatment. _J. Am. Med. Assoc_ 155, 24–29 (1954).
Article PubMed Google Scholar * Northfield, T. C. Oxygen therapy for spontaneous pneumothorax. _BMJ._ 4, 86–88 (1971). Article CAS PubMed PubMed Central Google Scholar * Munnell, E.
R. Thoracic drainage. _Ann. Thorac. Surg._ 63, 1497–1502 (1997). Article CAS PubMed Google Scholar * Chen, J. S. _et al._ Simple aspiration and drainage and intrapleural minocycline
pleurodesis versus simple aspiration and drainage for the initial treatment of primary spontaneous pneumothorax: an open-label, parallel-group, prospective, randomised, controlled trail.
_Lancet_ 381, 1277–1282 (2013). Article CAS PubMed Google Scholar * Vedam, H. & Barnes, D. J. Comparison of large- and small- bore intercostal catheters in the management of
spontaneous pneumothorax. _Intern. Med. J._ 33, 495–499 (2003). Article CAS PubMed Google Scholar * Akowuah, E. _et al._ Less pain with flexible fluted silicone chest drains than with
conventional rigid chest tubes after cardiac surgery. _J. Thorac. Cardiovasc. Surg._ 124, 1027–1028 (2002). Article PubMed Google Scholar * Chen, J. S. _et al._ Salvage for unsuccessful
aspiration of primary pneumothorax: thoracoscopic surgery or chest tube drainage? _Ann. Thorac. Surg._ 85, 1908–13 (2008). Article PubMed Google Scholar * Chang, Y. C. _et al._ Modified
needlescopic video-assisted thoracic surgery for primary spontaneous pneumothorax: The long-term effects of apical pleurectomy versus pleural abrasion. _Surg. Endosc._ 20, 757–762 (2006).
Article PubMed Google Scholar * Schramel, F. M. _et al._ Cost-effectiveness of video-assisted thoracoscopic surgery versus conservative treatment for first time or recurrent spontaneous
pneumothorax. _Eur. Respir. J._ 9, 1821–1825 (1996). Article CAS PubMed Google Scholar Download references ACKNOWLEDGEMENTS We would like to thank Jia-Chun He for her assistance with the
statistical analysis. The study was supported by research grants from National Taiwan University Hospital, Taipei, Taiwan (NTUH105-P02, NTUH105-003233, MS419), and the Ministry of Science
and Technology, Taiwan (104-2314-B-002-090). AUTHOR INFORMATION Author notes * Tung-Ming Tsai and Mong-Wei Lin contributed equally to this work. AUTHORS AND AFFILIATIONS * Department of
Surgery, National Taiwan University Hospital and National Taiwan University College of Medicine, Taipei, 10002, Taiwan Tung-Ming Tsai, Mong-Wei Lin, Hsao-Hsun Hsu & Jin-Shing Chen *
Graduate Institute of Epidemiology, College of Public Health, National Taiwan University, Taipei, 10055, Taiwan Yao-Jen Li * Genomic Research Center, Academia Sinica, Taipei, 11529, Taiwan
Yao-Jen Li * Department of Medical Research, National Taiwan University Hospital, Taipei, 10002, Taiwan Chin-Hao Chang * Department of Traumatology, National Taiwan University Hospital,
Taipei, 10002, Taiwan Hsien-Chi Liao & Jin-Shing Chen * Division of Thoracic Surgery, Department of Surgery, Far Eastern Memorial Hospital, New Taipei City, 22060, Taiwan Chao-Yu Liu
Authors * Tung-Ming Tsai View author publications You can also search for this author inPubMed Google Scholar * Mong-Wei Lin View author publications You can also search for this author
inPubMed Google Scholar * Yao-Jen Li View author publications You can also search for this author inPubMed Google Scholar * Chin-Hao Chang View author publications You can also search for
this author inPubMed Google Scholar * Hsien-Chi Liao View author publications You can also search for this author inPubMed Google Scholar * Chao-Yu Liu View author publications You can also
search for this author inPubMed Google Scholar * Hsao-Hsun Hsu View author publications You can also search for this author inPubMed Google Scholar * Jin-Shing Chen View author publications
You can also search for this author inPubMed Google Scholar CONTRIBUTIONS Study concept and design: T.T., M.L., H.H., and J.C. Acquisition, analysis, or interpretation of data: T.T., M.L.,
Y.L., C.C., H.L., and C.L. Drafting of the manuscript: T.T., M.L., H.L., and C.L. Critical revision of the manuscript for important intellectual content: M.L., Y.L., C.C., H.H., and J.C.
Statistical analysis: T.T., Y.L., C.C., and J.C. All authors reviewed the manuscript. CORRESPONDING AUTHORS Correspondence to Hsao-Hsun Hsu or Jin-Shing Chen. ETHICS DECLARATIONS COMPETING
INTERESTS The authors declare that they have no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE: Springer Nature remains neutral with regard to jurisdictional claims in
published maps and institutional affiliations. RIGHTS AND PERMISSIONS This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party
material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons
license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ Reprints
and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Tsai, TM., Lin, MW., Li, YJ. _et al._ The Size of Spontaneous Pneumothorax is a Predictor of Unsuccessful Catheter Drainage. _Sci Rep_ 7,
181 (2017). https://doi.org/10.1038/s41598-017-00284-8 Download citation * Received: 29 March 2016 * Accepted: 20 February 2017 * Published: 15 March 2017 * DOI:
https://doi.org/10.1038/s41598-017-00284-8 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative