Supporting sexuality and improving sexual function in transgender persons
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
Sexuality is important for most cisgender as well as transgender persons and is an essential aspect of quality of life. For both the patient and their clinicians, managing gender dysphoria
includes establishing a comfortable relationship with sexual health issues, which can evolve throughout the course of gender-affirming treatment. Gender-affirming endocrine treatment of
transgender men and women has considerable effects on sex drive and sexual function. Gender-affirming surgery (GAS) can improve body satisfaction and ease gender dysphoria, but surgery
itself can be associated with sexual sequelae associated with physical constraints of the new genitals or postsurgical pain, psychological difficulties with accepting the new body, or social
aspects of having changed gender. In general, a positive body image is associated with better sexual function and satisfaction, but satisfaction with sexual function after GAS can be
present despite dissatisfaction with the surgery and vice versa. Factors involved in the integrated experience of gender-affirming treatment and the way in which sexuality is perceived are
complex, and supporting sexuality and improving sexual function in transgender patients is, correspondingly, multifaceted. As the transgender patient moves through their life before, during,
and after gender-affirming treatment, sexuality and sexual function should be considered and maximized at all stages in order to improve quality of life.
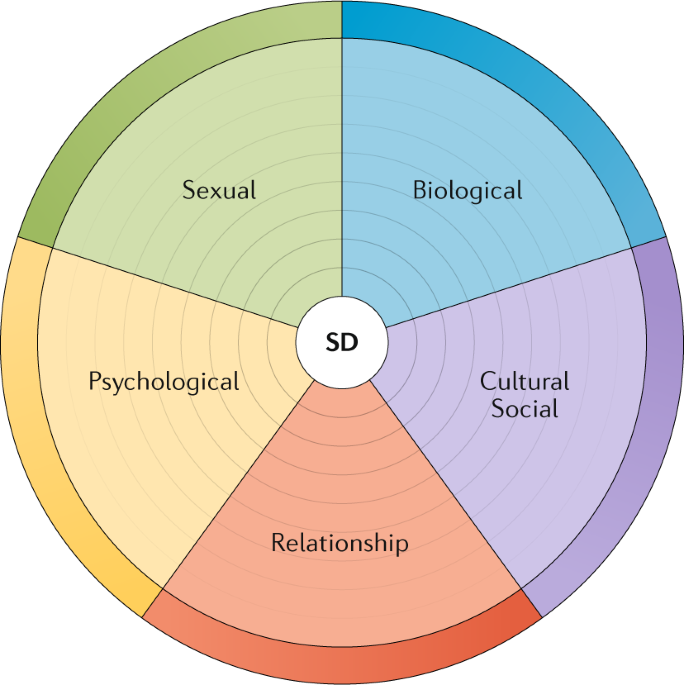
Evaluation of sexual dysfunction in transgender persons is multidimensional.
Hormonal treatment is likely to increase sexual desire in transgender men and decrease desire in transgender women.
A reduction in sexual drive is not necessarily a concern, but can, in fact, be appreciated or even desirable for some patients.
Before initiating hormonal or surgical treatment, wishes and hopes about future sexual function should be explored.
Sexual problems in transgender persons can be trans specific or not. General principles in sexual medicine apply to both cisgender and transgender persons.
The authors would like to thank plastic surgeon H. Sigurjonsson for important feedback regarding the illustrations.
Natural Reviews Urology thanks S. Morrison, T. v. d. Grift and the other anonymous reviewer(s) for the peer review of this manuscript.
All authors researched data for article, made substantial contributions to discussions of content, and wrote and edited the manuscript before submission.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Anyone you share the following link with will be able to read this content: