Back to the future: targeting the extracellular matrix to treat systemic sclerosis
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
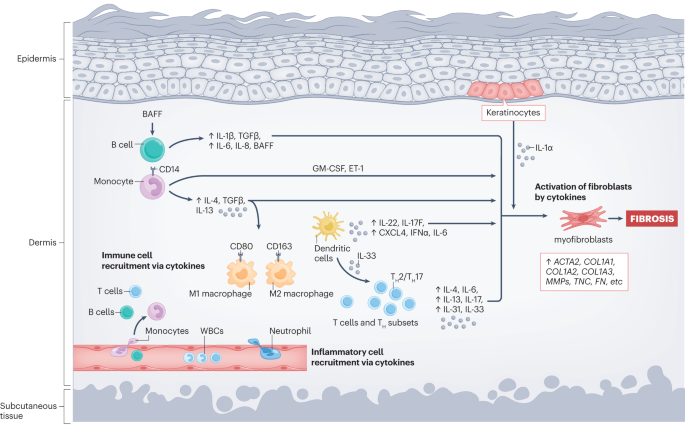
ABSTRACT Fibrosis is the excessive deposition of a stable extracellular matrix (ECM); fibrotic tissue is composed principally of highly crosslinked type I collagen and highly contractile
myofibroblasts. Systemic sclerosis (SSc) is a multisystem autoimmune connective tissue disease characterized by skin and organ fibrosis. The fibrotic process has been recognized in SSc for
>40 years, but drugs with demonstrable efficacy against SSc fibrosis in ameliorating the lung involvement have only recently been identified. Unfortunately, these treatments are
ineffective at improving the skin score in patients with SSc. Previous clinical trials in SSc have largely focused on the cross-purposing of anti-inflammatory drugs and the use of
immunosuppressive drugs from the transplantation field, which address inflammatory and/or autoimmune processes. Limited examination has taken place of specific anti-fibrotic agents developed
through their ability to directly target the ECM in SSc by, for example, alleviating the persistent matrix stiffness and mechanotransduction that might be required for both the initiation
and maintenance of fibrosis, including in SSc. However, because of the importance of the ECM in the SSc phenotype, attempts have now been made to identify drugs that specifically target the
ECM, including some drugs that are currently under consideration for the treatment of cancer. KEY POINTS * Systemic sclerosis (SSc) is a fibrotic disease, and anti-fibrotic agents deserve
consideration as treatments for this disease. * Major efforts have been made in the past ~20–25 years to uncover common mechanisms underlying fibrotic disease, including mechanotransductive
pathways and enzymes that directly affect extracellular matrix stiffness. * Potential SSc targets include collagen prolyl 4-hydroxylase, lysyl oxidase, focal adhesion kinase, TGFβ-activating
integrin subunits, TGFβ-activated kinase 1, yes-associated protein 1, myocardin-related transcription factor A and cellular communication network factors. * Current efforts are focused on
understanding how fibroblast subsets respond excessively to inflammation in fibrosis. Access through your institution Buy or subscribe This is a preview of subscription content, access via
your institution ACCESS OPTIONS Access through your institution Access Nature and 54 other Nature Portfolio journals Get Nature+, our best-value online-access subscription $32.99 / 30 days
cancel any time Learn more Subscribe to this journal Receive 12 print issues and online access $209.00 per year only $17.42 per issue Learn more Buy this article * Purchase on SpringerLink *
Instant access to full article PDF Buy now Prices may be subject to local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional
subscriptions * Read our FAQs * Contact customer support SIMILAR CONTENT BEING VIEWED BY OTHERS IMMUNE CELL DYSREGULATION AS A MEDIATOR OF FIBROSIS IN SYSTEMIC SCLEROSIS Article 09 November
2022 SSC-ILD MOUSE MODEL INDUCED BY OSMOTIC MINIPUMP DELIVERED BLEOMYCIN: EFFECT OF NINTEDANIB Article Open access 16 September 2021 MESENCHYMAL STEM CELLS ALLEVIATE SYSTEMIC SCLEROSIS BY
INHIBITING THE RECRUITMENT OF PATHOGENIC MACROPHAGES Article Open access 26 November 2022 REFERENCES * Herrick, A. L., Assassi, S. & Denton, C. P. Skin involvement in early diffuse
cutaneous systemic sclerosis: an unmet clinical need. _Nat. Rev. Rheumatol._ 18, 276–285 (2022). Article PubMed PubMed Central Google Scholar * Jiang, Y., Turk, M. A. & Pope, J. E.
Factors associated with pulmonary arterial hypertension (PAH) in systemic sclerosis (SSc). _Autoimmun. Rev._ 19, 102602 (2020). Article CAS PubMed Google Scholar * Attanasio, U. et al.
Pulmonary hypertension phenotypes in systemic sclerosis: the right diagnosis for the right treatment. _Int. J. Mol. Sci._ 21, 4430 (2020). Article CAS PubMed PubMed Central Google
Scholar * Siqueira, V. S. et al. Predictors of progression to systemic sclerosis: analysis of very early diagnosis of systemic sclerosis in a large single-centre cohort. _Rheumatology_ 61,
3686–3692 (2022). Article CAS PubMed Google Scholar * Domsic, R. T. et al. Defining the optimal disease duration of early diffuse systemic sclerosis for clinical trial design.
_Rheumatology_ 60, 4662–4670 (2021). Article CAS PubMed PubMed Central Google Scholar * Higley, H. et al. Immunocytochemical localization and serologic detection of transforming growth
factor β1. Association with type I procollagen and inflammatory cell markers in diffuse and limited systemic sclerosis, morphea, and Raynaud’s phenomenon. _Arthritis Rheum._ 37, 278–288
(1994). Article CAS PubMed Google Scholar * Tsou, P. S., Shi, B. & Varga, J. Role of cellular senescence in the pathogenesis of systemic sclerosis. _Curr. Opin. Rheumatol._ 34,
343–350 (2022). Article CAS PubMed Google Scholar * Lescoat, A., Lecureur, V. & Varga, J. Contribution of monocytes and macrophages to the pathogenesis of systemic sclerosis: recent
insights and therapeutic implications. _Curr. Opin. Rheumatol._ 33, 463–470 (2021). Article CAS PubMed Google Scholar * Tsou, P. S., Varga, J. & O’Reilly, S. Advances in epigenetics
in systemic sclerosis: molecular mechanisms and therapeutic potential. _Nat. Rev. Rheumatol._ 17, 596–607 (2021). Article PubMed Google Scholar * Shah, S. & Denton, C. P. Scleroderma
autoantibodies in guiding monitoring and treatment decisions. _Curr. Opin. Rheumatol._ 34, 302–310 (2022). Article CAS PubMed Google Scholar * Lescoat, A., Varga, J., Matucci-Cerinic, M.
& Khanna, D. New promising drugs for the treatment of systemic sclerosis: pathogenic considerations, enhanced classifications, and personalized medicine. _Expert. Opin. Investig. Drugs_
30, 635–652 (2021). Article CAS PubMed PubMed Central Google Scholar * Distler, O. et al. Nintedanib for systemic sclerosis-associated interstitial lung disease. _N. Engl. J. Med._
380, 2518–2528 (2019). Article CAS PubMed Google Scholar * Haynes, D. C. & Gershwin, M. E. The immunopathology of progressive systemic sclerosis (PSS). _Semin. Arthritis Rheum._ 11,
331–351 (1982). Article CAS PubMed Google Scholar * Sappino, A. P., Masouyé, I., Saurat, J. H. & Gabbiani, G. Smooth muscle differentiation in scleroderma fibroblastic cells. _Am. J.
Pathol._ 137, 585–591 (1990). CAS PubMed PubMed Central Google Scholar * Kirk, T. Z., Mark, M. E., Chua, C. C., Chua, B. H. & Mayes, M. D. Myofibroblasts from scleroderma skin
synthesize elevated levels of collagen and tissue inhibitor of metalloproteinase (TIMP-1) with two forms of TIMP-1. _J. Biol. Chem._ 270, 3423–3428 (1995). Article CAS PubMed Google
Scholar * Krieg, T., Perlish, J. S., Mauch, C. & Fleischmajer, R. Collagen synthesis by scleroderma fibroblasts. _Ann. N. Y. Acad. Sci._ 460, 375–386 (1985). Article CAS PubMed
Google Scholar * LeRoy, E. C. The pathogenesis of systemic sclerosis. _Clin. Exp. Rheumatol._ 7, S135–S137 (1989). PubMed Google Scholar * Mauch, C. & Kreig, T. Fibroblast-matrix
interactions and their role in the pathogenesis of fibrosis. _Rheum. Dis. Clin. North. Am._ 16, 93–107 (1990). Article CAS PubMed Google Scholar * van der Slot, A. J. et al.
Identification of PLOD2 as telopeptide lysyl hydroxylase, an important enzyme in fibrosis. _J. Biol. Chem._ 278, 40967–40972 (2003). Article PubMed Google Scholar * Ivarsson, M.,
McWhirter, A., Black, C. M. & Rubin, K. Impaired regulation of collagen pro-α1(I) mRNA and change in pattern of collagen-binding integrins on scleroderma fibroblasts. _J. Invest.
Dermatol._ 101, 216–221 (1993). Article CAS PubMed Google Scholar * Bou-Gharios, G., Osman, J., Black, C. & Olsen, I. Excess matrix accumulation in scleroderma is caused partly by
differential regulation of stromelysin and TIMP-1 synthesis. _Clin. Chim. Acta_ 231, 69–78 (1994). Article CAS PubMed Google Scholar * Wakhlu, A. et al. Assessment of extent of skin
involvement in scleroderma using shear wave elastography. _Indian. J. Rheumatol._ 12, 194–198 (2017). Article Google Scholar * Aden, N. et al. Proteomic analysis of scleroderma lesional
skin reveals activated wound healing phenotype of epidermal cell layer. _Rheumatology_ 47, 1754–1760 (2008). Article CAS PubMed Google Scholar * Allanore, Y. et al. Correlation of serum
collagen I carboxyterminal telopeptide concentrations with cutaneous and pulmonary involvement in systemic sclerosis. _J. Rheumatol._ 30, 68–73 (2003). CAS PubMed Google Scholar * Lurje,
I., Gaisa, N. T., Weiskirchen, R. & Tacke, F. Mechanisms of organ fibrosis: emerging concepts and implications for novel treatment strategies. _Mol. Asp. Med._ 92, 101191 (2023). Article
CAS Google Scholar * Brown, M. & O’Reilly, S. The immunopathogenesis of fibrosis in systemic sclerosis. _Clin. Exp. Immunol._ 195, 310–321 (2019). Article CAS PubMed Google
Scholar * van Bon, L., Cossu, M. & Radstake, T. R. An update on an immune system that goes awry in systemic sclerosis. _Curr. Opin. Rheumatol._ 23, 505–510 (2011). Article PubMed
Google Scholar * Wei, L., Abraham, D. & Ong, V. The Yin and Yang of IL-17 in systemic sclerosis. _Front. Immunol._ 13, 885609 (2022). Article CAS PubMed PubMed Central Google
Scholar * Worrell, J. C. & O’Reilly, S. Bi-directional communication: conversations between fibroblasts and immune cells in systemic sclerosis. _J. Autoimmun._ 113, 102526 (2020).
Article CAS PubMed Google Scholar * Li, G. et al. Skin-resident effector memory CD8+CD28− T cells exhibit a profibrotic phenotype in patients with systemic sclerosis. _J. Invest.
Dermatol._ 137, 1042–1050 (2017). Article CAS PubMed Google Scholar * Yaseen, B. et al. Interleukin-31 promotes pathogenic mechanisms underlying skin and lung fibrosis in scleroderma.
_Rheumatology_ 59, 2625–2636 (2020). Article CAS PubMed Google Scholar * Makhluf, H. A. et al. IL-4 upregulates tenascin synthesis in scleroderma and healthy skin fibroblasts. _J.
Invest. Dermatol._ 107, 856–859 (1996). Article CAS PubMed Google Scholar * Matsushita, T. et al. BAFF inhibition attenuates fibrosis in scleroderma by modulating the regulatory and
effector B cell balance. _Sci. Adv._ 4, eaas9944 (2018). Article PubMed PubMed Central Google Scholar * François, A. et al. B lymphocytes and B-cell activating factor promote collagen
and profibrotic markers expression by dermal fibroblasts in systemic sclerosis. _Arthritis Res. Ther._ 15, R168 (2013). Article PubMed PubMed Central Google Scholar * Matsushita, T. et
al. Elevated serum BAFF levels in patients with systemic sclerosis: enhanced BAFF signaling in systemic sclerosis B lymphocytes. _Arthritis Rheum._ 54, 192–201 (2006). Article CAS PubMed
Google Scholar * van der Kroef, M. et al. CXCL4 triggers monocytes and macrophages to produce PDGF-BB, culminating in fibroblast activation: implications for systemic sclerosis. _J.
Autoimmun._ 111, 102444 (2020). Article PubMed Google Scholar * Binai, N., O’Reilly, S., Griffiths, B., van Laar, J. M. & Hügle, T. Differentiation potential of CD14+ monocytes into
myofibroblasts in patients with systemic sclerosis. _PLoS ONE_ 7, e33508 (2012). Article CAS PubMed PubMed Central Google Scholar * Herrick, A. L. et al. Treatment outcome in early
diffuse cutaneous systemic sclerosis: the European Scleroderma Observational Study (ESOS). _Ann. Rheum. Dis._ 76, 1207–1218 (2017). Article CAS PubMed Google Scholar * Namas, R. et al.
Efficacy of mycophenolate mofetil and oral cyclophosphamide on skin thickness: post hoc analyses from two randomized placebo-controlled trials. _Arthritis Care Res._ 70, 439–444 (2018).
Article CAS Google Scholar * Pakshir, P. et al. The myofibroblast at a glance. _J. Cell Sci._ 133, jcs227900 (2020). Article CAS PubMed Google Scholar * Liu, S. et al. Role of Rac1 in
a bleomycin-induced scleroderma model using fibroblast-specific Rac1-knockout mice. _Arthritis Rheum._ 58, 2189–2195 (2008). Article CAS PubMed Google Scholar * Liu, S., Shi-wen, X.,
Abraham, D. J. & Leask, A. CCN2 is required for bleomycin-induced skin fibrosis in mice. _Arthritis Rheum._ 63, 239–246 (2011). Article CAS PubMed Google Scholar * Tsang, M. et al.
Insights into fibroblast plasticity: cellular communication network 2 is required for activation of cancer-associated fibroblasts in a murine model of melanoma. _Am. J. Pathol._ 190, 206–221
(2020). Article CAS PubMed Google Scholar * Chen, Y. et al. Matrix contraction by dermal fibroblasts requires transforming growth factor-β/activin-linked kinase 5, heparan
sulfate-containing proteoglycans, and MEK/ERK: insights into pathological scarring in chronic fibrotic disease. _Am. J. Pathol._ 167, 1699–1711 (2005). Article CAS PubMed PubMed Central
Google Scholar * Rajkumar, V. S. et al. Shared expression of phenotypic markers in systemic sclerosis indicates a convergence of pericytes and fibroblasts to a myofibroblast lineage in
fibrosis. _Arthritis Res. Ther._ 7, R1113–R1123 (2005). Article CAS PubMed PubMed Central Google Scholar * Rajkumar, V. S., Sundberg, C., Abraham, D. J., Rubin, K. & Black, C. M.
Activation of microvascular pericytes in autoimmune Raynaud’s phenomenon and systemic sclerosis. _Arthritis Rheum._ 42, 930–941 (1999). Article CAS PubMed Google Scholar * Young-Min, S.
A. et al. Serum TIMP-1, TIMP-2, and MMP-1 in patients with systemic sclerosis, primary Raynaud’s phenomenon, and in normal controls. _Ann. Rheum. Dis._ 60, 846–851 (2001). CAS PubMed
PubMed Central Google Scholar * Xu, S. et al. Endothelins: effect on matrix biosynthesis and proliferation in normal and scleroderma fibroblasts. _J. Cardiovasc. Pharmacol._ 31, S360–S363
(1998). Article CAS PubMed Google Scholar * Chanoki, M. et al. Increased expression of lysyl oxidase in skin with scleroderma. _Br. J. Dermatol._ 133, 710–715 (1995). Article CAS
PubMed Google Scholar * Rimar, D. et al. Brief report: lysyl oxidase is a potential biomarker of fibrosis in systemic sclerosis. _Arthritis Rheumatol._ 66, 726–730 (2014). Article PubMed
Google Scholar * Nguyen, X. X. et al. Lysyl oxidase directly contributes to extracellular matrix production and fibrosis in systemic sclerosis. _Am. J. Physiol. Lung Cell Mol. Physiol._
320, L29–L40 (2021). Article CAS PubMed Google Scholar * Siegel, R. C., Pinnell, S. R. & Martin, G. R. Cross-linking of collagen and elastin. Properties of lysyl oxidase.
_Biochemistry_ 9, 4486–4492 (1970). Article CAS PubMed Google Scholar * Peltonen, L., Palotie, A., Myllylä, R., Krieg, T. & Oikarinen, A. Collagen biosynthesis in systemic
scleroderma: regulation of posttranslational modifications and synthesis of procollagen in cultured fibroblasts. _J. Invest. Dermatol._ 84, 14–18 (1985). Article CAS PubMed Google Scholar
* Kawaguchi, Y. et al. Cytokine regulation of prolyl 4-hydroxylase production in skin fibroblast cultures from patients with systemic sclerosis: contribution to collagen synthesis and
fibrosis. _J. Rheumatol._ 19, 1195–1201 (1992). CAS PubMed Google Scholar * Tomasek, J. J., Gabbiani, G., Hinz, B., Chaponnier, C. & Brown, R. A. Myofibroblasts and mechano-regulation
of connective tissue remodelling. _Nat. Rev. Mol. Cell Biol._ 3, 349–363 (2002). Article CAS PubMed Google Scholar * Van De Water, L., Varney, S. & Tomasek, J. J. Mechanoregulation
of the myofibroblast in wound contraction, scarring, and fibrosis: opportunities for new therapeutic intervention. _Adv. Wound Care_ 2, 122–141 (2013). Article Google Scholar * Ogawa, R.
& Hsu, C. K. Mechanobiological dysregulation of the epidermis and dermis in skin disorders and in degeneration. _J. Cell Mol. Med._ 17, 817–822 (2013). Article PubMed PubMed Central
Google Scholar * Leask, A. The hard problem: mechanotransduction perpetuates the myofibroblast phenotype in scleroderma fibrosis. _Wound Repair. Regen._ 29, 582–587 (2021). Article PubMed
Google Scholar * Spiera, R. et al. A randomised, double-blind, placebo-controlled phase 3 study of lenabasum in diffuse cutaneous systemic sclerosis: RESOLVE-1 design and rationale.
_Clin. Exp. Rheumatol._ 239, 124–133 (2021). Article Google Scholar * Khanna, D. et al. Tocilizumab in systemic sclerosis: a randomised, double-blind, placebo-controlled, phase 3 trial.
_Lancet Respir. Med._ 8, 963–974 (2020). Article CAS PubMed Google Scholar * Khanna, D. et al. An open-label, phase II study of the safety and tolerability of pirfenidone in patients
with scleroderma-associated interstitial lung disease: the LOTUSS trial. _J. Rheumatol._ 43, 1672–1679 (2016). Article PubMed Google Scholar * Leask, A. Signaling in fibrosis: targeting
the TGFbeta, endothelin-1 and CCN2 axis in scleroderma. _Front. Biosci._ 1, 115–122 (2009). Google Scholar * Leask, A., Holmes, A., Black, C. M. & Abraham, D. J. Connective tissue
growth factor gene regulation. Requirements for its induction by transforming growth factor-β2 in fibroblasts. _J. Biol. Chem._ 278, 13008–13015 (2003). Article CAS PubMed Google Scholar
* Thannickal, V. J. et al. Myofibroblast differentiation by transforming growth factor-β1 is dependent on cell adhesion and integrin signaling via focal adhesion kinase. _J. Biol. Chem._
278, 12384–12389 (2003). Article CAS PubMed Google Scholar * Shi-wen, X. et al. Requirement of transforming growth factor β-activated kinase 1 for transforming growth factor β-induced
α-smooth muscle actin expression and extracellular matrix contraction in fibroblasts. _Arthritis Rheum._ 60, 234–241 (2009). Article PubMed Google Scholar * Lagares, D. et al. Inhibition
of focal adhesion kinase prevents experimental lung fibrosis and myofibroblast formation. _Arthritis Rheum._ 64, 1653–1664 (2012). Article CAS PubMed PubMed Central Google Scholar *
Shi-wen, X. et al. Focal adhesion kinase and reactive oxygen species contribute to the persistent fibrotic phenotype of lesional scleroderma fibroblasts. _Rheumatology_ 51, 2146–2154 (2012).
Article PubMed Google Scholar * Khan, Z. & Marshall, J. F. The role of integrins in TGFβ activation in the tumour stroma. _Cell Tissue Res._ 365, 657–673 (2016). Article CAS PubMed
PubMed Central Google Scholar * Asano, Y., Ihn, H., Jinnin, M., Mimura, Y. & Tamaki, K. Involvement of αvβ5 integrin in the establishment of autocrine TGF-β signaling in dermal
fibroblasts derived from localized scleroderma. _J. Invest. Dermatol._ 126, 1761–1769 (2006). Article CAS PubMed Google Scholar * Asano, Y. et al. Increased expression of integrin αvβ3
contributes to the establishment of autocrine TGF-β signaling in scleroderma fibroblasts. _J. Immunol._ 175, 7708–7718 (2005). Article CAS PubMed Google Scholar * Asano, Y., Ihn, H.,
Yamane, K., Jinnin, M. & Tamaki, K. Increased expression of integrin αvβ5 induces the myofibroblastic differentiation of dermal fibroblasts. _Am. J. Pathol._ 168, 499–510 (2006). Article
CAS PubMed PubMed Central Google Scholar * Munger, J. S. et al. The integrin αvβ6 binds and activates latent TGF β1: a mechanism for regulating pulmonary inflammation and fibrosis.
_Cell_ 96, 319–328 (1999). Article CAS PubMed Google Scholar * Liu, S. et al. Expression of integrin β1 by fibroblasts is required for tissue repair in vivo. _J. Cell Sci._ 123,
3674–3682 (2010). Article CAS PubMed Google Scholar * Myllyharju, J. Prolyl 4-hydroxylases, key enzymes in the synthesis of collagens and regulation of the response to hypoxia, and their
roles as treatment targets. _Ann. Med._ 40, 402–417 (2008). Article CAS PubMed Google Scholar * Gorres, K. L. & Raines, R. T. Prolyl 4-hydroxylase. _Crit. Rev. Biochem. Mol. Biol._
45, 106–124 (2010). Article CAS PubMed PubMed Central Google Scholar * Franklin, T. J. Therapeutic approaches to organ fibrosis. _Int. J. Biochem. Cell Biol._ 29, 79–89 (1997). Article
CAS PubMed Google Scholar * Böker, K., Schwarting, G., Kaule, G., Günzler, V. & Schmidt, E. Fibrosis of the liver in rats induced by bile duct ligation. Effects of inhibition by
prolyl 4-hydroxylase. _J. Hepatol._ 13, S35–S40 (1991). Article PubMed Google Scholar * Bickel, M. et al. Selective inhibition of hepatic collagen accumulation in experimental liver
fibrosis in rats by a new prolyl 4-hydroxylase inhibitor. _Hepatology_ 28, 404–411 (1998). Article CAS PubMed Google Scholar * Nwogu, J. I. et al. Inhibition of collagen synthesis with
prolyl 4-hydroxylase inhibitor improves left ventricular function and alters the pattern of left ventricular dilatation after myocardial infarction. _Circulation_ 104, 2216–2221 (2001).
Article CAS PubMed Google Scholar * Bolarin, D. M., Palicharla, P. & Fuller, G. C. Enzymes of collagen synthesis in lung tissues of bleomycin-induced pulmonary fibrosis. _Toxicol.
Appl. Pharmacol._ 73, 188–191 (1984). Article CAS PubMed Google Scholar * Takeda, K., Kawai, S., Kato, F., Tetsuka, T. & Konno, K. Stimulation of prolyl hydroxylase activity by
bleomycin. _J. Antibiot._ 31, 884–887 (1978). Article CAS Google Scholar * Tschank, G., Raghunath, M., Günzler, V. & Hanauske-Abel, H. M. Pyridinedicarboxylates, the first
mechanism-derived inhibitors for prolyl 4-hydroxylase, selectively suppress cellular hydroxyprolyl biosynthesis. Decrease in interstitial collagen and Clq secretion in cell culture.
_Biochem. J._ 248, 625–633 (1987). Article CAS PubMed PubMed Central Google Scholar * Vasta, J. D. et al. Selective inhibition of collagen prolyl 4-hydroxylase in human cells. _ACS
Chem. Biol._ 11, 193–199 (2016). Article CAS PubMed Google Scholar * Szauter, K. M., Cao, T., Boyd, C. D. & Csiszar, K. Lysyl oxidase in development, aging and pathologies of the
skin. _Pathol. Biol._ 53, 448–456 (2005). Article CAS PubMed Google Scholar * Pharmaxis. Product pipeline: amine oxidase platform. _Pharmaxis_
https://www.pharmaxis.com.au/product-pipeline/amine-oxidase-platform/ (2023). * Infante, J. R. et al. Safety, pharmacokinetic, and pharmacodynamic phase I dose-escalation trial of
PF-00562271, an inhibitor of focal adhesion kinase, in advanced solid tumors. _J. Clin. Oncol._ 30, 1527–1533 (2012). Article CAS PubMed Google Scholar * Peidl, A., Perbal, B. &
Leask, A. Yin/Yang expression of CCN family members: transforming growth factor beta 1, via ALK5/FAK/MEK, induces CCN1 and CCN2, yet suppresses CCN3, expression in human dermal fibroblasts.
_PLoS ONE_ 14, e0218178 (2019). Article CAS PubMed PubMed Central Google Scholar * Jones, S. F. et al. A phase I study of VS-6063, a second-generation focal adhesion kinase inhibitor,
in patients with advanced solid tumors. _Invest. N. Drugs_ 33, 1100–1107 (2015). Article CAS Google Scholar * Gerber, D. E. et al. Phase 2 study of the focal adhesion kinase inhibitor
defactinib (VS-6063) in previously treated advanced KRAS mutant non-small cell lung cancer. _Lung Cancer_ 139, 60–67 (2020). Article PubMed Google Scholar * Wang-Gillam, A. et al.
Defactinib, pembrolizumab, and gemcitabine in patients with advanced treatment refractory pancreatic cancer: a phase I dose escalation and expansion study. _Clin. Cancer Res._ 28, 5254–5262
(2022). Article CAS PubMed PubMed Central Google Scholar * François, R. A. et al. Targeting focal adhesion kinase and resistance to mTOR inhibition in pancreatic neuroendocrine tumors.
_J. Natl Cancer Inst._ 107, djv123 (2015). Article PubMed PubMed Central Google Scholar * Henderson, N. C. et al. Targeting of αv integrin identifies a core molecular pathway that
regulates fibrosis in several organs. _Nat. Med._ 19, 1617–1624 (2013). Article CAS PubMed Google Scholar * Reed, N. I. et al. The αvβ1 integrin plays a critical in vivo role in tissue
fibrosis. _Sci. Transl. Med._ 7, 288ra79 (2015). Article PubMed PubMed Central Google Scholar * Mullard, A. Pliant’s integrin inhibitor boosted by phase II IPF data. _Nat. Rev. Drug.
Discov._ 21, 626 (2022). PubMed Google Scholar * Liu, S. & Leask, A. Integrin β1 is required for dermal homeostasis. _J. Invest. Dermatol._ 133, 899–906 (2013). Article CAS PubMed
Google Scholar * Riopel, M. M., Li, J., Liu, S., Leask, A. & Wang, R. β1 integrin-extracellular matrix interactions are essential for maintaining exocrine pancreas architecture and
function. _Lab. Invest._ 93, 31–40 (2013). Article CAS PubMed Google Scholar * Parapuram, S. K., Huh, K., Liu, S. & Leask, A. Integrin β1 is necessary for the maintenance of corneal
structural integrity. _Invest. Ophthalmol. Vis. Sci._ 52, 7799–7806 (2011). Article CAS PubMed Google Scholar * Liu, S. & Leask, A. Integrin β1 is required for maintenance of
vascular tone in postnatal mice. _J. Cell Commun. Signal._ 6, 175–180 (2012). Article PubMed PubMed Central Google Scholar * Zeltz, C. et al. Integrin α11β1 in tumor fibrosis: more than
just another cancer-associated fibroblast biomarker? _J. Cell Commun. Signal._ 16, 649–666 (2022). Article CAS PubMed PubMed Central Google Scholar * Zeltz, C. et al. α11β1 integrin is
induced in a subset of cancer-associated fibroblasts in desmoplastic tumor stroma and mediates in vitro cell migration. _Cancers_ 11, 765 (2019). Article CAS PubMed PubMed Central Google
Scholar * Wang, W. et al. TAK1: a molecular link between liver inflammation, fibrosis, steatosis, and carcinogenesis. _Front. Cell Dev. Biol._ 9, 734749 (2021). Article PubMed PubMed
Central Google Scholar * Totzke, J. et al. Takinib, a selective TAK1 inhibitor, broadens the therapeutic efficacy of TNF-α inhibition for cancer and autoimmune disease. _Cell Chem. Biol._
24, 1029–1039.e7 (2017). Article CAS PubMed PubMed Central Google Scholar * Scarneo, S. et al. Development and efficacy of an orally bioavailable selective TAK1 inhibitor for the
treatment of inflammatory arthritis. _ACS Chem. Biol._ 17, 536–544 (2022). Article CAS PubMed PubMed Central Google Scholar * Scarneo, S. A. et al. Pharmacological inhibition of TAK1,
with the selective inhibitor takinib, alleviates clinical manifestation of arthritis in CIA mice. _Arthritis Res. Ther._ 21, 292 (2019). Article CAS PubMed PubMed Central Google Scholar
* Foster, C. T., Gualdrini, F. & Treisman, R. Mutual dependence of the MRTF-SRF and YAP-TEAD pathways in cancer-associated fibroblasts is indirect and mediated by cytoskeletal
dynamics. _Genes. Dev._ 31, 2361–2375 (2017). Article CAS PubMed PubMed Central Google Scholar * Gibault, F. et al. Non-photoinduced biological properties of verteporfin. _Curr. Med.
Chem._ 23, 1171–1184 (2016). Article CAS PubMed Google Scholar * Seeneevassen, L., Dubus, P., Gronnier, C. & Varon, C. Hippo in gastric cancer: from signalling to therapy. _Cancers_
14, 2282 (2022). Article CAS PubMed PubMed Central Google Scholar * Shi-Wen, X. et al. Verteporfin inhibits the persistent fibrotic phenotype of lesional scleroderma dermal fibroblasts.
_J. Cell Commun. Signal._ 15, 71–80 (2021). Article CAS PubMed PubMed Central Google Scholar * Chitturi, P. et al. The _Tripterygium wilfordii_ derivative celastrol, a YAP inhibitor,
has anti-fibrotic effects in systemic sclerosis. _Ann. Rheum. Dis._ 82, 1191–1204 (2023). PubMed Google Scholar * Shiwen, X. et al. A role of myocardin related transcription factor-A
(MRTF-A) in scleroderma related fibrosis. _PLoS ONE_ 10, e0126015 (2015). Article PubMed PubMed Central Google Scholar * Ma, H. Y. et al. Inhibition of MRTF activation as a clinically
achievable anti-fibrotic mechanism for pirfenidone. _Eur. Respir. J._ 61, 2200604 (2023). Article CAS PubMed PubMed Central Google Scholar * Leask, A. Conjunction junction, what’s the
function? CCN proteins as targets in fibrosis and cancers. _Am. J. Physiol. Cell Physiol._ 318, C1046–C1054 (2020). Article CAS PubMed PubMed Central Google Scholar * Chen, Y. et al.
CCN2 (connective tissue growth factor) promotes fibroblast adhesion to fibronectin. _Mol. Biol. Cell_ 15, 5635–5646 (2004). Article CAS PubMed PubMed Central Google Scholar * Shi-wen,
X. et al. CCN2 is necessary for adhesive responses to transforming growth factor-β1 in embryonic fibroblasts. _J. Biol. Chem._ 281, 10715–10726 (2006). Article PubMed Google Scholar *
Lau, L. F. Cell surface receptors for CCN proteins. _J. Cell Commun. Signal._ 10, 121–127 (2016). Article PubMed PubMed Central Google Scholar * Richeldi, L. et al. Pamrevlumab, an
anti-connective tissue growth factor therapy, for idiopathic pulmonary fibrosis (PRAISE): a phase 2, randomised, double-blind, placebo-controlled trial. _Lancet Respir. Med._ 28, 25–33
(2020). Article Google Scholar * Makino, K. et al. Anti-connective tissue growth factor (CTGF/CCN2) monoclonal antibody attenuates skin fibrosis in mice models of systemic sclerosis.
_Arthritis Res. Ther._ 19, 134 (2017). Article PubMed PubMed Central Google Scholar * Liu, S., Thompson, K. & Leask, A. CCN2 expression by fibroblasts is not required for cutaneous
tissue repair. _Wound Repair. Regen._ 22, 119–124 (2014). Article PubMed Google Scholar * Liu, S., Parapuram, S. K. & Leask, A. Fibrosis caused by loss of PTEN expression in mouse
fibroblasts is crucially dependent on CCN2. _Arthritis Rheum._ 65, 2940–2944 (2013). Article CAS PubMed Google Scholar * FibroGen. FibroGen announces topline results from phase 3
ZEPHYRUS-1 study of pamrevlumab for the treatment of idiopathic pulmonary fibrosis. _FibroGen_
https://fibrogen.gcs-web.com/news-releases/news-release-details/fibrogen-announces-topline-results-phase-3-zephyrus-1-study (2023). * Grazioli, S. et al. CYR61 (CCN1) overexpression induces
lung injury in mice. _Am. J. Physiol. Lung Cell Mol. Physiol._ 308, L759–L765 (2015). Article CAS PubMed PubMed Central Google Scholar * Kurundkar, A. R. et al. The matricellular
protein CCN1 enhances TGF-β1/SMAD3-dependent profibrotic signaling in fibroblasts and contributes to fibrogenic responses to lung injury. _FASEB J._ 30, 2135–2150 (2016). Article CAS
PubMed PubMed Central Google Scholar * Kulkarni, T. et al. The senescence-associated matricellular protein CCN1 in plasma of human subjects with idiopathic pulmonary fibrosis. _Respir.
Med._ 161, 105821 (2020). Article PubMed Google Scholar * Quesnel, K. et al. CCN1 expression by fibroblasts is required for bleomycin-induced skin fibrosis. _Matrix Biol._ 3, 100009
(2019). Article Google Scholar * Königshoff, M. et al. WNT1-inducible signaling protein-1 mediates pulmonary fibrosis in mice and is upregulated in humans with idiopathic pulmonary
fibrosis. _J. Clin. Invest._ 119, 772–787 (2009). PubMed PubMed Central Google Scholar * FibroGen. Pamrevlumab trials. _FibroGen_ https://www.fibrogen.com/pamrevlumab-trials (2023). * Lu,
G. et al. Co-administered antibody improves penetration of antibody–dye conjugate into human cancers with implications for antibody–drug conjugates. _Nat. Commun._ 211, 5667 (2020). Article
Google Scholar * Resovi, A. et al. CCN-based therapeutic peptides modify pancreatic ductal adenocarcinoma microenvironment and decrease tumor growth in combination with chemotherapy.
_Cells_ 9, 952 (2020). Article CAS PubMed PubMed Central Google Scholar * Riser, B. L., Barnes, J. L. & Varani, J. Balanced regulation of the CCN family of matricellular proteins: a
novel approach to the prevention and treatment of fibrosis and cancer. _J. Cell Commun. Signal._ 9, 327–339 (2015). Article PubMed PubMed Central Google Scholar * Leask, A. Yin and Yang
revisited: CCN3 as an anti-fibrotic therapeutic? _J. Cell Commun. Signal._ 9, 97–98 (2015). Article PubMed PubMed Central Google Scholar * & Leask, A. Yin and Yang: CCN3 inhibits
the pro-fibrotic effects of CCN2. _J. Cell Commun. Signal._ 3, 161–162 (2009). Article PubMed PubMed Central Google Scholar * Pliant Therapeutics. World-class drug development
capabilities. _Pliant_ https://pliantrx.com/pipeline/ (2023). * Adami, E. et al. IL11 is elevated in systemic sclerosis and IL11-dependent ERK signalling underlies TGFβ-mediated activation
of dermal fibroblasts. _Rheumatology_ 60, 5820–5826 (2021). Article CAS PubMed PubMed Central Google Scholar * Werner, G. et al. Single-cell transcriptome analysis identifies
subclusters with inflammatory fibroblast responses in localized scleroderma. _Int. J. Mol. Sci._ 24, 9796 (2023). Article CAS PubMed PubMed Central Google Scholar * Ishida, Y.,
Kuninaka, Y., Mukaida, N. & Kondo, T. Immune mechanisms of pulmonary fibrosis with bleomycin. _Int. J. Mol. Sci._ 24, 3149 (2023). Article CAS PubMed PubMed Central Google Scholar *
Lagares, D. & Hinz, B. Animal and human models of tissue repair and fibrosis: an introduction. _Methods Mol. Biol._ 2299, 277–290 (2021). Article CAS PubMed Google Scholar Download
references AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * College of Dentistry, University of Saskatchewan, Saskatoon, Saskatchewan, Canada Andrew Leask & Angha Naik * Centre for
Rheumatology and Connective Tissue Diseases, UCL Division of Medicine, London, UK Richard J. Stratton Authors * Andrew Leask View author publications You can also search for this author
inPubMed Google Scholar * Angha Naik View author publications You can also search for this author inPubMed Google Scholar * Richard J. Stratton View author publications You can also search
for this author inPubMed Google Scholar CONTRIBUTIONS All authors researched data for the article. A.L. and R.J.S. contributed substantially to discussion of the content. All authors wrote
the article. All authors reviewed and/or edited the manuscript before submission. CORRESPONDING AUTHOR Correspondence to Andrew Leask. ETHICS DECLARATIONS COMPETING INTERESTS The authors
declare no competing interests. PEER REVIEW PEER REVIEW INFORMATION _Nature Reviews Rheumatology_ thanks Yoshihide Asano, Gabriela Kania and the other, anonymous, reviewer(s) for their
contribution to the peer review of this work. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional
affiliations. RIGHTS AND PERMISSIONS Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s)
or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law. Reprints
and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Leask, A., Naik, A. & Stratton, R.J. Back to the future: targeting the extracellular matrix to treat systemic sclerosis. _Nat Rev
Rheumatol_ 19, 713–723 (2023). https://doi.org/10.1038/s41584-023-01032-1 Download citation * Accepted: 31 August 2023 * Published: 03 October 2023 * Issue Date: November 2023 * DOI:
https://doi.org/10.1038/s41584-023-01032-1 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative