Lineage plasticity in cancer: a shared pathway of therapeutic resistance
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
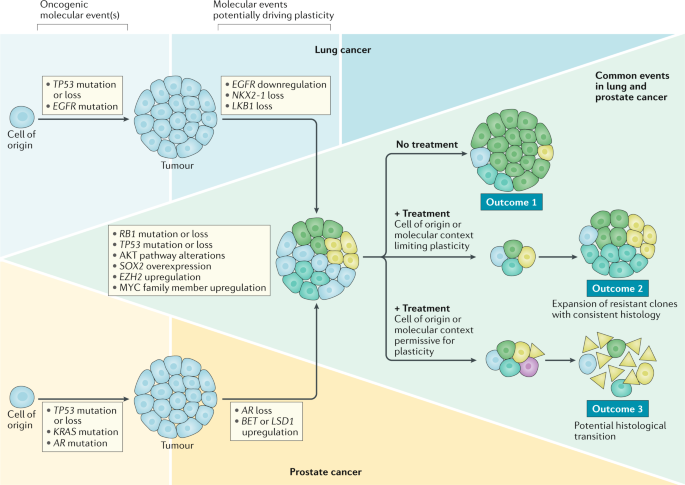
ABSTRACT Lineage plasticity, the ability of cells to transition from one committed developmental pathway to another, has been proposed as a source of intratumoural heterogeneity and of
tumour adaptation to an adverse tumour microenvironment including exposure to targeted anticancer treatments. Tumour cell conversion into a different histological subtype has been associated
with a loss of dependency on the original oncogenic driver, leading to therapeutic resistance. A well-known pathway of lineage plasticity in cancer — the histological transformation of
adenocarcinomas to aggressive neuroendocrine derivatives — was initially described in lung cancers harbouring an _EGFR_ mutation, and was subsequently reported in multiple other
adenocarcinomas, including prostate cancer in the presence of antiandrogens. Squamous transformation is a subsequently identified and less well-characterized pathway of adenocarcinoma escape
from suppressive anticancer therapy. The increased practice of tumour re-biopsy upon disease progression has increased the recognition of these mechanisms of resistance and has improved our
understanding of the underlying biology. In this Review, we provide an overview of the impact of lineage plasticity on cancer progression and therapy resistance, with a focus on
neuroendocrine transformation in lung and prostate tumours. We discuss the current understanding of the molecular drivers of this phenomenon, emerging management strategies and open
questions in the field. KEY POINTS * Lineage plasticity can promote both metastasis and therapy resistance. * Histological transformation occurs in up to 5% of _EGFR_-mutant lung
adenocarcinomas and at least 20% of prostate adenocarcinomas on targeted therapy. * RB1 and p53 deficiency are implicated in — but not sufficient for — neuroendocrine transformation. * AKT
pathway activation and aberrant activity of the MYC and SOX families of transcriptional regulators have been implicated as being effectors of histological transformation. Access through your
institution Buy or subscribe This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through your institution Access Nature and 54 other Nature
Portfolio journals Get Nature+, our best-value online-access subscription $32.99 / 30 days cancel any time Learn more Subscribe to this journal Receive 12 print issues and online access
$209.00 per year only $17.42 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now Prices may be subject to local taxes which are
calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer support SIMILAR CONTENT BEING VIEWED BY OTHERS
SUBSETS OF CANCER CELLS EXPRESSING CX3CR1 ARE ENDOWED WITH METASTASIS-INITIATING PROPERTIES AND RESISTANCE TO CHEMOTHERAPY Article 08 January 2022 TUMOR CELL PLASTICITY IN TARGETED
THERAPY-INDUCED RESISTANCE: MECHANISMS AND NEW STRATEGIES Article Open access 11 March 2023 THE NEUROENDOCRINE TRANSITION IN PROSTATE CANCER IS DYNAMIC AND DEPENDENT ON ASCL1 Article Open
access 11 October 2024 CHANGE HISTORY * _ 17 MARCH 2020 A Correction to this paper has been published: https://doi.org/10.1038/s41571-020-0355-5 _ REFERENCES * Sipos, F., Constantinovits, M.
& Muzes, G. Intratumoral functional heterogeneity and chemotherapy. _World J. Gastroenterol._ 20, 2429–2432 (2014). PubMed PubMed Central Google Scholar * Zellmer, V. R. & Zhang,
S. Evolving concepts of tumor heterogeneity. _Cell Biosci._ 4, 69 (2014). PubMed PubMed Central Google Scholar * Calbo, J. et al. A functional role for tumor cell heterogeneity in a
mouse model of small cell lung cancer. _Cancer Cell_ 19, 244–256 (2011). CAS PubMed Google Scholar * Lim, J. S. et al. Intratumoural heterogeneity generated by Notch signalling promotes
small-cell lung cancer. _Nature_ 545, 360–364 (2017). CAS PubMed PubMed Central Google Scholar * Dongre, A. & Weinberg, R. A. New insights into the mechanisms of
epithelial-mesenchymal transition and implications for cancer. _Nat. Rev. Mol. Cell Biol._ 20, 69–84 (2019). CAS PubMed Google Scholar * Rios, A. C. et al. Intraclonal plasticity in
mammary tumors revealed through large-scale single-cell resolution 3D imaging. _Cancer Cell_ 35, 618–632.e6 (2019). CAS PubMed Google Scholar * Hao, Y. et al. TGFbeta signaling limits
lineage plasticity in prostate cancer. _PLOS Genet._ 14, e1007409 (2018). PubMed PubMed Central Google Scholar * Guo, W. et al. Slug and Sox9 cooperatively determine the mammary stem cell
state. _Cell_ 148, 1015–1028 (2012). CAS PubMed PubMed Central Google Scholar * Mani, S. A. et al. The epithelial-mesenchymal transition generates cells with properties of stem cells.
_Cell_ 133, 704–715 (2008). CAS PubMed PubMed Central Google Scholar * Grosse-Wilde, A. et al. Stemness of the hybrid epithelial/mesenchymal state in breast cancer and its association
with poor survival. _PLoS One_ 10, e0126522 (2015). PubMed PubMed Central Google Scholar * McCoy, E. L. et al. Six1 expands the mouse mammary epithelial stem/progenitor cell pool and
induces mammary tumors that undergo epithelial-mesenchymal transition. _J. Clin. Invest._ 119, 2663–2677 (2009). CAS PubMed PubMed Central Google Scholar * Yu, M. et al. A
developmentally regulated inducer of EMT, LBX1, contributes to breast cancer progression. _Genes Dev._ 23, 1737–1742 (2009). CAS PubMed PubMed Central Google Scholar * Aiello, N. M. et
al. EMT subtype influences epithelial plasticity and mode of cell migration. _Dev. Cell_ 45, 681–695.e4 (2018). CAS PubMed PubMed Central Google Scholar * Reyngold, M. et al. Remodeling
of the methylation landscape in breast cancer metastasis. _PLoS One_ 9, e103896 (2014). PubMed PubMed Central Google Scholar * Munoz, D. P. et al. Activation-induced cytidine deaminase
(AID) is necessary for the epithelial-mesenchymal transition in mammary epithelial cells. _Proc. Natl Acad. Sci. USA_ 110, E2977–E2986 (2013). CAS PubMed PubMed Central Google Scholar *
Lopez-Lago, M. A. et al. Genomic deregulation during metastasis of renal cell carcinoma implements a myofibroblast-like program of gene expression. _Cancer Res._ 70, 9682–9692 (2010). CAS
PubMed PubMed Central Google Scholar * Carmona, F. J. et al. Epigenetic disruption of cadherin-11 in human cancer metastasis. _J. Pathol._ 228, 230–240 (2012). CAS PubMed PubMed Central
Google Scholar * Ezponda, T. et al. The histone methyltransferase MMSET/WHSC1 activates TWIST1 to promote an epithelial-mesenchymal transition and invasive properties of prostate cancer.
_Oncogene_ 32, 2882–2890 (2013). CAS PubMed Google Scholar * Cedar, H. & Bergman, Y. Linking DNA methylation and histone modification: patterns and paradigms. _Nat. Rev. Genet._ 10,
295–304 (2009). CAS PubMed Google Scholar * Bernstein, B. E. et al. A bivalent chromatin structure marks key developmental genes in embryonic stem cells. _Cell_ 125, 315–326 (2006). CAS
PubMed Google Scholar * Maruyama, R. et al. Epigenetic regulation of cell type-specific expression patterns in the human mammary epithelium. _PLOS Genet._ 7, e1001369 (2011). CAS PubMed
PubMed Central Google Scholar * Chaffer, C. L. et al. Poised chromatin at the ZEB1 promoter enables breast cancer cell plasticity and enhances tumorigenicity. _Cell_ 154, 61–74 (2013). CAS
PubMed PubMed Central Google Scholar * Lamouille, S., Xu, J. & Derynck, R. Molecular mechanisms of epithelial-mesenchymal transition. _Nat. Rev. Mol. Cell Biol._ 15, 178–196 (2014).
CAS PubMed PubMed Central Google Scholar * Chen, S. et al. Conversion of epithelial-to-mesenchymal transition to mesenchymal-to-epithelial transition is mediated by oxygen concentration
in pancreatic cancer cells. _Oncol. Lett._ 15, 7144–7152 (2018). PubMed PubMed Central Google Scholar * Lim, S. et al. Lysine-specific demethylase 1 (LSD1) is highly expressed in
ER-negative breast cancers and a biomarker predicting aggressive biology. _Carcinogenesis_ 31, 512–520 (2010). CAS PubMed Google Scholar * Harris, W. J. et al. The histone demethylase
KDM1A sustains the oncogenic potential of MLL-AF9 leukemia stem cells. _Cancer Cell_ 21, 473–487 (2012). CAS PubMed Google Scholar * Dong, C. et al. Interaction with Suv39H1 is critical
for Snail-mediated E-cadherin repression in breast cancer. _Oncogene_ 32, 1351–1362 (2013). CAS PubMed Google Scholar * Herranz, N. et al. Polycomb complex 2 is required for E-cadherin
repression by the Snail1 transcription factor. _Mol. Cell. Biol._ 28, 4772–4781 (2008). CAS PubMed PubMed Central Google Scholar * Dong, C. et al. G9a interacts with Snail and is
critical for Snail-mediated E-cadherin repression in human breast cancer. _J. Clin. Invest._ 122, 1469–1486 (2012). CAS PubMed PubMed Central Google Scholar * Pattabiraman, D. R. et al.
Activation of PKA leads to mesenchymal-to-epithelial transition and loss of tumor-initiating ability. _Science_ 351, aad3680 (2016). PubMed PubMed Central Google Scholar * Wingrove, E. et
al. Transcriptomic hallmarks of tumor plasticity and stromal interactions in brain metastasis. _Cell Rep._ 27, 1277–1292 (2019). CAS PubMed PubMed Central Google Scholar * Kiss, M., Van
Gassen, S., Movahedi, K., Saeys, Y. & Laoui, D. Myeloid cell heterogeneity in cancer: not a single cell alike. _Cell Immunol._ 330, 188–201 (2018). CAS PubMed Google Scholar * Park,
E. S. et al. Cross-species hybridization of microarrays for studying tumor transcriptome of brain metastasis. _Proc. Natl Acad. Sci. USA_ 108, 17456–17461 (2011). CAS PubMed PubMed Central
Google Scholar * Sato, R. et al. RNA sequencing analysis reveals interactions between breast cancer or melanoma cells and the tissue microenvironment during brain metastasis. _Biomed.
Res. Int._ 2017, 8032910 (2017). PubMed PubMed Central Google Scholar * Tata, P. R. et al. Developmental history provides a roadmap for the emergence of tumor plasticity. _Dev. Cell_ 44,
679–693 (2018). CAS PubMed PubMed Central Google Scholar * Zhang, H. et al. Lkb1 inactivation drives lung cancer lineage switching governed by polycomb repressive complex 2. _Nat.
Commun._ 8, 14922 (2017). CAS PubMed PubMed Central Google Scholar * Mukhopadhyay, A. et al. Sox2 cooperates with Lkb1 loss in a mouse model of squamous cell lung cancer. _Cell Rep._ 8,
40–49 (2014). CAS PubMed PubMed Central Google Scholar * Ferone, G. et al. SOX2 is the determining oncogenic switch in promoting lung squamous cell carcinoma from different cells of
origin. _Cancer Cell_ 30, 519–532 (2016). CAS PubMed PubMed Central Google Scholar * Kim, W. et al. Targeted disruption of the EZH2-EED complex inhibits EZH2-dependent cancer. _Nat.
Chem. Biol._ 9, 643–650 (2013). CAS PubMed PubMed Central Google Scholar * Kwon, O. J., Zhang, L., Ittmann, M. M. & Xin, L. Prostatic inflammation enhances basal-to-luminal
differentiation and accelerates initiation of prostate cancer with a basal cell origin. _Proc. Natl Acad. Sci. USA_ 111, E592–E600 (2014). CAS PubMed Google Scholar * Tata, P. R. &
Rajagopal, J. Plasticity in the lung: making and breaking cell identity. _Development_ 144, 755–766 (2017). CAS PubMed PubMed Central Google Scholar * Yu, H. A. et al. Analysis of tumor
specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. _Clin. Cancer Res._ 19, 2240–2247 (2013). CAS PubMed PubMed Central Google
Scholar * Huang, Y., Jiang, X., Liang, X. & Jiang, G. Molecular and cellular mechanisms of castration resistant prostate cancer. _Oncol. Lett._ 15, 6063–6076 (2018). PubMed PubMed
Central Google Scholar * Zou, M. et al. Transdifferentiation as a mechanism of treatment resistance in a mouse model of castration-resistant prostate cancer. _Cancer Discov._ 7, 736–749
(2017). CAS PubMed PubMed Central Google Scholar * Bluemn, E. G. et al. Androgen receptor pathway-independent prostate cancer is sustained through FGF signaling. _Cancer Cell_ 32,
474–489 (2017). CAS PubMed PubMed Central Google Scholar * Sehrawat, A. et al. LSD1 activates a lethal prostate cancer gene network independently of its demethylase function. _Proc. Natl
Acad. Sci. USA_ 115, E4179–E4188 (2018). CAS PubMed PubMed Central Google Scholar * Welti, J. et al. Targeting bromodomain and extra-terminal (bet) family proteins in
castration-resistant prostate cancer (CRPC). _Clin. Cancer Res._ 24, 3149–3162 (2018). CAS PubMed Google Scholar * Biehs, B. et al. A cell identity switch allows residual BCC to survive
Hedgehog pathway inhibition. _Nature_ 562, 429–433 (2018). CAS PubMed Google Scholar * Sanchez-Danes, A. et al. A slow-cycling LGR5 tumour population mediates basal cell carcinoma relapse
after therapy. _Nature_ 562, 434–438 (2018). CAS PubMed PubMed Central Google Scholar * Tsoi, J. et al. Multi-stage differentiation defines melanoma subtypes with differential
vulnerability to drug-induced iron-dependent oxidative stress. _Cancer Cell_ 33, 890–904 (2018). CAS PubMed PubMed Central Google Scholar * Rambow, F. et al. Toward minimal residual
disease-directed therapy in melanoma. _Cell_ 174, 843–855.e19 (2018). CAS PubMed Google Scholar * Fallahi-Sichani, M. et al. Adaptive resistance of melanoma cells to RAF inhibition via
reversible induction of a slowly dividing de-differentiated state. _Mol. Syst. Biol._ 13, 905 (2017). PubMed PubMed Central Google Scholar * Landsberg, J. et al. Melanomas resist T-cell
therapy through inflammation-induced reversible dedifferentiation. _Nature_ 490, 412–416 (2012). CAS PubMed Google Scholar * Offin, M. et al. Concurrent RB1 and TP53 alterations define a
subset of EGFR-mutant lung cancers at risk for histologic transformation and inferior clinical outcomes. _J. Thorac. Oncol._ 14, 1784–1793 (2019). CAS PubMed PubMed Central Google Scholar
* Lee, J. K. et al. Clonal history and genetic predictors of transformation into small-cell carcinomas from lung adenocarcinomas. _J. Clin. Oncol._ 35, 3065–3074 (2017). CAS PubMed
Google Scholar * Aggarwal, R. et al. Clinical and genomic characterization of treatment-emergent small-cell neuroendocrine prostate cancer: a multi-institutional prospective study. _J.
Clin. Oncol._ 36, 2492–2503 (2018). CAS PubMed PubMed Central Google Scholar * Niederst, M. J. et al. RB loss in resistant EGFR mutant lung adenocarcinomas that transform to small-cell
lung cancer. _Nat. Commun._ 6, 6377 (2015). CAS PubMed Google Scholar * Takahashi, K. & Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast
cultures by defined factors. _Cell_ 126, 663–676 (2006). CAS PubMed Google Scholar * Lin, T. et al. p53 induces differentiation of mouse embryonic stem cells by suppressing Nanog
expression. _Nat. Cell Biol._ 7, 165–171 (2005). CAS PubMed Google Scholar * Lim, S. T. et al. Nuclear FAK promotes cell proliferation and survival through FERM-enhanced p53 degradation.
_Mol. Cell_ 29, 9–22 (2008). CAS PubMed PubMed Central Google Scholar * Gastaldi, S. et al. Met signaling regulates growth, repopulating potential and basal cell-fate commitment of
mammary luminal progenitors: implications for basal-like breast cancer. _Oncogene_ 32, 1428–1440 (2013). CAS PubMed Google Scholar * Chiche, A. et al. p53 controls the plasticity of
mammary luminal progenitor cells downstream of Met signaling. _Breast Cancer Res._ 21, 13 (2019). PubMed PubMed Central Google Scholar * Ku, S. Y. et al. Rb1 and Trp53 cooperate to
suppress prostate cancer lineage plasticity, metastasis, and antiandrogen resistance. _Science_ 355, 78–83 (2017). CAS PubMed PubMed Central Google Scholar * Park, J. W. et al.
Reprogramming normal human epithelial tissues to a common, lethal neuroendocrine cancer lineage. _Science_ 362, 91–95 (2018). CAS PubMed PubMed Central Google Scholar * Nakagawa, M.,
Takizawa, N., Narita, M., Ichisaka, T. & Yamanaka, S. Promotion of direct reprogramming by transformation-deficient Myc. _Proc. Natl Acad. Sci. USA_ 107, 14152–14157 (2010). CAS PubMed
PubMed Central Google Scholar * Dardenne, E. et al. N-Myc induces an EZH2-mediated transcriptional program driving neuroendocrine prostate cancer. _Cancer Cell_ 30, 563–577 (2016). CAS
PubMed PubMed Central Google Scholar * Beltran, H. et al. Molecular characterization of neuroendocrine prostate cancer and identification of new drug targets. _Cancer Discov._ 1, 487–495
(2011). CAS PubMed PubMed Central Google Scholar * Beltran, H. et al. Divergent clonal evolution of castration-resistant neuroendocrine prostate cancer. _Nat. Med._ 22, 298–305 (2016).
CAS PubMed PubMed Central Google Scholar * Berger, A. et al. N-Myc-mediated epigenetic reprogramming drives lineage plasticity in advanced prostate cancer. _J. Clin. Invest._ 130,
3924–3940 (2019). Google Scholar * Chen, Z. et al. Diverse AR-V7 cistromes in castration-resistant prostate cancer are governed by HoxB13. _Proc. Natl Acad. Sci. USA_ 115, 6810–6815 (2018).
CAS PubMed PubMed Central Google Scholar * Wang, J. et al. Pim1 kinase synergizes with c-MYC to induce advanced prostate carcinoma. _Oncogene_ 29, 2477–2487 (2010). CAS PubMed PubMed
Central Google Scholar * Ellwood-Yen, K. et al. Myc-driven murine prostate cancer shares molecular features with human prostate tumors. _Cancer Cell_ 4, 223–238 (2003). CAS PubMed Google
Scholar * Kim, J. et al. A mouse model of heterogeneous, c-MYC-initiated prostate cancer with loss of Pten and p53. _Oncogene_ 31, 322–332 (2012). CAS PubMed Google Scholar * Farrell,
A. S. et al. MYC regulates ductal-neuroendocrine lineage plasticity in pancreatic ductal adenocarcinoma associated with poor outcome and chemoresistance. _Nat. Commun._ 8, 1728 (2017).
PubMed PubMed Central Google Scholar * Chen, Y. et al. ETS factors reprogram the androgen receptor cistrome and prime prostate tumorigenesis in response to PTEN loss. _Nat. Med._ 19,
1023–1029 (2013). CAS PubMed PubMed Central Google Scholar * Lee, D. K. et al. Neuroendocrine prostate carcinoma cells originate from the p63-expressing basal cells but not the
pre-existing adenocarcinoma cells in mice. _Cell Res._ 29, 420–422 (2019). PubMed PubMed Central Google Scholar * Yao, J. C. et al. Everolimus for advanced pancreatic neuroendocrine
tumors. _N. Engl. J. Med._ 364, 514–523 (2011). CAS PubMed PubMed Central Google Scholar * Schaefer, T. & Lengerke, C. SOX2 protein biochemistry in stemness, reprogramming, and
cancer: the PI3K/AKT/SOX2 axis and beyond. _Oncogene_ 2, 278–292 (2019). Google Scholar * Rudin, C. M. et al. Comprehensive genomic analysis identifies SOX2 as a frequently amplified gene
in small-cell lung cancer. _Nat. Genet._ 44, 1111–1116 (2012). CAS PubMed PubMed Central Google Scholar * Bass, A. J. et al. SOX2 is an amplified lineage-survival oncogene in lung and
esophageal squamous cell carcinomas. _Nat. Genet._ 41, 1238–1242 (2009). CAS PubMed PubMed Central Google Scholar * Mu, P. et al. SOX2 promotes lineage plasticity and antiandrogen
resistance in TP53- and RB1-deficient prostate cancer. _Science_ 355, 84–88 (2017). CAS PubMed PubMed Central Google Scholar * Bhattaram, P. et al. Organogenesis relies on SoxC
transcription factors for the survival of neural and mesenchymal progenitors. _Nat. Commun._ 1, 9 (2010). PubMed Google Scholar * Sock, E. et al. Gene targeting reveals a widespread role
for the high-mobility-group transcription factor Sox11 in tissue remodeling. _Mol. Cell. Biol._ 24, 6635–6644 (2004). CAS PubMed PubMed Central Google Scholar * Mosquera, J. M. et al.
Concurrent AURKA and MYCN gene amplifications are harbingers of lethal treatment-related neuroendocrine prostate cancer. _Neoplasia_ 15, 1–10 (2013). CAS PubMed PubMed Central Google
Scholar * Gong, X. et al. Aurora A kinase inhibition is synthetic lethal with loss of the RB1 tumor suppressor gene. _Cancer Discov._ 9, 248–263 (2019). CAS PubMed Google Scholar * Oser,
M. G. et al. Cells lacking the RB1 tumor suppressor gene are hyperdependent on Aurora B kinase for survival. _Cancer Discov._ 9, 230–247 (2019). CAS PubMed Google Scholar * Kim, J. et
al. FOXA1 inhibits prostate cancer neuroendocrine differentiation. _Oncogene_ 36, 4072–4080 (2017). CAS PubMed PubMed Central Google Scholar * Adams, E. J. et al. FOXA1 mutations alter
pioneering activity, differentiation and prostate cancer phenotypes. _Nature_ 571, 408–412 (2019). CAS PubMed PubMed Central Google Scholar * Barbieri, C. E. et al. Exome sequencing
identifies recurrent SPOP, FOXA1 and MED12 mutations in prostate cancer. _Nat. Genet._ 44, 685–689 (2012). CAS PubMed PubMed Central Google Scholar * Robinson, D. et al. Integrative
clinical genomics of advanced prostate cancer. _Cell_ 162, 454 (2015). CAS PubMed Google Scholar * Blee, A. M. et al. TMPRSS2-ERG controls luminal epithelial lineage and antiandrogen
sensitivity in PTEN and TP53-mutated prostate cancer. _Clin. Cancer Res._ 24, 4551–4565 (2018). CAS PubMed PubMed Central Google Scholar * McGranahan, N. et al. Clonal status of
actionable driver events and the timing of mutational processes in cancer evolution. _Sci. Transl Med._ 7, 283ra254 (2015). Google Scholar * Sequist, L. V. et al. Genotypic and histological
evolution of lung cancers acquiring resistance to EGFR inhibitors. _Sci. Transl Med._ 3, 75ra26 (2011). PubMed PubMed Central Google Scholar * Beltran, H. et al. The initial detection
and partial characterization of circulating tumor cells in neuroendocrine prostate cancer. _Clin. Cancer Res._ 22, 1510–1519 (2016). CAS PubMed Google Scholar * Roca, E. et al. Outcome of
patients with lung adenocarcinoma with transformation to small-cell lung cancer following tyrosine kinase inhibitors treatment: a systematic review and pooled analysis. _Cancer Treat. Rev._
59, 117–122 (2017). CAS PubMed Google Scholar * Marcoux, N. et al. EGFR-mutant adenocarcinomas that transform to small-cell lung cancer and other neuroendocrine carcinomas: clinical
outcomes. _J. Clin. Oncol._ 37, 278–285 (2019). CAS PubMed Google Scholar * Foster, N. R. et al. Tumor response and progression-free survival as potential surrogate endpoints for overall
survival in extensive stage small-cell lung cancer: findings on the basis of North Central Cancer Treatment Group trials. _Cancer_ 117, 1262–1271 (2011). PubMed Google Scholar * Jiang, S.
Y. et al. Small-cell lung cancer transformation in patients with pulmonary adenocarcinoma: a case report and review of literature. _Medicine_ 95, e2752 (2016). PubMed PubMed Central Google
Scholar * Soo, R. A. et al. Immune checkpoint inhibitors in epidermal growth factor receptor mutant non-small cell lung cancer: current controversies and future directions. _Lung Cancer_
115, 12–20 (2018). PubMed Google Scholar * Davies, A. H., Beltran, H. & Zoubeidi, A. Cellular plasticity and the neuroendocrine phenotype in prostate cancer. _Nat. Rev. Urol._ 15,
271–286 (2018). CAS PubMed Google Scholar * Shah, R. B. et al. Androgen-independent prostate cancer is a heterogeneous group of diseases: lessons from a rapid autopsy program. _Cancer
Res._ 64, 9209–9216 (2004). CAS PubMed Google Scholar * Turbat-Herrera, E. A. et al. Neuroendocrine differentiation in prostatic carcinomas. A retrospective autopsy study. _Arch. Pathol.
Lab. Med._ 112, 1100–1105 (1988). CAS PubMed Google Scholar * Gilani, S., Guo, C. C., Li-Ning, E. M., Pettaway, C. & Troncoso, P. Transformation of prostatic adenocarcinoma to
well-differentiated neuroendocrine tumor after hormonal treatment. _Hum. Pathol._ 64, 186–190 (2017). PubMed Google Scholar * Volta, A. D. et al. Transformation of prostate adenocarcinoma
into small-cell neuroendocrine cancer under androgen deprivation therapy: much is achieved but more information is needed. _J. Clin. Oncol._ 37, 350–351 (2019). CAS PubMed Google Scholar
* Aparicio, A. M. et al. Platinum-based chemotherapy for variant castrate-resistant prostate cancer. _Clin. Cancer Res._ 19, 3621–3630 (2013). CAS PubMed PubMed Central Google Scholar *
Flechon, A. et al. Phase II study of carboplatin and etoposide in patients with anaplastic progressive metastatic castration-resistant prostate cancer (mCRPC) with or without neuroendocrine
differentiation: results of the French Genito-Urinary Tumor Group (GETUG) P01 trial. _Ann. Oncol._ 22, 2476–2481 (2011). CAS PubMed Google Scholar * Papandreou, C. N. et al. Results of a
phase II study with doxorubicin, etoposide, and cisplatin in patients with fully characterized small-cell carcinoma of the prostate. _J. Clin. Oncol._ 20, 3072–3080 (2002). CAS PubMed
Google Scholar * Shukuya, T. et al. Efficacy of gefitinib for non-adenocarcinoma non-small-cell lung cancer patients harboring epidermal growth factor receptor mutations: a pooled analysis
of published reports. _Cancer Sci._ 102, 1032–1037 (2011). CAS PubMed Google Scholar * Park, S., Han, J. & Sun, J. M. Histologic transformation of ALK-rearranged adenocarcinoma to
squamous cell carcinoma after treatment with ALK inhibitor. _Lung Cancer_ 127, 66–68 (2019). PubMed Google Scholar * Gong, J. et al. Squamous cell transformation of primary lung
adenocarcinoma in a patient with EML4-ALK fusion variant 5 refractory to ALK inhibitors. _J. Natl Compr. Canc. Netw._ 17, 297–301 (2019). CAS PubMed Google Scholar * Scagliotti, G. et al.
The differential efficacy of pemetrexed according to NSCLC histology: a review of two phase III studies. _Oncologist_ 14, 253–263 (2009). CAS PubMed Google Scholar * Izumi, H. et al.
Squamous cell carcinoma transformation from EGFR-mutated lung adenocarcinoma: a case report and literature review. _Clin. Lung Cancer_ 19, e63–e66 (2018). PubMed Google Scholar * Balanis,
N. G. et al. Pan-cancer convergence to a small-cell neuroendocrine phenotype that shares susceptibilities with hematological malignancies. _Cancer Cell_ 36, 17–34 (2019). CAS PubMed PubMed
Central Google Scholar * Fujita, S., Masago, K., Katakami, N. & Yatabe, Y. Transformation to SCLC after treatment with the ALK inhibitor alectinib. _J. Thorac. Oncol._ 11, e67–e72
(2016). PubMed Google Scholar * Balla, A., Khan, F., Hampel, K. J., Aisner, D. L. & Sidiropoulos, N. Small-cell transformation of ALK-rearranged non-small-cell adenocarcinoma of the
lung. _Cold Spring Harb. Mol. Case Stud._ 4, a002394 (2018). PubMed PubMed Central Google Scholar * Le, X. et al. De novo pulmonary small cell carcinomas and large cell neuroendocrine
carcinomas harboring EGFR mutations: lack of response to EGFR inhibitors. _Lung Cancer_ 88, 70–73 (2015). PubMed Google Scholar * Schartinger, V. H. et al. Neuroendocrine differentiation
in head and neck squamous cell carcinoma. _J. Laryngol. Otol._ 126, 1261–1270 (2012). CAS PubMed Google Scholar * Yamagata, K. et al. A case of primary combined squamous cell carcinoma
with neuroendocrine (atypical carcinoid) tumor in the floor of the mouth. _Case Rep. Dent._ 2016, 7532805 (2016). PubMed PubMed Central Google Scholar * Mangum, M. D., Greco, F. A.,
Hainsworth, J. D., Hande, K. R. & Johnson, D. H. Combined small-cell and non-small-cell lung cancer. _J. Clin. Oncol._ 7, 607–612 (1989). CAS PubMed Google Scholar * Rudin, C. M. et
al. Molecular subtypes of small cell lung cancer: a synthesis of human and mouse model data. _Nat. Rev. Cancer_ 19, 289–297 (2019). CAS PubMed PubMed Central Google Scholar * Moriguchi,
S. et al. Transformation of epidermal growth factor receptor T790M mutation-positive adenosquamous carcinoma of the lung to small cell carcinoma and large-cell neuroendocrine carcinoma
following osimertinib therapy: an autopsy case report. _Respirol. Case Rep._ 7, e00402 (2019). PubMed PubMed Central Google Scholar * Priftakis, D., Kritikos, N., Stavrinides, S.,
Kleanthous, S. & Baziotis, N. Neuroendocrine differentiation in castration-resistant prostate cancer: a case report. _Mol. Clin. Oncol._ 3, 1392–1394 (2015). PubMed PubMed Central
Google Scholar * Gluck, G., Mihai, M., Stoica, R., Andrei, R. & Sinescu, I. Prostate cancer with neuroendocrine differentiation — case report. _J. Med. Life_ 5, 101–104 (2012). CAS
PubMed PubMed Central Google Scholar * Rudin, C. M. et al. Phase II study of single-agent navitoclax (ABT-263) and biomarker correlates in patients with relapsed small cell lung cancer.
_Clin. Cancer Res._ 18, 3163–3169 (2012). CAS PubMed PubMed Central Google Scholar * Puca, L. et al. Delta-like protein 3 expression and therapeutic targeting in neuroendocrine prostate
cancer. _Sci. Transl Med._ 11, eaav0891 (2019). PubMed PubMed Central Google Scholar * Saunders, L. R. et al. A DLL3-targeted antibody-drug conjugate eradicates high-grade pulmonary
neuroendocrine tumor-initiating cells in vivo. _Sci. Transl Med._ 7, 302ra136 (2015). PubMed PubMed Central Google Scholar * Rudin, C. M. et al. Rovalpituzumab tesirine, a DLL3-targeted
antibody-drug conjugate, in recurrent small-cell lung cancer: a first-in-human, first-in-class, open-label, phase 1 study. _Lancet Oncol._ 18, 42–51 (2017). CAS PubMed Google Scholar *
Takagi, S. et al. LSD1 inhibitor T-3775440 inhibits SCLC cell proliferation by disrupting LSD1 interactions with SNAG domain proteins INSM1 and GFI1B. _Cancer Res._ 77, 4652–4662 (2017). CAS
PubMed Google Scholar * Asangani, I. A. et al. Therapeutic targeting of BET bromodomain proteins in castration-resistant prostate cancer. _Nature_ 510, 278–282 (2014). CAS PubMed
PubMed Central Google Scholar * Aggarwal, R. R. et al. Whole-genome and transcriptional analysis of treatment-emergent small-cell neuroendocrine prostate cancer demonstrates intraclass
heterogeneity. _Mol. Cancer Res._ 17, 1235–1240 (2019). CAS PubMed PubMed Central Google Scholar Download references ACKNOWLEDGEMENTS The authors’ work is supported by grants from the US
National Institutes of Health, including U24CA213274 and R01CA197936 (to C.M.R.). AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Medicine, Thoracic Oncology Service, Memorial
Sloan Kettering Cancer Center, New York, NY, USA Álvaro Quintanal-Villalonga, Joseph M. Chan, Helena A. Yu, Triparna Sen & Charles M. Rudin * Program for Computational and Systems
Biology, Sloan Kettering Institute, Memorial Sloan Kettering Cancer Center, New York, NY, USA Joseph M. Chan & Dana Pe’er * Parker Institute for Cancer Immunotherapy, Memorial Sloan
Kettering Cancer Center, New York, NY, USA Joseph M. Chan & Dana Pe’er * Human Oncology and Pathogenesis Program, Memorial Sloan Kettering Cancer Center, New York, NY, USA Charles L.
Sawyers * Howard Hughes Medical Institute, Chevy Chase, MD, USA Charles L. Sawyers Authors * Álvaro Quintanal-Villalonga View author publications You can also search for this author inPubMed
Google Scholar * Joseph M. Chan View author publications You can also search for this author inPubMed Google Scholar * Helena A. Yu View author publications You can also search for this
author inPubMed Google Scholar * Dana Pe’er View author publications You can also search for this author inPubMed Google Scholar * Charles L. Sawyers View author publications You can also
search for this author inPubMed Google Scholar * Triparna Sen View author publications You can also search for this author inPubMed Google Scholar * Charles M. Rudin View author publications
You can also search for this author inPubMed Google Scholar CONTRIBUTIONS A.Q.-V. and J.M.C. researched and drafted the article. H.A.Y., D.P., C.L.S., T.S. and C.M.R. supervised the
content. All authors wrote, reviewed and edited the manuscript before submission. CORRESPONDING AUTHORS Correspondence to Triparna Sen or Charles M. Rudin. ETHICS DECLARATIONS COMPETING
INTERESTS H.A.Y. has been a consultant on oncology drug development for Astellas Pharma, Astra Zeneca, Daiichi, Lilly, Novartis and Pfizer, and is an inventor on a patent application for
pulsatile use of erlotinib to treat or prevent metastases. C.L.S. serves on the board of directors of Novartis, is a co-founder of ORIC Pharmaceuticals and is a co-inventor of enzalutamide
and apalutamide. He is a science adviser to Agios, Beigene, Blueprint, Column Group, Foghorn, Housey Pharma, Nextech, KSQ, Petra and PMV. C.M.R. has been a consultant on oncology drug
development for AbbVie, Amgen, Ascentage, Astra Zeneca, Bristol-Myers Squibb, Celgene, Daiichi Sankyo, Genentech–Roche, Ipsen, Loxo, Pharmamar and Vavotek. He serves on the scientific
advisory boards of Bridge Medicines and Harpoon Therapeutics. The other authors declare no competing interests. ADDITIONAL INFORMATION PEER REVIEW INFORMATION _Nature Reviews Clinical
Oncology_ thanks T. Graeber, M. Wicha and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. PUBLISHER’S NOTE Springer Nature remains neutral with
regard to jurisdictional claims in published maps and institutional affiliations. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Quintanal-Villalonga,
Á., Chan, J.M., Yu, H.A. _et al._ Lineage plasticity in cancer: a shared pathway of therapeutic resistance. _Nat Rev Clin Oncol_ 17, 360–371 (2020). https://doi.org/10.1038/s41571-020-0340-z
Download citation * Accepted: 04 February 2020 * Published: 09 March 2020 * Issue Date: 15 June 2020 * DOI: https://doi.org/10.1038/s41571-020-0340-z SHARE THIS ARTICLE Anyone you share the
following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer
Nature SharedIt content-sharing initiative