Association of vision impairment and blindness with socioeconomic status in adults 50 years and older from alto amazonas, peru
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT OBJECTIVE To determine the relationship between socioeconomic status (SES) and visual impairment (VI) or blindness in the rural Peruvian Amazon, hypothesizing that higher SES would
have a protective effect on the odds of VI or blindness. METHODS In this cross-sectional study of 16 rural communities in the Peruvian Amazon, consenting adults aged ≥ 50 years were
recruited from ~30 randomly selected households per village. Each household was administered a questionnaire and had a SES score constructed using principal components analysis. Blindness
and VI were determined using a ministry of health 3-meter visual acuity card. RESULTS Overall, 207 adults aged ≥ 50 were eligible; 146 (70.5%) completed visual acuity screening and answered
the questionnaire. Of those 146 participants who completed presenting visual acuity screening, 57 (39.0%, 95% CI 30.2–47.1) were classified as visually impaired and 6 (4.1%, 95% CI 0.9–7.3)
as blind. Belonging to the highest SES tercile had a protective effect on VI or blindness (OR 0.29, 95% CI 0.09 to 0.91, _p_ = 0.034), with a linear trend across decreasing levels of SES
(_p_ = 0.019). This observed effect remained significant regardless of how SES groups were assigned. CONCLUSION Belonging to a higher SES group resulted in a lower odds of VI or blindness
compared to those in the lowest SES group. The observation of a dose response provides confidence in the observed association, but causality remains unclear. Blindness prevention programs
could maximize impact by designing activities that specifically target people with lower SES. SIMILAR CONTENT BEING VIEWED BY OTHERS ASSOCIATION OF VISUAL IMPAIRMENT WITH DISABILITY: A
POPULATION-BASED STUDY Article 17 March 2021 THE PREVALENCE OF VISION IMPAIRMENT AND BLINDNESS AMONG OLDER ADULTS IN INDIA: FINDINGS FROM THE LONGITUDINAL AGEING STUDY IN INDIA Article 07
November 2022 SOCIOECONOMIC AND PHYSICAL HEALTH STATUS CHANGES AFTER VISUAL IMPAIRMENT IN KOREA USING DIFFERENCE-IN-DIFFERENCE ESTIMATIONS Article Open access 08 March 2021 INTRODUCTION
Overall, 405 million people worldwide are estimated to live with visual impairment (VI), 76% of whom suffer from a treatable or preventable cause, with the majority living in low-income
countries with minimal access to detection and treatment [1, 2]. Socioeconomic status (SES) has been associated with a variety of adverse visual outcomes, including VI [3, 4], and this
relationship is accentuated in rural areas [5, 6]. While some studies on the prevalence of VI and its associated risk factors have been conducted in the Brazilian Amazon, few studies exist
for Peru and fewer still have examined the association between SES and VI [7,8,9]. Furthermore, many of the existing studies failed to use a composite, asset-based measure of SES. Low SES
might be expected to have a particular impact on health outcomes in the Peruvian Amazon, given the remoteness of communities and relative inaccessibility of eye care. In this study, we
sought to determine the relationship between SES and VI in the Alto Amazonas region of Peru, hypothesizing that higher SES would have a protective effect on the odds of VI and blindness.
MATERIALS AND METHODS STUDY DESIGN AND SETTING Peru is organized into 26 regions, which are further subdivided into provinces and districts. Alto Amazonas is one of eight provinces in the
region of Loreto, covering 18,764 km2 and containing a population of 122,725 in its six districts (i.e., Balsapuerto, Lagunas, Santa Cruz, Jeberos, Teniente César López Rojas, and
Yurimaguas) [10]. Supplementary Fig. 1 depicts the study location within Peru and the location of study villages, other villages, and optometrists or ophthalmologists offices. According to
the 2017 census, 83,584 (68.1%) of the total population was urban and 12,756 (15.1%) of those 12 years old and above identified as indigenous [10]. A 2018 report by Peru’s National Institute
of Statistics and Informatics found that out of the 1,874 districts in Peru, Balsapuerto ranked as the 249th poorest district, Lagunas as the 578th, Santa Cruz as the 580th, Jeberos as the
878th, Teniente César López Rojas as the 978th, and Yurimaguas as the 1031st. The proportion of the population living below the poverty line ranged from 44.3 to 62.5% in Balsapuerto and 27.6
to 35.9% in Yurimaguas. For comparison, the Iquitos district, containing the capital city of the Loreto region, was ranked 1752nd with 6.7–10.6% of the population below the poverty line
while the Miraflores district in Lima was ranked 1873rd with 0.0–0.2% of the population below the poverty line [11]. In this cross-sectional study, 22 communities, defined as settlements of
100 people or more [12], in the Alto Amazonas region of Peru were randomly selected from a sampling frame of 105 communities for participation in a trachoma prevalence survey using
probability-proportional-to-size sampling after excluding urban areas (i.e., the capital city of each district and the district of Yurimaguas, given the expected low burden of trachoma in
urban areas) [13, 14]. In addition to collecting data on trachoma, visual acuity in adults 50 years and older was measured in order to leverage the effort necessary to reach these areas.
After field testing the visual acuity procedures in several communities during the first round of fieldwork, the subsequent 16 communities were selected for this sub-study. Within each
village, ~30 randomly selected households were visited and all adults 50 years and older within the household invited to participate. Fieldwork was conducted from January to March of 2021.
The sample size was based on the underlying trachoma prevalence survey and therefore fixed. Assuming (1) 30 households and 180 people aged ≥ 1 year would be surveyed per community, (2) 10%
of the population would be ≥50 years (i.e., ~288 people across all communities, and thus 96 per tercile), (3) the prevalence of VI and blindness would be ~20% [9], and (4) an alpha of 0.05,
then the study would provide ~80% power to estimate a 15% or greater difference in the prevalence of blindness or VI between the lowest and highest SES terciles (i.e., 10% vs 25% VI). DATA
COLLECTION Vision was tested in a central location in the village by field workers who had undergone a 1-week training using a Ministry of Health endorsed 3-meter visual acuity card
(Ministerio de Salud, Lima, Peru). The card consists of six lines of tumbling E optotypes of different sizes (corresponding to 20/200, 20/100, 20/70, 20/50, 20/40, and 20/30) (Supplementary
Fig. 2). Individuals were seated 3 meters away from the card in ambient lighting conditions and each eye was tested separately. A successful effort required the correct identification of
half or more of the optotypes in each line. If participants were unable to detect the optotypes, the fieldworker tested them for the ability to read the largest optotype at 1.5 m (i.e.,
20/400), counting fingers (CF) at 1.5 m, hand motion (HM) at 1.5 m, or light perception (LP) at 30 cm. If the participants could not perceive light they were recorded as no LP (NLP).
Participants were first tested with spectacle correction if available (i.e., the World Health Organization [WHO]’s definition of presenting visual acuity), followed by pinhole occlusion over
any correction. Each head of household was administered a socioeconomic survey, with survey items modified from the questions from Peru’s 2012 Demographic and Health Survey, with input from
local health workers and researchers [15]. Since the study was planned for a rural and relatively resource-limited population, the questionnaire focused on asset-based measures to capture
SES instead of information on consumption, expenditure, or income [16, 17]. DEFINITIONS AND CONVENTIONS Visual acuity for the better seeing eye was used in all analyses, categorized
according to the WHO’s International Classification of Disease [18]. Individuals with visual acuity worse than 20/60 up to 20/400 were considered visually impaired, with individuals scoring
20/70, 20/100, and 20/200 considered moderately visually impaired, and those scoring 20/400 considered severely visually impaired. Those scoring worse than 20/400 (i.e., CF, HM, LP, NLP)
were considered blind. A principal components analysis (PCA) was used to construct a SES index for each household. As PCA works best when asset variables exhibit varied distribution across
households, assets owned by all or no households were removed. Multilevel categorical SES variables were dichotomized (e.g., type of floor converted into presence or absence of wooden floor,
dirt floor, or brick floor). The statistical methods used to convert survey questions into a SES score have been described elsewhere [19]. The PCA in this study was conducted via singular
value decomposition of the centered and scaled data-matrix in order to account for differences in the units of measurement for each variable (e.g., quantitative variables like number of
birds were given equal weight as binary ownership variables). The first principal component score for each household was assumed to be a measure of SES and was standardized to a mean of 0
and standard deviation of 1. The households were then grouped into socioeconomic terciles, assigning the top third of households to the highest tercile, the lowest third to the lowest
tercile, and the remaining third to the middle tercile. Other thresholds for grouping SES were explored in sensitivity analyses. STATISTICAL CONSIDERATIONS The exposure of interest was
socioeconomic tercile and the outcome was presenting VI or blindness. The relationship between SES tercile and presenting VI or blindness was assessed with an age- and sex-adjusted mixed
effects logistic regression model with a random intercept for community to account for community-level clustering. A similar model was constructed for pinhole VI (i.e., VI or blindness in
the better seeing eye with pinhole occlusion). Age was treated as a continuous variable in all models. Missing SES data from 39 participants, most of whom were missing only one (_N_ = 19) or
two (_N_ = 9) fields, were imputed using the data interpolating empirical orthogonal functions approach, which has been described elsewhere [20]. In sensitivity analyses, prevalence ratios
(PR) were calculated using a modified Poisson approach with robust standard errors [21]. A significance level of 0.05 was chosen for all analyses given the exploratory nature of this
observational study. All analyses were performed with R version 3.6.0 (R Foundation for Statistical Computing, Vienna, Austria). ETHICS The study adhered to the guidelines of the Declaration
of Helsinki and received ethical approval from the University of California San Francisco (reference number: 247252), Universidad Peruana Cayetano Heredia (reference number: 104344), and
the Pan American Health Organization (reference number: PAHOERC.0145.03). Written informed consent was obtained for all participants; no stipend was provided. RESULTS Overall, 207 adults ≥
50 years were eligible for inclusion; 146 (70.5%) completed visual acuity screening and answered the SES questionnaire. There was no evidence of differences between participants and
non-participants in terms of sex or age (_p_ value for sex = 0.848; _p_ value for age = 0.640). Of the 146 participants who completed presenting visual acuity screening, 57 (39.0%, 95% CI
30.2–47.1) were classified as visually impaired (_N_ = 54 with moderate VI [i.e., visual acuity of 20/70, 20/100, and 20/200 in the better seeing eye] and _N_ = 3 with severe VI [i.e.,
visual acuity of 20/400 in the better seeing eye]) and 6 (4.1%, 95% CI 0.9–7.3) as blind (i.e., visual acuity worse than 20/400 in the better seeing eye). Of the 146 participants who
completed pinhole visual acuity screening, 40 (27.4%, 95% CI 19.3–34.6) were visually impaired (_N_ = 38 with moderate VI and N = 2 with severe VI) and 6 (4.1%, 95% CI 0.9–7.3%) blind.
Aggregated results for each of the survey questions after dichotomization are provided in Supplementary Table 1. When categorized into terciles, the middle and lowest SES terciles had a
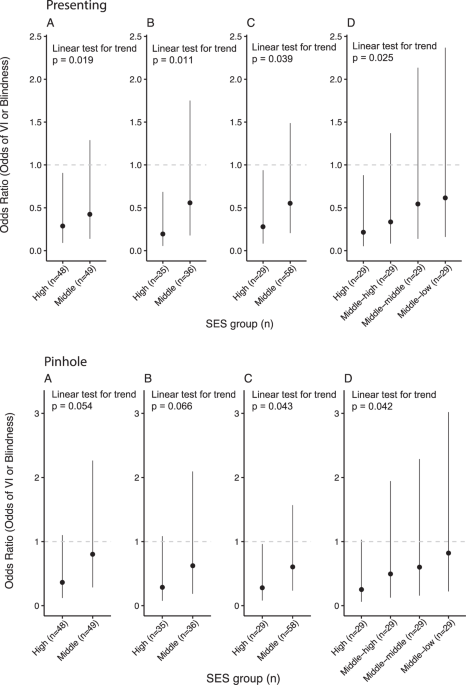
higher percentage of individuals with both presenting and pinhole VI compared to the highest tercile (Table 1). The results of the age- and sex-adjusted mixed-effect logistic regression
models for presenting VI and blindness are depicted in Fig. 1. The model found that those in the highest SES tercile had 0.29 the odds of being blind or visually impaired relative to those
in the lowest SES tercile (95% CI 0.09–0.91, _p_ = 0.034). Those in the middle SES tercile also had lower odds of blindness or VI compared to the lowest SES tercile, although the
relationship did not achieve predetermined statistical significance (OR 0.42, 95% CI 0.14–1.29, _p_ = 0.130). Conclusions did not change when analyses were repeated without imputing missing
variables (OR 0.19 comparing highest to lowest SES tercile, 95% CI 0.06–0.67, _p_ = 0.011). Sensitivity analyses found a similar relationship between SES and VI using other common thresholds
to segment individuals into SES groups [19, 22, 23]. Specifically, similar regression models were constructed with socioeconomic groups assigned as: (1) unequal thirds (i.e., 20% in the
highest and 40% in the middle and bottom groups) and (2) equal quintiles (i.e., 20% in each group). The highest SES group had a lower odds of VI or blindness in both unequal SES thirds (OR
0.28, 95% CI 0.08–0.94; _p_ = 0.039) and equal SES quintiles (OR 0.22, 95% CI 0.05–0.88; _p_ = 0.033) relative to the lowest SES group (Fig. 1). In all cases, statistical analyses only
provided strong evidence of a reduced odds in the highest SES group relative to the lowest, although evidence of a linear trend was found when comparing the odds ratios across increasing
levels of SES (Fig. 1; _p_ value for first-order orthogonal polynomial contrast = 0.019 using imputed data and equal SES terciles, _p_ = 0.011 using complete data, _p_ = 0.039 using uneven
SES thirds, and _p_ = 0.025 using SES quintiles). A sensitivity analysis with a modified Poisson regression was consistent with the main results (PR for highest equal tercile relative to
lowest: 0.56, 95% CI 0.38–0.85; _p_ = 0.006). The results of age- and sex-adjusted mixed effects logistic regression models for the pinhole vision outcomes were consistent with the main
analysis, with a similar magnitude of effect but wider confidence intervals and less statistical evidence to support the observed odds ratios and linear trends (Fig. 1). DISCUSSION This
study’s principal finding was that individuals of higher SES had lower odds of presenting VI or blindness relative to the lowest SES group. This effect remained significant regardless of the
thresholds used to segment individuals into SES groups and exhibited a linear dose response, thus strengthening the likelihood of the observed association. We found that approximately 40%
of individuals were classified as VI and 4% as blind when using presenting visual acuity. While the present study’s estimates have relatively wide confidence intervals, the observed
prevalence of blindness was similar to a 2005 study in rural northern Peru as well as a 2019 study in the Brazilian Amazon [9, 24]. In contrast, the overall prevalence of blindness in Peru
is ~2% based on a 2014 nationwide survey [25]. Estimates of VI in the present study were generally higher than those of previous studies in Peru and other parts of Latin America [9,
24,25,26,27,28,29,30,31,32]. It is plausible that the more rural and remote areas of Peru, such as this remote part of the Amazon, have a higher burden of VI and blindness given poorer
access to ophthalmic care and fewer government –sponsored vision programs. While we did not investigate the etiology of blindness or VI in our study population, the decrease in the
proportion of individuals with presenting VI after pinhole correction from 39.0 to 24.7% suggests a relatively high burden of uncorrected refractive error in this population, similar to what
has been reported in other parts of Latin America [33,34,35]. Pinhole correction did not change the proportion of blind individuals in the present study and more detailed evaluation of the
etiology of blindness in the region is necessary. Interestingly the magnitude of the effect of SES on pinhole VI or blindness was similar to the main analysis; the wider confidence intervals
and weaker statistical evidence to support the observed odds ratios are likely due to the presence of fewer visually impaired individuals after pinhole correction. Several studies have
looked at the association between VI or blindness and markers of SES. Rius et al. [4] found that illiterate, disabled, and unemployed individuals had significantly higher odds of VI in El
Salvador. An ecological analysis of cross-sectional eye health surveys from seven Latin American countries found a higher prevalence of blindness and moderate VI among the more socially
disadvantaged countries, determined as a composite of educational achievement, literacy, and wealth [34]. Our results agree with these prior studies and increase the rigor of the analysis
through the use of household-level composite SES scores and individual analysis. It is notable that the present study found SES to be correlated with VI even within one the poorest regions
of the country, where the differences between rich and poor may not be as stark as in other places. While level of education could have been used as a proxy for SES, the vast majority (84%)
of adults in the area had completed primary or secondary schooling and thus educational achievement would likely have been less able to classify individuals into different groups compared to
the use of a composite SES score [10]. These studies draw attention to the need for interventions to reduce blindness and VI in the most disadvantaged groups, among whom the burden is
highest. This study is relevant for public health planners in Peru and other countries with very remote populations, since it highlights that VI and blindness appear to be most common in the
very population that has the least financial resources available for diagnosis or treatment. Given the expense and time required to even reach one of these villages in the Amazon, a
blindness prevention program may want to design activities that specifically target those with low SES, who are both most likely to benefit from an intervention and also least likely to be
able to afford an intervention on their own. Although specific activities would undoubtedly need to be adapted to the local context, examples of such interventions include offering
discounted or free spectacles and cataract surgical services, providing education regarding eye diseases and available eye care services, and deploying equitable models of eye health
delivery [36, 37]. Several limitations of the present study should be noted. The cross-sectional nature precluded conclusions about causation, given the possibility of reverse causality. The
individuals who did not complete both visual acuity screening and the questionnaire may have differed systematically and resulted in selection bias, although we found no evidence of a
difference in age or sex between the two groups. SES was calculated at the household level and assumed to apply to all household members equally. Ordinal data on visual acuity were
dichotomized, which reduced statistical power but made for more easily interpretable regression models. The relatively small sample size increased the uncertainty of prevalence estimates.
The small number of blind individuals and their uneven distribution across the socioeconomic groups prevented a separate analysis looking exclusively at the relationship between SES and
blindness. While the sampling schema for the parent trachoma study increased the study’s generalizability within this region of Peru, the generalizability of the findings outside of Alto
Amazonas is not clear; it is possible that SES has a weaker association with VI and blindness in other locations with better access to eye health services. In summary, we found that
belonging to a higher SES group resulted in a lower odds of VI or blindness compared to those in the lowest group, regardless of the manner in which the groups were constructed. The
observation of a linear dose response provides confidence in the observed association, but reverse causality remains a concern. Although studies in other areas of the Amazon basin would be
helpful to assess generalizability, these findings can aid public health planners identify at-risk groups who would benefit the most from ocular health interventions. SUMMARY WHAT WAS KNOWN
BEFORE * SES has been associated with various adverse visual outcomes. This relationship is accentuated in rural areas. To date there exist little data from the Amazon basin. WHAT THIS STUDY
ADDS * This study reports the relationship between VI or blindness and SES in the Peruvian Amazon. It was found that lower SES was associated with higher odds of VI or blindness. DATA
AVAILABILITY The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to their containing information
that could compromise the privacy of research participants. REFERENCES * Bourne RRA, Flaxman SR, Braithwaite T, Cicinelli MV, Das A, Jonas JB, et al. Magnitude, temporal trends, and
projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e888–97. Article Google Scholar
* Bourne RRA, Stevens GA, White RA, Smith JL, Flaxman SR, Price H, et al. Causes of vision loss worldwide, 1990–2010: a systematic analysis. Lancet Glob Health. 2013;1:e339–49. Article
Google Scholar * Zheng Y, Lamoureux E, Finkelstein E, Wu R, Lavanya R, Chua D, et al. Independent impact of area-level socioeconomic measures on visual impairment. Investig Ophthalmol Vis
Sci. 2011;52:8799–805. Article Google Scholar * Rius A, Guisasola L, Sabidó M, Leasher JL, Moriña D, Villalobos A, et al. Prevalence of visual impairment in El Salvador: inequalities in
educational level and occupational status. Rev Panam Salud Publica. 2014;36:290–9. Google Scholar * Yan X, Chen L, Yan H. Socio-economic status, visual impairment and the mediating role of
lifestyles in developed rural areas of China. PLoS ONE. 2019;14:e0215329. Article CAS Google Scholar * Jadoon MZ, Dineen B, Bourne RR, Shah SP, Khan MA, Johnson GJ, et al. Prevalence of
blindness and visual impairment in Pakistan: the Pakistan National Blindness and Visual Impairment Survey. Investig Ophthalmol Vis Sci. 2006;47:4749–55. Article Google Scholar * Watanabe
SES, Berezovsky A, Furtado JM, Kimie Higashi Mitsuhiro MR, Cypel M, Cohen MJ, et al. Population-based cataract surgery complications and their impact on visual status in the Brazilian Amazon
region. Am J Ophthalmol. 2019;208:295–304. Article Google Scholar * Cunha CC, Berezovsky A, Furtado JM, Ferraz NN, Fernandes AG, Muñoz S, et al. Presbyopia and ocular conditions causing
near vision impairment in older adults from the Brazilian Amazon region. Am J Ophthalmol. 2018;196:72–81. Article Google Scholar * Furtado JM, Berezovsky A, Ferraz NN, Muñoz S, Fernandes
AG, Watanabe SS, et al. Prevalence and causes of visual impairment and blindness in adults aged 45 years and older from parintins: the Brazilian Amazon Region Eye Survey. Ophthalmic
Epidemiol. 2019;26:345–54. Article Google Scholar * INEI. Definitive results of 2017 National Census. INEI. https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1561/
2017. * Instituto Nacional de Estadística e Informática. Mapa de pobreza monetaria provincial y distrital 2018. Lima, Perú: Instituto Nacional de Estadística e Informática; 2020. *
OpenStreetMap Wiki contributors. Key: place. OpenStreetMap Wiki; 2019. https://wiki.openstreetmap.org/w/index.php?title=Key:place&oldid=1910053. * Solomon, Anthony W, World Health
Organization, International Trachoma Initiative. Trachoma control: a guide for programme managers. Switzerland: WHO; 2006. * Nesemann J, Muñoz MB, Morocho-Alburqueque N, Quincho-Lopez A,
Wittberg DM, Honorio H, et al. Prevalence of trachoma in Alto Amazonas, Loreto Department, Perú. Investig Ophthalmol Vis Sci. 2021;62:2625. Google Scholar * Instituto Nacional de
EstadÌstica e Informática Perú. Perú Encuesta Demográfica y de Salud Familiar—ENDES 2012. Lima, Perú: INEI; 2013. * McKenzie D. Measuring inequality with asset indicators. J Popul Econ.
2005;18:229–60. Article Google Scholar * Rutstein SO. The DHS wealth index: approaches for rural and urban areas. Calverton, Maryland, USA: Macro International; 2008. * WHO. International
classification of diseases for mortality and morbidity statistics (11th Revision). WHO; 2020. https://icd.who.int/en/. * Vyas S, Kumaranayake L. Constructing socio-economic status indices:
how to use principal components analysis. Health Policy Plan. 2006;21:459–68. Article Google Scholar * Beckers J-M, Rixen M. EOF calculations and data filling from incomplete oceanographic
datasets. J Atmos Ocean Technol. 2003;20:1839–56. Article Google Scholar * Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison
of models that directly estimate the prevalence ratio. BMC Med Res Methodol. 2003;3:21. Article Google Scholar * Filmer D, Pritchett LH. Estimating wealth effects without expenditure
data-or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–32. CAS Google Scholar * Gwatkin DR, Rutstein S, Johnson K, Suliman E, Wagstaff A,
Amouzou A. Socio-economic differences in health, nutrition, and population: Nigeria 1990, 2003. Country reports on HNP and poverty. Washington, DC: World Bank; 2007. * Pongo Aguila L,
Carrión R, Luna W, Silva JC, Limburg H. Cataract blindness in people 50 years old or older in a semirural area of northern Peru. Rev Panam Salud Publica. 2005;17:387–93. Google Scholar *
Campos B, Cerrate A, Montjoy E, Dulanto Gomero V, Gonzales C, Tecse A, et al. National survey on the prevalence and causes of blindness in Peru. Rev Panam Salud Publica. 2014;36:283–9.
Google Scholar * Duerksen R, Limburg H, Carron JE, Foster A. Cataract blindness in Paraguay-results of a national survey. Ophthalmic Epidemiol. 2003;10:349–57. Article Google Scholar *
Beltranena F, Casasola K, Silva JC, Limburg H. Cataract blindness in 4 regions of Guatemala: results of a population-based survey. Ophthalmology. 2007;114:1558–63. Article Google Scholar *
Nano ME, Nano HD, Mugica JM, Silva JC, Montaña G, Limburg H. Rapid assessment of visual impairment due to cataract and cataract surgical services in urban Argentina. Ophthalmic Epidemiol.
2006;13:191–7. Article Google Scholar * Siso F, Esche G, Limburg H. Test nacional de catarata y servicios quirúrgicos “RACSS rapid assesment of cataract and surgical services” primera
encuesta nacional. Rev oftalmol venez. 2005;61:112–39. * Limburg H, von-Bischhoffshausen FB, Gomez P, Silva JC, Foster A. Review of recent surveys on blindness and visual impairment in Latin
America. Br J Ophthalmol. 2008;92:315–9. Article Google Scholar * Barría F, Silva J, Limburg H, Muñoz D, Castillo L, Martínez L, et al. Análisis de la prevalencia de ceguera y sus causas,
determinados mediante encuesta rápida de ceguera evitable (RAAB) en la VIII región, Chile. Chile Arch Chil Oftalmol. 2008;64:69–78. Google Scholar * Hernández Silva JR, Río Torres
M.Padilla González CM, Resultados del RACSS en Ciudad de La Habana, Cuba, 2005. Rev Cubana Oftalmolía. 2006;19:1–9. * Leasher JL, Lansingh V, Flaxman SR, Jonas JB, Keeffe J, Naidoo K, et al.
Prevalence and causes of vision loss in Latin America and the Caribbean: 1990-2010. Br J Ophthalmol. 2014;98:619–28. Article Google Scholar * Silva JC, Mújica OJ, Vega E, Barcelo A,
Lansingh VC, McLeod J, et al. A comparative assessment of avoidable blindness and visual impairment in seven Latin American countries: prevalence, coverage, and inequality. Rev Panam Salud
Publica. 2015;37:13–20. Google Scholar * Salomão SR, Berezovsky A, Furtado JM, Fernandes AG, Muñoz S, Cavascan NN, et al. Vision status in older adults: the Brazilian Amazon Region Eye
Survey. Sci Rep. 2018;8:886. Article Google Scholar * Natchiar G, Robin AL, Thulasiraj RD, Krishnaswamy S. Attacking the backlog of India’s curable blind. The Aravind Eye Hospital model.
Arch Ophthalmol. 1994;112:987–93. Article CAS Google Scholar * Ramke J, Petkovic J, Welch V, Blignault I, Gilbert C, Blanchet K, et al. Interventions to improve access to cataract
surgical services and their impact on equity in low- and middle-income countries. Cochrane Database Syst Rev. 2017;11:Cd011307. Google Scholar Download references ACKNOWLEDGEMENTS The
authors would like to acknowledge all the field workers who did the truly hard work that made the study possible: Jim Bill Oliveira Garay, Técnico en Enfermería; Segundo Rosbel Soria
Saavedra, Técnico en Enfermería; Rider Isaias Pizango Taminchi, Técnico en Enfermería; Hernan Dario Tapayuri Curitima, Técnico en Enfermería; Geiner Armas Damacen, Técnico en Enfermería;
Kike Guevara Alarcón, Técnico Sistema de Información Geográfica; Lester Lenin Vela Tello, Técnico en Enfermería; Abdias Valles Davila, Técnico en Enfermería; Luis Edgar Payaba Pacaya,
Técnico en Producción Agropecuario; Lizandro Guerra Rios, Técnico en Enfermería; Francisco Javier Noriega Morey, Técnico en Enfermería; Jorge Chasnamote Macahuachi, Técnico en Enfermería;
and Gene Lucio Panaifo Garces, Técnico en Enfermería. The authors also thank Edgardo Nepo Linares, MD, as representative of PAHO Peru whose help laid the foundations for this project;
Salvith Karen Melendez Ruiz, RN, and Rosario Avellaneda, RN, for sharing their experience and help in coordinating this project; and Nilda Trejo Maguiña, RN, and Héctor Shimabuku Ysa, MD,
from the technical team of the Ocular Health and Prevention of Blindness department of the Peruvian Ministry of Health, who contributed to the review of the manuscript. FUNDING This project
was supported by the National Eye Institute and the Fogarty International Center of the National Institutes of Health (NIH) under Award Number D43TW009343 as well as the University of
California Global Health Institute (UCGHI) in the form of a Fogarty grant to JMN. The content is solely the responsibility of the authors and does not necessarily represent the official
views of the NIH or UCGHI. Support was also provided by That Man May See and Research to Prevent Blindness. MISD is a staff member of the Pan American Health Organization (PAHO). In any
reproduction of this article, there should be no suggestion that PAHO or this article endorse any specific organization, products or services. The use of PAHO logos is not permitted. This
notice should be preserved along with the article’s original URL. The authors held no agreement with the funders that may have limited their ability to complete the research as planned and
have full control of all primary data. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Francis I. Proctor Foundation, University of California, San Francisco, CA, USA John M. Nesemann &
Jeremy D. Keenan * David Geffen School of Medicine, University of California, Los Angeles, CA, USA John M. Nesemann * Emerge, Emerging Diseases and Climate Change Research Unit, School of
Public Health and Administration, Universidad Peruana Cayetano Heredia, Lima, Peru John M. Nesemann & Andres G. Lescano * Universidad Nacional de Piura, Piura, Peru Noelia
Morocho-Alburqueque * Universidad Nacional Mayor de San Marcos, Lima, Peru Alvaro Quincho-Lopez * Área de Epidemiología, Red de Salud Alto Amazonas, Yurimaguas, Peru Marleny Muñoz * Escuela
Superior de Oftalmología del Instituto Barraquer de América, Bogotá, Colombia Sandra Liliana-Talero * Clinical Research Department, London School of Hygiene & Tropical Medicine, London,
UK Emma M. Harding-Esch * Department of Communicable Diseases and Environmental Determinants of Health, Pan American Health Organization, Washington, DC, USA Martha Idalí Saboyá-Díaz *
Componente de Salud Ocular y Prevención de la Ceguera, Ministerio de Salud, Lima, Peru Harvy A. Honorio-Morales * Área de Epidemiología, Dirección Regional de Salud Loreto, Iquitos, Peru
Salomón Durand * Universidad Nacional de la Amazonia Peruana, Iquitos, Peru Cristiam A. Carey-Angeles * Department of Population and Public Health Sciences, Keck School of Medicine,
University of Southern California, Los Angeles, CA, USA Jeffrey D. Klausner * Department of Ophthalmology, University of California, San Francisco, CA, USA Jeremy D. Keenan Authors * John M.
Nesemann View author publications You can also search for this author inPubMed Google Scholar * Noelia Morocho-Alburqueque View author publications You can also search for this author
inPubMed Google Scholar * Alvaro Quincho-Lopez View author publications You can also search for this author inPubMed Google Scholar * Marleny Muñoz View author publications You can also
search for this author inPubMed Google Scholar * Sandra Liliana-Talero View author publications You can also search for this author inPubMed Google Scholar * Emma M. Harding-Esch View author
publications You can also search for this author inPubMed Google Scholar * Martha Idalí Saboyá-Díaz View author publications You can also search for this author inPubMed Google Scholar *
Harvy A. Honorio-Morales View author publications You can also search for this author inPubMed Google Scholar * Salomón Durand View author publications You can also search for this author
inPubMed Google Scholar * Cristiam A. Carey-Angeles View author publications You can also search for this author inPubMed Google Scholar * Jeffrey D. Klausner View author publications You
can also search for this author inPubMed Google Scholar * Andres G. Lescano View author publications You can also search for this author inPubMed Google Scholar * Jeremy D. Keenan View
author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS Concept and design: JMN, JDKeenan, JDKlausner, and AGL. Acquisition, analysis, or interpretation
of data and critical revision of the manuscript for important intellectual content: all authors. Drafting of the manuscript: JMN and JDKeenan. Administrative, technical, or material
support: MM, SLT, EMHE, MISD, MAHM, SD, CACA, JDKlausner, AGL, and JDKeenan. Supervision: MM, JDKeenan, JDKlausner, and AGL. CORRESPONDING AUTHOR Correspondence to John M. Nesemann. ETHICS
DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in
published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTAL FIGURE AND TABLE LEGENDS SUPPLEMENTAL FIGURE 1 SUPPLEMENTAL FIGURE 2 SUPPLEMENTAL TABLE 1 RIGHTS AND
PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any
medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The
images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not
included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly
from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Nesemann, J.M.,
Morocho-Alburqueque, N., Quincho-Lopez, A. _et al._ Association of vision impairment and blindness with socioeconomic status in adults 50 years and older from Alto Amazonas, Peru. _Eye_ 37,
434–439 (2023). https://doi.org/10.1038/s41433-021-01870-x Download citation * Received: 10 May 2021 * Revised: 12 November 2021 * Accepted: 19 November 2021 * Published: 03 February 2022 *
Issue Date: February 2023 * DOI: https://doi.org/10.1038/s41433-021-01870-x SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link
Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative