To extract or not to extract: examining the referrals for third molar removal
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
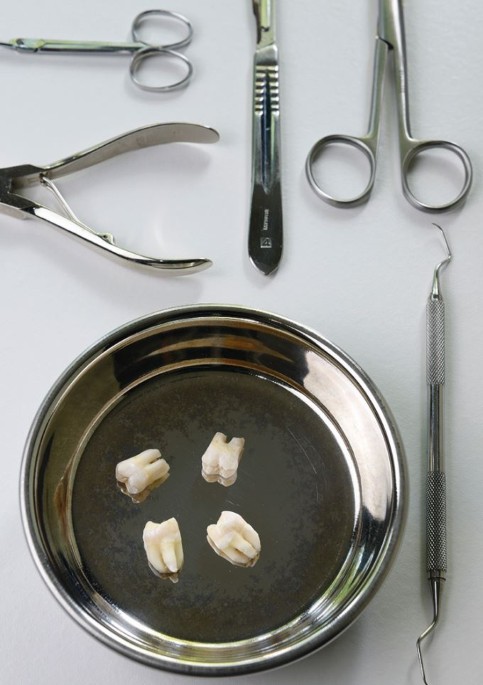
You have full access to this article via your institution. Download PDF Mackie L, Wong-McDermott R, Bell G W. An evaluation of referrals requesting third molar tooth removal: clinical
diagnosis and treatment outcome. _Br Dent J_ 2019; 226: 577-580. DOI: https://doi.org/10.1038/s41415-019-0199-5. Despite dentistry being considered an objective field in health care, there
are high levels of subjectivity that exist within it. This rings especially true when it comes to the management of third molars, a topic which has long been the subject of debate in the
profession. Problematic third molars are one of the most common developmental conditions that a practitioner can come across and their surgical removal are among the most frequently
performed procedures undertaken within the NHS. Taking this into consideration, it is therefore vital that practitioners are well educated in the management of these cases. This study aims
to assess exactly that and whether the changes in recommendations brought about by published guidelines and research have actually been integrated into practice. Referrals to a secondary
care service were prospectively analysed over the course of 20 months with respect to reason for referral, clinical diagnosis and treatment outcome. One of the most striking findings was
that 17.5% of referrals did not actually require the extraction of the third molars, highlighting how common misdiagnosis is in primary practice. The study also found that, despite caries
being a growing reason for the extraction of third molars, temporomandibular disorders (TMD) should not be overlooked as a diagnosis, presenting in 18.7% of the cases. Significantly, out of
the teeth that did not proceed to extraction, over half were due to a diagnosis of TMD where there were no signs that the third molar teeth had been affected. Perhaps what was most
concerning, however, was that there were numerous incidences of patients being prescribed antibiotics in the treatment of orofacial pain with no clinical indications such as pyrexia,
bleeding or discharge to do so. Some practitioners appeared to have an inclination of attributing the cause of orofacial pain that the patient was experiencing to impacted or unerupted molar
teeth in the absence of relevant symptoms. This was combated in secondary care by asking the patient to describe their symptoms in their own words rather than depending on the referral.
Evidently, a disconnect seems to exist between theoretical knowledge and practical applications in the management of third molars. Unnecessary referrals are both costly to the healthcare
system and not in the best interest of patients, especially those who are suffering from chronic orofacial pain. To overcome this, practitioners need to ensure that they are well acquainted
with the appropriate diagnostic criteria, guidelines and treatment planning. Perhaps we need to spend some more time extracting the correct diagnosis from the patient before we start
extracting their teeth. BY AREFEH AHMADIFARD AUTHOR Q&A Q: WHY DID YOU DECIDE TO UNDERTAKE THIS STUDY? We were intrigued by the number of referrals requesting removal of third molar
teeth, especially when the third molars were disease free and patients' symptoms were attributable to other causes. Q: DID ANY OF THE RESULTS SURPRISE YOU? Yes, greater than one in ten
patient referrals resulted in a primary diagnosis of temporomandibular disorders, with no disease affecting the third molars and no surgery being required. Almost one in five patients did
not require removal of, or fulfil current guidelines for removal of third molar teeth. Almost one in five patients received a diagnosis of temporomandibular disorders as a primary, secondary
or tertiary diagnosis. We realised the importance of pre-operative discussion in relation to the nature of chronic orofacial pain in those patients that proceeded to have third molar teeth
removed, but who also had a diagnosis of temporomandibular disorders, the symptoms of which would not be influenced by surgery. Q: WHAT DO YOU THINK THE NEXT STEPS SHOULD BE CONSIDERING YOUR
FINDINGS? Raising awareness of the prevalence and nature of chronic orofacial pain not just within primary and secondary care but also among patients is essential. Education to enable
accurate diagnosis and evidence-based management is of paramount importance. Orofacial pain and headache are diagnosed and managed by both medical and dental general practitioners.
Empowering both groups with the skills and resources to manage such is crucial. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE To extract or not to
extract: examining the referrals for third molar removal. _Br Dent J_ 226, 856 (2019). https://doi.org/10.1038/s41415-019-0424-2 Download citation * Published: 14 June 2019 * Issue Date:
June 2019 * DOI: https://doi.org/10.1038/s41415-019-0424-2 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a
shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative