Impact of anti-t-lymphocyte globulin dosing on gvhd and immune reconstitution in matched unrelated myeloablative peripheral blood stem cell transplantation
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT Data on the influence of different Anti-lymphocyte globulin (ATLG) doses on graft versus host disease (GVHD) incidence and immune reconstitution in matched unrelated (MUD)
allogeneic Stem cell transplantation (allo-SCT) is limited. This retrospective study conducted at the University Medical-Center Hamburg compares GVHD and Immune reconstitution after
myeloablative MUD (HLA 10/10) PBSC allogeneic stem cell transplant between 30 mg/Kg (_n_ = 73) and 60 mg/Kg (_n_ = 216) ATLG. Detailed phenotypes of T, B natural killer (NK), natural killer
T (NKT) cells were analyzed by multicolor flow at day 30, 100, and 180 posttransplant. Neutrophil and platelet engraftments were significantly delayed in the 60 mg/kg group with a higher
Cumulative incidence of Infections (67% vs 75% _p_ = 0.049) and EBV (21% vs 41% _p_ = 0.049) reactivation at day 100 in this group. In the 30 mg/kg group, we observed a faster reconstitution
of naïve-B cells (_p_ < 0.0001) and γδ T cells (_p_ = 0.045) at day+30 and a faster naïve helper T-cell (_p_ = 0.046), NK-cells (_p_ = 0.035), and naïve B-cell reconstitution (_p_ =
0.009) at day+180. There were no significant differences in aGVHD, cGVHD, NRM, RI, PFS, and OS between the groups. The choice of ATLG dose has significant impact on IR but not on GVHD after
MUD-allo-SCT. Higher doses are associated with delayed engraftment and increased infections. SIMILAR CONTENT BEING VIEWED BY OTHERS IMMUNOLOGICAL RECONSTITUTION AND INFECTIONS AFTER ALLOHCT
- A COMPARISON BETWEEN POST-TRANSPLANTATION CYCLOPHOSPHAMIDE, ATLG AND NON-ATLG BASED GVHD PROPHYLAXIS Article Open access 19 November 2024 LONG-TERM RESULTS AND GVHD AFTER PROPHYLACTIC AND
PREEMPTIVE DONOR LYMPHOCYTE INFUSION AFTER ALLOGENEIC STEM CELL TRANSPLANTATION FOR ACUTE LEUKEMIA Article Open access 08 November 2021 THE ROLE OF ANTI-THYMOCYTE GLOBULIN IN ALLOGENEIC STEM
CELL TRANSPLANTATION (HSCT) FROM HLA-MATCHED UNRELATED DONORS (MUD) FOR SECONDARY AML IN REMISSION: A STUDY FROM THE ALWP /EBMT Article 02 September 2023 INTRODUCTION Due to the graft
versus tumor effect, allogeneic stem cell transplantation (allo-SCT) is a potentially curative treatment strategy for hematological diseases [1, 2]. However its benefits may be offset by
increased non related mortality (NRM), mainly due graft-versus-host-disease (GVHD) and infections [3]. The use of an unrelated donor and peripheral blood stem cells (PBSC) is associated with
an increased risk of GVHD. Randomized studies have shown that pretransplant anti-T-Lymphocyte globulin (ATLG) can prevent severe acute and chronic GVHD [4,5,6]. Although lower ATLG doses
may compromise the immunosuppression effects, higher ATLG doses may offset its benefit by decreasing antiviral and graft-versus-malignancy effect by depletion of donor effector T cells [7].
Even though the use of ATLG in allo-SCT is well established, however, data on optimal ATLG dosing in the setting of MUD-PBSC is scarce, only one study has compared different ATLG doses in
this setting [8]. In the present study, we aim to compare the IR kinetics and transplant outcomes between recipients of 30 mg/Kg vs 60 mg/Kg ATLG as TCD strategies undergoing
MUD-PBSC-allo-SCT with myeloablative conditioning (MAC). MATERIALS AND METHODS This retrospective study conducted at University Medical Center Hamburg-Eppendorf (UKE) with a primary goal to
compare IR between 30 mg/Kg (ATLG-30) vs. 60 mg/kg (ATLG-60) ATLG in recipients of MAC PBSC allo-SCT. The choice of ATLG dose was according to treating physician preference. Secondary
outcomes included incidence of viral reactivations, engraftment, rate of infections and Infection related mortality (IRM), aGVHD, cGVHD, non relapse mortality (NRM), progression free
survival (PFS), and overall survival (OS). All patients signed written informed consents for treatment and the study was approved by the institutional review board at UKE. To have comparable
groups, we selected only patients receiving MAC with PBSC as stem cell source, and MUD (HLA 10/10). MAC regimens were defined according to published working group definition [9]. ATLG
(Grafalon®, Neovii, Switzerland) was given at a dose of 30 mg/kg or 60 mg/kg. A test dose of 200 mg was given at day −4 and the remaining ATLG doses were fractionated between days −3 to −1.
Similar supportive care was used for all patients per institutional guidelines including antimicrobial prophylaxis consisting of fluoroquinolone for bacterial infections,
trimethoprim-sulfamethoxazole or pentamidine for _Pnemocystis jiroveci_, micafungin for fungal infections and acyclovir for viral infections. Patients were screened weekly for CMV and EBV by
blood PCR. Neutrophil engraftment was defined as the first 3 consecutive days with a measure of absolute neutrophil count >0.5 × 109/L. Platelet engraftment was defined as the first
consecutive days with a platelet count >20 × 109/L without transfusion support. Acute GVHD was graded according to standard criteria [10]. Chronic GVHD was graded according to National
Institute of Health (NIH) criteria routinely at every visit after transplantation [11]. Infections were defined as any microbial testing with a positive result and requiring therapy at any
time-point after allo-SCT. As per institution guidelines, blood samples were collected for each patient on days +30, +100, and +180 post-allo-SCT. Routine analyses for absolute
concentrations of CD3+, CD4+, CD8+, NK, and γδ T cells were performed by flow cytometry according to an internal protocol: (1) CD4-APC, CD8-PE, Multitest (CD3 FITC, CD16 + 56 PE, CD45 PerCP,
CD19 APC); (2) CD4-APC, CD45-V450, Multitest (CD45RA FITC, CD45RO PE, CD3 PerCP, CD8 APC); (3) CD45-V450, CD3-PerCPl, anti-TCR-PE, anti-HLA DR-APC in peripheral blood samples. All
antibodies were obtained from Becton Dickinson (BD Biosciences, New Jersey, USA). Up to 5000 events (25,000 per sample) were acquired per tube. Sample acquisition was performed using a BDTM
FACS-Canto flow cytometer with the BDTM FACSDiva software which was also used for data analyses.Immunophenotypes were assessed using four color cytometry using mouse anti-human antibodies
for the following cells: T-lymphocytes (CD3+), activated-T-lymphocytes (CD3+ HLADR+), T-helper (CD3+/CD4+), T-cytotoxic (CD3+/CD8+), B-lymphocytes (CD19+), B-lymphocytes subpopulations
(CD19+CD5+ CD1d+)(CD19+ CD27+), naïve-B-cells (CD19+ CD27-CD10+), NK-cells (CD56+ CD3-), NKT-cells (CD56+ CD3+), naïve-T-helper (CD4+ CD45RA+), memory-T-helper (CD4+ CD45R0+),
naïve-T-cytotoxic (CD8+ CD45RA+), memory-T-cytotoxic (CD8+ CD45R0+ ), γδT-cells (γδTCR+, CD3+), regulatory-T-cells (CD4+ CD25+ CD127low-neg). STATISTICAL METHODS All data was retrospectively
collected and was summarized by standard descriptive statistical methods. χ2 test was used to compare categorical variables, whereas continuous variables were compared using student’s
_t_-test. We defined PFS as survival without relapse or progression of hematological disease; we censored patients without disease or progression at the time of last follow up. We defined OS
and NRM as death from any cause, and without evidence of relapse, respectively. We used the Kaplan-Meier method to calculate the probabilities of DFS and OS; and the cumulative incidence
functions were used to estimate incidence of GVHD, Infections, viral reactivations, RI and NRM. All analysis was performed using SPSS version 26.0 and R version 4.0.5. RESULTS PATIENTS AND
TRANSPLANT CHARACTERISTICS A total of 289 consecutive patients were included in the study. Seventy-three patients (25%) received ATLG-30 and 216 Patients (75%) received ATLG-60with a
tendency to give lower doses in more recent years. The median age at transplant was 57 years (range, 18–71) and 50 years (range, 18–74) in the ATLG-30 and ATLG-60 (_p_ = NS), respectively.
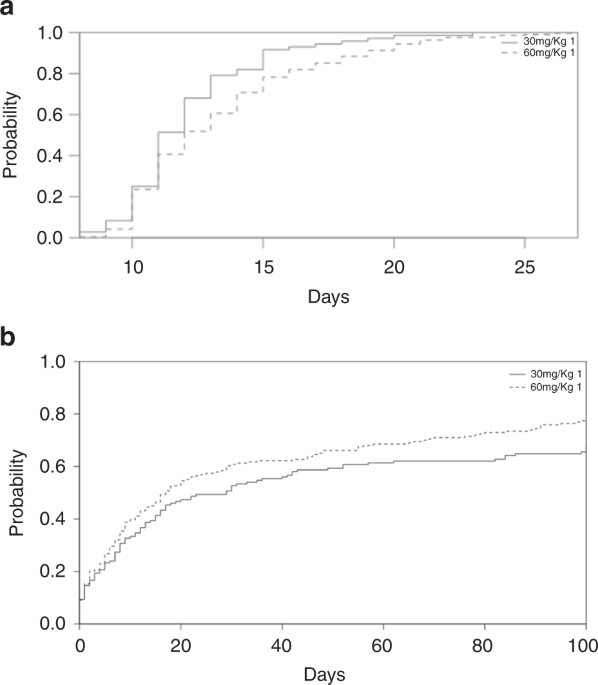
All patients, donor and transplant characteristics are listed in Table 1. TRANSPLANT OUTCOMES All transplant outcomes are summarized in Table 2. ENGRAFTMENT Platelet and neutrophil
engraftment were significantly delayed in ATLG-60 group when compared to the ATLG-30 group with a median of 11 days (range, 8–23) to neutrophil in the ATLG-30 vs 12 days (range, 8–27) in
ATLG-60 group (_P_ = 0.009) (Fig. 1a); and a median of 14 days (range, 9–53) to platelet engraftment in ATLG-30 group vs. 16 days (range, 8–237) in the ATLG-60 group (_p_ = 0.011).
INFECTIONS CMV AND EBV REACTIVATION We observed no significant differences in incidence of CMV reactivation before day 100 (ATLG-30 43%, ATLG-60 45%). The overall incidence of infection
before day 100 was significantly higher in the ATLG-60 (78%) when compared to the ATLG-30 (67%), _p_ = 0.04 (Fig. 1b). The incidence of EBV reactivation before days 100 in the ATLG-30 group
was lower than the ATLG-60 group (21% vs. 41% _p_ = 0.049). IRM at 1-years was 10% in the ATLG-30 vs 11% in the ATLG-60 group (_p_ = 0.7) GRAFT-VERSUS-HOST DISEASE The cumulative incidence
of aGVHD grade II-IV (47% vs 37%, _P_ = 0.09) and III-IV (19% vs 14%, _P_ = 0.2) were comparable in the ATLG-30 vs ATLG-60 groups, respectively. We observed a higher incidence of aGVHD grade
IV in patients receiving ATLG-30 when compared to the ATLG-60 group (8% vs 0.5% _p_ = 0.0002). On univariate analysis, we observed no difference in the cumulative incidence of cGVHD all
grade was (32% vs 37%, _p_ = 0.47), moderate/severe (14% in both groups, _p_ = 0.48) and grade severe (5% vs 4%, _p_ = 0.64) were similar between the 30 mg/Kg ATLG and the 60 mg/Kg ATLG,
respectively. OVERALL SURVIVAL The estimated 3-year OS was 55% for patients in the ATLG-30 group and 51% in the ATLG-60 group (_p_ = 0.16) (Fig. 2a). On univariate analyses patients’ age,
patient and donor CMV serology, donor gender and disease status at transplant significantly affected OS. However, on multivariate analyses only Status at Transplant, Recipient CMV serology
and Donor Gender were significant (Table 3). PROGRESSION FREE SURVIVAL The estimated 3-year PFS was 45% for patients in the ATLG-30 group and 54% in the ATLG-60 group (_p_ = 0.18) (Fig. 2b).
On univariate analyses, older patients, negative recipient CMV serology, female donor, SCT chronology>1 and active disease at time of transplant were associated with decreased DFS. All
the variables except patient age retained their negative impact on DFS in the multivariate analysis (Table 3). NON-RELAPSE MORTALITY The 2-years cumulative incidence of NRM was comparable
between the two groups, with 14% vs 12% in the ATLG-30 and ATLG-60 (_p_ = 0.89), respectively (Fig. 3). On Univariate analysis: older patients, female donor, and negative recipient CMV
serology negatively affected NRM. These variables remained significant on multivariate analyses (Table 4). IMMUNE RECONSTITUTION At day +30, we observed a faster γδTcells reconstitution in
the ATLG-30 group (_p_ = 0.045) (Fig. 4a), however the values at day +100 and +180 were comparable between the two groups. Furthermore, helper naïve T-cells (CD4 + /CD45RA + ) (Fig. 4b) and
NK cells reconstitution was faster at day +180 in the ATLG-30 group (Fig. 4c) and reconstitution of naïve B-cells (CD19+/CD27−/CD10+) was faster at days +30 and +180 in the ATLG-30 group
(_p_ < 0.0001) (Fig. 2d). All our data is summarized in Supplementary Table 1. DISCUSSION Although ATLG is recommended for GVHD prevention in allo-SCT [12], data on optimal ATLG dosing in
the setting of MUD-PBSC is still lacking. Recently a consensus-based recommendation by an international expert panel recommended the use of 30 mg/Kg and 60 mg/Kg of ATLG for sibling and
unrelated MAC allo-SCT, respectively [13]. A retrospective study conducted in 2003 compared two doses of ATLG (<60 mg/Kg vs 60 mg/Kg) in CML Patients undergoing MUD allo-SCT reports
improved OS and DFS in patients receiving >60 mg/Kg ATLG. These differences were attributed to the higher incidence of severe aGVHD in the lower ATLG dose group. A number of 31 patients
received a lower ATLG Dose with 58% receiving 20 mg/Kg ATLG and 36% receiving 40 mg/Kg ATLG [14]. Our findings fall in line with the study, as we reported a higher incidence of severe aGVHD
on univariate and multivariate analysis in the lower ATLG dosing, however this did not impact any of the other outcomes. The discrepancy can be explained by the lower ATLG Doses in this
study and improved supportive care in our population. A study published from our center compared 30 mg/Kg ATLG with 60 mg/Kg ATLG in the MUD-allo-SCT setting between 1997–2005. ATLG was
administered at a dose of 30 mg/kg on day –1 in the 30 mg/Kg group or 20 mg/kg/day on days –3 to –1 in the 60 mg/Kg group. This study reported a higher NRM in the ATLG-60 group, mainly due
to increased incidence of infections in this group with no differences in incidences of aGVHD, cGVHD and Relapse [8]. Our results fall in line with the present study. We observed a higher
incidence of infections in the ATLG-60 group, however, due to improved supportive care this had no impact on NRM. In a multicenter, randomized, open label phase 3 Trial Locatelli et al.
assessed the impact of two doses of ATLG (15 mg/Kg vs 30 mg/Kg over 3 days, from day −4 to −2) in children undergoing MUD-allo-SCT with MAC. They reported lower NRM, higher event free
survival and OS in the lower ATLG dose group. In addition, higher doses of ATLG were associated with increased EBV and Adenovirus reactivation and increased IRM. They observed no significant
differences in incidences of aGVHD and cGVHD between the two groups. Our results fall in line with Locatelli et al. In our we observed a higher incidence of EBV reactivation in the lower
ATLG dose group, however, no differences in any of the long-term outcomes [15]. Butera et al. retrospectively evaluated the impact of two different anti-thymocyte globulin dose
(Thymoglobulin, 5 mg/Kg vs 6.5 mg/Kg) in adults undergoing MUD-allo-SCT at three Italian centers [16]. They report an increased Infection related mortality in the higher ATG dose group, and
no significant differences in any of the other outcomes. In our study, we observed a higher incidence of Infection, however no differences in Infection related mortality between the two
groups. The differences in our outcomes can be explained in terms of the discrepancies in transplant characteristics. Butera et al. included both MAC and RIC, Bone Marrow and PBSC grafts and
they reported a higher proportion of patients with 1HLA mismatch in the higher ATG dose group; while in our population Contrary in the present study, patients were more homogeneous, they
all received MAC, PBSC with 10/10 HLA matched grafts. In addition, in contrast to ATLG Thymoglobulin may contain not only antibodies specific against mature T cell antigens but also antigens
on the thymus-specific cells, thus directly impairing Thymic T cell regeneration and deepening the immunosuppression [17], thus explaining the increased IRM in patients receiving ATG in
contrast to ATLG. Gooptu et al. investigated the effect of ATLG on IR in MUD-PBSCT (_n_ = 44 ATLG, _n_ = 47 placebo) [18]. They reported improved CD3+, CD4+, CD8+, and Treg Lymphocytes in
the Placebo group. They additionally reported delayed CD3+ and CD4+ Lymphocytes reconstitution up to 6 months. Our study falls in line with these findings, the CD3+ and CD4+ Lymphocytes did
not normalize at last follow up. Bacigalupo et al. compared in two randomized trials two different doses of thymoglobuline (15 mg/kg vs 7.5 mg/kg) in patients undergoing MUD-allo-SCT with
MAC conditioning and BM grafts [19]. They reported decreased aGVHD in patients receiving higher doses (37% vs 69%). Two additional studies have compared different ATLG dosing, in
haplo-identical and cord-blood setting [20, 21], both studies have reported increased infectious complications. Taking into consideration the basic differences in transplant types, our
results fall in line with these findings, higher doses of ATLG have reduced incidence of grade IV aGVHD however at the cost of increasing infections in our patient’s population, without any
impact on the long-term outcomes. It has been recently suggested that ATG/ATLG dose should be calculated not only based on Body weight but also according to absolute Lymphocyte count on the
first day of infusion [22, 23]. In two studies this approach has maximized the benefit by decreasing GVHD and reduced the risks of increased infections and relapse. This was also validated
in a post hoc analysis of a RCT where lower ALC counts on first ATLG infusion day was associated with lower PFS and OS [24]. In our study we have not evaluated the impact of ALC on any of
the outcomes. γδTcells and NK-cells protect against viral and bacterial infections [25,26,27,28]. In addition administration of ATLG is associated with a faster γδTcell recovery [29].
Moreover, a recent study on the impact of γδTcells recovery on transplant outcomes in pediatric patients with acute leukemia reported improved DFS and OS in Patients with higher γδTcells
[30], which was also confirmed in the adult populations [29, 31, 32], in addition they reported a decreased incidence of infections in patients with higher γδTcell count. The decreased
γδTcells and longer period of aplasia in the ATLG-60 group can explain the higher incidence of infections in this group. After allo-SCT the numbers of B cells normalize within a year
[33,34,35]. In addition, ATLG induces apoptosis in CD20 + B cells and has shown to induce complement dependent cell lysis in myeloma cells [36, 37]. In our study the B cell have increased
but did not normalize at day 180. In addition, the ATLG-60 group had a significantly lower naïve B-cell Population which supports the hypothesis that CD19 + B cells reduction by ATLG is dose
dependent [38,39,40,41]. Early NK-cells recovery after allo-SCT has been previously reported and it has been postulated that ATLG spares NK cells when compared with other in vivo TCD
strategies [42, 43]. In our study NK-cells recovered at day 30 in both groups and we observed no differences in cell count at all time points after transplant. However, we observed a higher
percentage of NK cells in the ATLG 30 group. This can be clarified by the improved overall lymphopoiesis observed in the ATLG-30 group. ATLG mediates in vivo T cell depletion by complement
mediated cytolysis, Fas-receptor dependent apoptosis and antibody dependent cell mediated cytotoxicity [44]. In addition, Servais et al. analyzed the impact of ATG on IR post MAC PBSC
allo-SCT [45]. It has been established that Tregs suppress GVHD without decreasing GVL [46], and that they accelerate T-cell IR in murine models [47]. Tregs in our study persisted after
allo-SCT and we observed no significant differences in Tregs IR between both groups. This can be explained by previous reports of ATG selectively sparing Tregs [45]. Two studies have
associated higher NKT-cell count with increased GVHD and relapse [48,49,50]. In our study, we observed early recovery of NKT cells without significant differences in IR between the two
groups. In both groups the CD8 + T cell compartment recovered at day +100, while the CD4 + Tcell compartment recovery was not achieved at day +180. This has been previously reported by Fehse
et al. where CD8 + Tcells recovered within the first year after allo-SCT however CD4 + T cells failed to reconstitute within 2 years after allo-SCT [51]. This can be explained by the fact
that: The reconstitution of the Tcell compartment after allo-SCT arises from both homeostatic peripheral expansion (HPE) of donor T-cells transferred with the graft and from novel production
of naïve T-cells in the thymus [52, 53]. In patients receiving MAC most of the T-cells originate from HPE [54, 55]. In addition, HPE occurs more asymmetrically between T-cells, with CD8 +
T-cells having higher proliferating potential by HPE when compared to CD4 + T-cells [45]. Moreover, It has been hypothesized that ATLG targets naïve T cells while sparing memory T cells
[45]. Our study falls in line with previous findings, ATLG selectively compromised the recovery of naïve CD4+, memory CD4+, and naïve CD8+ cells, while it spared memory CD8 + T cells.
However, in our study higher doses of ATLG had more pronounced effects on naïve T CD4 + Tcells, which supports the theory that ATLG exerts a dose dependent T cell effect [38, 56]. In
addition, we observed a higher incidence of EBV reactivation in the ATLG-60 group. This can be attributed to the more pronounced severe depletion of naïve CD4 + Tcells and NK cells in this
group. More patients in the ATLG-30 group were not in CR at time of transplant, however we observed no differences in relapse incidence between the two groups which suggests a higher Graft
versus Malignancy effect in the ATLG-30 group. However, it should be noted that more Patients in the ATLG-30 group had active disease at time of transplant, therefore calcineurin inhibitor
may have differed between the two groups and may have influenced immune reconstitution. Acknowledging the retrospective nature of our study, the choice of ATLG dose has significant impact on
IR post MUD-allo-SCT, higher doses reduce aGVHD however they delayed engraftment, impair B-cell, γδTcells, NK and CD4 + T cell reconstitution and increase the risk for infection and EBV
reactivation. However, this did not affect any of the long-term outcomes. DATA AVAILABILITY The datasets generated during and/or analysed during the current study are available from the
corresponding author on reasonable request. REFERENCES * Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006;354:1813–26. https://doi.org/10.1056/NEJMra052638. Article
CAS PubMed Google Scholar * Horowitz MM, Gale RP, Sondel PM, Goldman JM, Kersey J, Kolb HJ, et al. Graft-versus-leukemia reactions after bone marrow transplantation. Blood.
1990;75:555–62. Article CAS Google Scholar * Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, et al. Clinical manifestations of graft-versus-host disease in human
recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974;18:295–304. https://doi.org/10.1097/00007890-197410000-00001. Article CAS PubMed Google Scholar * Bonifazi F,
Solano C, Wolschke C, Sessa M, Patriarca F, Zallio F, et al. Acute GVHD prophylaxis plus ATLG after myeloablative allogeneic haemopoietic peripheral blood stem-cell transplantation from
HLA-identical siblings in patients with acute myeloid leukaemia in remission: final results of quality of life and long-term outcome analysis of a phase 3 randomised study. Lancet Haematol.
2019;6:e89–e99. https://doi.org/10.1016/S2352-3026(18)30214-X. Article PubMed Google Scholar * Finke J, Bethge WA, Schmoor C, Ottinger HD, Stelljes M, Zander AR, et al. Standard
graft-versus-host disease prophylaxis with or without anti-T-cell globulin in haematopoietic cell transplantation from matched unrelated donors: a randomised, open-label, multicentre phase 3
trial. Lancet Oncol. 2009;10:855–64. https://doi.org/10.1016/S1470-2045(09)70225-6. Article CAS PubMed Google Scholar * Kroger N, Solano C, Wolschke C, Bandini G, Patriarca F, Pini M,
et al. Antilymphocyte globulin for prevention of chronic graft-versus-host disease. N Engl J Med. 2016;374:43–53. https://doi.org/10.1056/NEJMoa1506002. Article CAS PubMed Google Scholar
* Locatelli F, Merli P, Bertaina A. Rabbit anti-human T-lymphocyte globulin and hematopoietic transplantation. Oncotarget. 2017;8:96460–1. https://doi.org/10.18632/oncotarget.20878.
Article PubMed PubMed Central Google Scholar * Ayuk F, Diyachenko G, Zabelina T, Wolschke C, Fehse B, Bacher U, et al. Comparison of two doses of antithymocyte globulin in patients
undergoing matched unrelated donor allogeneic stem cell transplantation. Biol Blood Marrow Transpl. 2008;14:913–9. https://doi.org/10.1016/j.bbmt.2008.05.023. Article CAS Google Scholar *
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transpl. 2009;15:1628–33.
https://doi.org/10.1016/j.bbmt.2009.07.004. Article Google Scholar * Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. Consensus conference on acute GVHD grading.
Bone Marrow Transpl 1995. 1994;15:825–8. Google Scholar * Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et al. National Institutes of Health consensus development
project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transpl. 2005;11:945–56.
https://doi.org/10.1016/j.bbmt.2005.09.004. Article Google Scholar * Penack O, Marchetti M, Ruutu T, Aljurf M, Bacigalupo A, Bonifazi F, et al. Prophylaxis and management of graft versus
host disease after stem-cell transplantation for haematological malignancies: updated consensus recommendations of the European Society for Blood and Marrow Transplantation. Lancet Haematol.
2020;7:e157–e167. https://doi.org/10.1016/S2352-3026(19)30256-X. Article PubMed Google Scholar * Bonifazi F, Rubio MT, Bacigalupo A, Boelens JJ, Finke J, Greinix H, et al. Rabbit
ATG/ATLG in preventing graft-versus-host disease after allogeneic stem cell transplantation: consensus-based recommendations by an international expert panel. Bone Marrow Transpl.
2020;55:1093–102. https://doi.org/10.1038/s41409-020-0792-x. Article CAS Google Scholar * Schleuning M, Gunther W, Tischer J, Ledderose G, Kolb HJ. Dose-dependent effects of in vivo
antithymocyte globulin during conditioning for allogeneic bone marrow transplantation from unrelated donors in patients with chronic phase CML. Bone Marrow Transpl. 2003;32:243–50.
https://doi.org/10.1038/sj.bmt.1704135. Article CAS Google Scholar * Locatelli F, Bernardo ME, Bertaina A, Rognoni C, Comoli P, Rovelli A, et al. Efficacy of two different doses of rabbit
anti-T-lymphocyte globulin to prevent graft-versus-host disease in children with haematological malignancies transplanted from an unrelated donor: a multicentre, randomised, open-label,
phase 3 trial. Lancet Oncol. 2017;18:1126–36. https://doi.org/10.1016/S1470-2045(17)30417-5. Article CAS PubMed Google Scholar * Butera S, Cerrano M, Brunello L, Dellacasa CM, Faraci DG,
Vassallo S, et al. Impact of anti-thymocyte globulin dose for graft-versus-host disease prophylaxis in allogeneic hematopoietic cell transplantation from matched unrelated donors: a
multicenter experience. Ann Hematol. 2021;100:1837–47. https://doi.org/10.1007/s00277-021-04521-z Article CAS PubMed PubMed Central Google Scholar * Mensen A, Na IK, Hafer R, Meerbach
A, Schlecht M, Pietschmann ML, et al. Comparison of different rabbit ATG preparation effects on early lymphocyte subset recovery after allogeneic HSCT and its association with EBV-mediated
PTLD. J Cancer Res Clin Oncol. 2014;140:1971–80. https://doi.org/10.1007/s00432-014-1742-z. Article CAS PubMed Google Scholar * Gooptu M, Kim HT, Chen YB, Rybka W, Artz A, Boyer M, et
al. Effect of antihuman T lymphocyte globulin on immune recovery after myeloablative allogeneic stem cell transplantation with matched unrelated donors: analysis of immune reconstitution in
a double-blind randomized controlled trial. Biol Blood Marrow Transpl. 2018;24:2216–23. https://doi.org/10.1016/j.bbmt.2018.07.002. Article CAS Google Scholar * Bacigalupo A, Lamparelli
T, Bruzzi P, Guidi S, Alessandrino PE, di Bartolomeo P, et al. Antithymocyte globulin for graft-versus-host disease prophylaxis in transplants from unrelated donors: 2 randomized studies
from Gruppo Italiano Trapianti Midollo Osseo (GITMO). Blood. 2001;98:2942–7. https://doi.org/10.1182/blood.v98.10.2942. Article CAS PubMed Google Scholar * Wang Y, Fu HX, Liu DH, Xu LP,
Zhang XH, Chang YJ, et al. Influence of two different doses of antithymocyte globulin in patients with standard-risk disease following haploidentical transplantation: a randomized trial.
Bone Marrow Transpl. 2014;49:426–33. https://doi.org/10.1038/bmt.2013.191. Article CAS Google Scholar * de Koning C, Admiraal R, Nierkens S, Boelens JJ. Immune reconstitution and outcomes
after conditioning with anti-thymocyte-globulin in unrelated cord blood transplantation; the good, the bad, and the ugly. Stem Cell Investig. 2017;4:38
https://doi.org/10.21037/sci.2017.05.02. Article CAS PubMed PubMed Central Google Scholar * Admiraal R, van Kesteren C, Zijde J-vd, Lankester CM, Bierings AC, Egberts MB, et al.
Association between anti-thymocyte globulin exposure and CD4+ immune reconstitution in paediatric haemopoietic cell transplantation: a multicentre, retrospective pharmacodynamic cohort
analysis. Lancet Haematol. 2015;2:e194–203. https://doi.org/10.1016/S2352-3026(15)00045-9. Article PubMed Google Scholar * Podgorny PJ, Ugarte-Torres A, Liu Y, Williamson TS, Russell JA,
Storek J. High rabbit-antihuman thymocyte globulin levels are associated with low likelihood of graft-vs-host disease and high likelihood of posttransplant lymphoproliferative disorder. Biol
Blood Marrow Transpl. 2010;16:915–26. https://doi.org/10.1016/j.bbmt.2010.02.027. Article CAS Google Scholar * Soiffer RJ, Kim HT, McGuirk J, Horwitz ME, Johnston L, Patnaik MM, et al.
Prospective, randomized, double-blind, phase III clinical trial of anti-T-lymphocyte globulin to assess impact on chronic graft-versus-host disease-free survival in patients undergoing
HLA-matched unrelated myeloablative hematopoietic cell transplantation. J Clin Oncol. 2017;35:4003–11. https://doi.org/10.1200/JCO.2017.75.8177. Article CAS PubMed PubMed Central Google
Scholar * Horowitz A, Stegmann KA, Riley EM. Activation of natural killer cells during microbial infections. Front Immunol. 2011;2:88. https://doi.org/10.3389/fimmu.2011.00088. Article
PubMed Google Scholar * Zheng J, Liu Y, Lau Y-L, Tu W. γδ-T cells: an unpolished sword in human anti-infection immunity. Cell Mol Immunol. 2013;10:50. Article CAS Google Scholar *
Scheper W, van Dorp S, Kersting S, Pietersma F, Lindemans C, Hol S, et al. T cells elicited by CMV reactivation after allo-SCT cross-recognize CMV and leukemia. Leukemia. 2013;27:1328.
Article CAS Google Scholar * Knight A, Madrigal AJ, Grace S, Sivakumaran J, Kottaridis P, Mackinnon S, et al. The role of Vδ2-negative γδ T cells during cytomegalovirus reactivation in
recipients of allogeneic stem cell transplantation. Blood. 2010;116:2164–72. Article CAS Google Scholar * Klyuchnikov E, Badbaran A, Massoud R, Fritsche-Friedland U, Janson D, Ayuk F, et
al. Enhanced Immune Reconstitution of γδ T Cells after Allogeneic Stem Cell Transplantation Overcomes the Negative Impact of Pretransplantation Minimal Residual Disease-Positive Status in
Patients with Acute Myelogenous Leukemia. Transplant Cell Ther. 2021;27:841–50. * Perko R, Kang G, Sunkara A, Leung W, Thomas PG, Dallas MH. Gamma delta T cell reconstitution is associated
with fewer infections and improved event-free survival after hematopoietic stem cell transplantation for pediatric leukemia. Biol Blood Marrow Transplant. 2015;21:130–6. Article Google
Scholar * Lamb L Jr., Gee AP, Hazlett LJ, Musk P, Parrish R, O’Hanlon T, et al. Influence of T cell depletion method on circulating γδ T cell reconstitution and potential role in the
graft-versus-leukemia effect. Cytotherapy. 1999;1:7–19. Article Google Scholar * Godder K, Henslee-Downey P, Mehta J, Park B, Chiang K, Abhyankar S, et al. Long term disease-free survival
in acute leukemia patients recovering with increased γδ T cells after partially mismatched related donor bone marrow transplantation. Bone Marrow Transplant. 2007;39:751. Article CAS
Google Scholar * Storek J, Ferrara S, Ku N, Giorgi JV, Champlin RE, Saxon A. B cell reconstitution after human bone marrow transplantation: recapitulation of ontogeny? Bone Marrow Transpl.
1993;12:387–98. CAS Google Scholar * Storek J, Dawson MA, Storer B, Stevens-Ayers T, Maloney DG, Marr KA, et al. Immune reconstitution after allogeneic marrow transplantation compared with
blood stem cell transplantation. Blood. 2001;97:3380–9. https://doi.org/10.1182/blood.v97.11.3380. Article CAS PubMed Google Scholar * Small TN, Keever CA, Weiner-Fedus S, Heller G,
O’Reilly RJ, Flomenberg N. B-cell differentiation following autologous, conventional, or T-cell depleted bone marrow transplantation: a recapitulation of normal B-cell ontogeny. Blood.
1990;76:1647–56. Article CAS Google Scholar * Grullich C, Ziegler C, Finke J. Rabbit anti T-lymphocyte globulin induces apoptosis in peripheral blood mononuclear cell compartments and
leukemia cells, while hematopoetic stem cells are apoptosis resistant. Biol Blood Marrow Transpl. 2009;15:173–82. https://doi.org/10.1016/j.bbmt.2008.11.014. Article Google Scholar * Ayuk
FA, Fang L, Fehse B, Zander AR, Kroger N. Antithymocyte globulin induces complement-dependent cell lysis and caspase-dependent apoptosis in myeloma cells. Exp Hematol. 2005;33:1531–6.
https://doi.org/10.1016/j.exphem.2005.08.004. Article CAS PubMed Google Scholar * Preville X, Flacher M, LeMauff B, Beauchard S, Davelu P, Tiollier J, et al. Mechanisms involved in
antithymocyte globulin immunosuppressive activity in a nonhuman primate model. Transplantation. 2001;71:460–8. https://doi.org/10.1097/00007890-200102150-00021. Article CAS PubMed Google
Scholar * Zand MS. B-cell activity of polyclonal antithymocyte globulins. Transplantation. 2006;82:1387–95. https://doi.org/10.1097/01.tp.0000244063.05338.27. Article CAS PubMed Google
Scholar * Muller TF, Grebe SO, Neumann MC, Heymanns J, Radsak K, Sprenger H, et al. Persistent long-term changes in lymphocyte subsets induced by polyclonal antibodies. Transplantation.
1997;64:1432–7. https://doi.org/10.1097/00007890-199711270-00010. Article CAS PubMed Google Scholar * Neumann MC, Muller TF, Sprenger H, Gemsa D, Lange H. The influence of the
immunosuppressants OKT3 and ATG on immunological parameters. Clin Nephrol. 1996;45:345–8. PubMed Google Scholar * Massoud R, Gagelmann N, Fritzsche-Friedland U, Zeck G, Heidenreich S,
Wolschke C, et al. Comparison of immune reconstitution between anti-T-lymphocyte globulin and post-transplant cyclophosphamide as acute graft-versus-host disease prophylaxis in allogeneic
myeloablative peripheral blood stem cell transplantation. Haematologica. 2022;107:857–67. Article PubMed PubMed Central Google Scholar * Retiere C, Willem C, Guillaume T, Vie H,
Gautreau-Rolland L, Scotet E, et al. Impact on early outcomes and immune reconstitution of high-dose post-transplant cyclophosphamide vs anti-thymocyte globulin after reduced intensity
conditioning peripheral blood stem cell allogeneic transplantation. Oncotarget. 2018;9:11451–64. https://doi.org/10.18632/oncotarget.24328. Article PubMed PubMed Central Google Scholar *
Mohty M. Mechanisms of action of antithymocyte globulin: T-cell depletion and beyond. Leukemia. 2007;21:1387–94. https://doi.org/10.1038/sj.leu.2404683. Article CAS PubMed Google Scholar
* Servais S, Menten-Dedoyart C, Beguin Y, Seidel L, Gothot A, Daulne C, et al. Impact of pre-transplant anti-T cell globulin (ATG) on immune recovery after myeloablative allogeneic
peripheral blood stem cell transplantation. PLoS One. 2015;10:e0130026 https://doi.org/10.1371/journal.pone.0130026. Article CAS PubMed PubMed Central Google Scholar * Edinger M,
Hoffmann P, Ermann J, Drago K, Fathman CG, Strober S, et al. CD4+ CD25+ regulatory T cells preserve graft-versus-tumor activity while inhibiting graft-versus-host disease after bone marrow
transplantation. Nat Med. 2003;9:1144. Article CAS Google Scholar * Nguyen VH, Shashidhar S, Chang DS, Ho L, Kambham N, Bachmann M, et al. The impact of regulatory T cells on T-cell
immunity following hematopoietic cell transplantation. Blood. 2008;111:945–53. https://doi.org/10.1182/blood-2007-07-103895. Article CAS PubMed PubMed Central Google Scholar * Salio M,
Silk JD, Yvonne JE, Cerundolo V. Biology of CD1-and MR1-restricted T cells. Annu Rev Immunol. 2014;32:323–66. Article CAS Google Scholar * Bendelac A, Savage PB, Teyton L. The biology of
NKT cells. Annu Rev Immunol. 2007;25:297–336. Article CAS Google Scholar * Kim TW, Park S-S, Lim J-Y, Min GJ, Park S, Jeon Y-W, et al. Predictive role of circulating immune cell subtypes
early after allogeneic hematopoietic stem cell transplantation in patients with acute leukemia. Int J Stem Cells. 2019;12:73. Article Google Scholar * Fehse N, Fehse B, Kroger N, Zabelina
T, Freiberger P, Kruger W, et al. Influence of anti-thymocyte globulin as part of the conditioning regimen on immune reconstitution following matched related bone marrow transplantation. J
Hematother Stem Cell Res. 2003;12:237–42. https://doi.org/10.1089/152581603321628377. Article CAS PubMed Google Scholar * Bosch M, Dhadda M, Hoegh-Petersen M, Liu Y, Hagel LM, Podgorny
P, et al. Immune reconstitution after anti-thymocyte globulin-conditioned hematopoietic cell transplantation. Cytotherapy. 2012;14:1258–75. https://doi.org/10.3109/14653249.2012.715243.
Article CAS PubMed PubMed Central Google Scholar * Toubert A, Glauzy S, Douay C, Clave E. Thymus and immune reconstitution after allogeneic hematopoietic stem cell transplantation in
humans: never say never again. Tissue Antigens. 2012;79:83–89. Article CAS Google Scholar * Chawla S, Dharmani-Khan P, Liu Y, Prokopishyn N, Amlish Munir M, Griffiths C, et al. High serum
level of antithymocyte globulin immediately before graft infusion is associated with a low likelihood of chronic, but not acute, graft-versus-host disease. Biol Blood Marrow Transpl.
2014;20:1156–62. https://doi.org/10.1016/j.bbmt.2014.04.007. Article CAS Google Scholar * Remberger M, Sundberg B. Rabbit-immunoglobulin G levels in patients receiving thymoglobulin as
part of conditioning before unrelated donor stem cell transplantation. Haematologica. 2005;90:931–8. CAS PubMed Google Scholar * Meijer E, Bloem AC, Dekker AW, Verdonck LF. Effect of
antithymocyte globulin on quantitative immune recovery and graft-versus-host disease after partially T-cell-depleted bone marrow transplantation: a comparison between recipients of matched
related and matched unrelated donor grafts. Transplantation. 2003;75:1910–3. https://doi.org/10.1097/01.TP.0000065737.60591.9D. Article CAS PubMed Google Scholar Download references
FUNDING Open Access funding enabled and organized by Projekt DEAL. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Stem Cell Transplantation, University Medical Center
Hamburg-Eppendorf, Hamburg, Germany Radwan Massoud, Evgeny Klyuchnikov, Nico Gagelmann, Tatiana Zabelina, Christine Wolschke, Francis Ayuk, Ulrike Fritzsche-Friedland, Axel Zander &
Nicolaus Kröger Authors * Radwan Massoud View author publications You can also search for this author inPubMed Google Scholar * Evgeny Klyuchnikov View author publications You can also
search for this author inPubMed Google Scholar * Nico Gagelmann View author publications You can also search for this author inPubMed Google Scholar * Tatiana Zabelina View author
publications You can also search for this author inPubMed Google Scholar * Christine Wolschke View author publications You can also search for this author inPubMed Google Scholar * Francis
Ayuk View author publications You can also search for this author inPubMed Google Scholar * Ulrike Fritzsche-Friedland View author publications You can also search for this author inPubMed
Google Scholar * Axel Zander View author publications You can also search for this author inPubMed Google Scholar * Nicolaus Kröger View author publications You can also search for this
author inPubMed Google Scholar CONTRIBUTIONS RM and NK designed the study, analyzed data, interpreted results, and wrote the manuscript. EK, NG, TZ, CW, FA, UF and AZ collected and analyzed
data. All authors approved the final version of the manuscript. CORRESPONDING AUTHOR Correspondence to Nicolaus Kröger. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no
competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
SUPPLEMENTARY INFORMATION SUPPLEMENTARY TABLE RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use,
sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative
Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated
otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds
the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/. Reprints and
permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Massoud, R., Klyuchnikov, E., Gagelmann, N. _et al._ Impact of Anti-T-lymphocyte globulin dosing on GVHD and Immune reconstitution in matched
unrelated myeloablative peripheral blood stem cell transplantation. _Bone Marrow Transplant_ 57, 1548–1555 (2022). https://doi.org/10.1038/s41409-022-01666-x Download citation * Received:
27 September 2021 * Revised: 23 March 2022 * Accepted: 29 March 2022 * Published: 13 July 2022 * Issue Date: October 2022 * DOI: https://doi.org/10.1038/s41409-022-01666-x SHARE THIS ARTICLE
Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard
Provided by the Springer Nature SharedIt content-sharing initiative