The significance of peri-transplantation minimal residual disease assessed by multiparameter flow cytometry on outcomes for adult aml patients receiving haploidentical allografts
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
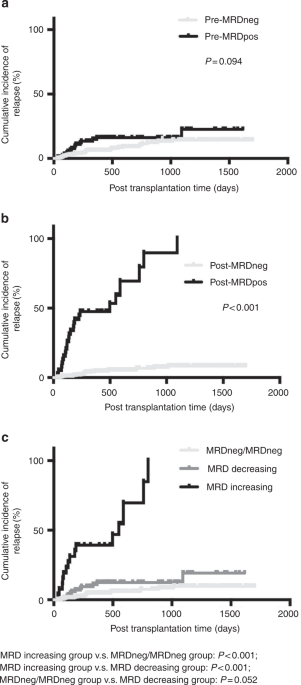
ABSTRACT A retrospective study (_n_ = 460) was performed to assess the relationship between minimal residual disease (MRD) and transplant outcomes in a haplo-stem cell transplantation (SCT)
setting. Patients from the pre-MRDneg group and the pre-MRDpos group had comparable outcomes. Compared to post-MRDneg patients, post-MRDpos patients had a higher incidence of relapse (100.0%
vs. 8.3%, _p_ < 0.001), lower incidences of overall survival (OS) (16.9% vs. 78.2%, _p_ < 0.001) and leukemia-free survival (LFS) (0% vs. 76.5%, _p_ < 0.001), and comparable
probability of NRM (13.4% vs. 16.9%, _p_ = 0.560). In a second set of analyses, all adult AML patients undergoing haplo-SCT were classified into the MRDneg/MRDneg group, the MRD decreasing
group, and the MRD increasing group according to MRD dynamics by flow cytometry peri-SCT. Compared to the other two groups, patients from the MRD increasing group had higher cumulative
incidences of relapse (MRD increasing, 100.0%; MRDneg/MRDneg, 9.6%; MRD decreasing, 19.2%; _p_ < 0.001) and worse probabilities of OS (MRD increasing, 28.5%; MRDneg/MRDneg, 76.3%; MRD
decreasing, 76.0%; p < 0.001) and LFS (MRD increasing, 0.0%; MRDneg/MRDneg, 73.9%; MRD decreasing, 74.0%; _p_ < 0.001). The results indicated that haploidentical allografts might have
a beneficial anti-leukemia effect in eradicating pretransplantation MRD, and MRD assessment peri-SCT is useful for risk stratification from a practical perspective. Access through your
institution Buy or subscribe This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through your institution Subscribe to this journal Receive 12 print
issues and online access $259.00 per year only $21.58 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now Prices may be subject to
local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer support SIMILAR CONTENT
BEING VIEWED BY OTHERS MEASURABLE RESIDUAL DISEASE STATUS AND OUTCOME OF TRANSPLANT IN ACUTE MYELOID LEUKEMIA IN SECOND COMPLETE REMISSION: A STUDY BY THE ACUTE LEUKEMIA WORKING PARTY OF THE
EBMT Article Open access 12 May 2021 PRETRANSPLANTATION RISK FACTORS FOR POSITIVE MRD AFTER ALLOGENEIC STEM CELL TRANSPLANTATION IN AML PATIENTS: A PROSPECTIVE STUDY Article 16 November
2024 RELATIONSHIP BETWEEN MORPHOLOGIC REMISSION WITH OR WITHOUT HEMATOLOGIC RECOVERY AND OUTCOME AFTER ALLOGENEIC HEMATOPOIETIC CELL TRANSPLANTATION IN ADULT ACUTE MYELOID LEUKEMIA Article
29 August 2024 REFERENCES * Campana D, Leung W. Clinical significance of minimal residual disease in patients with acute leukaemia undergoing haematopoietic stem cell transplantation. Br J
Haematol. 2013;162:147–61. https://doi.org/10.1111/bjh.12358 Article PubMed Google Scholar * Buckley SA, Appelbaum FR, Walter RB. Prognostic and therapeutic implications of minimal
residual disease at the time of transplantation in acute leukemia. Bone Marrow Transplant. 2013;48:630–41. https://doi.org/10.1038/bmt.2012.139 Article CAS PubMed Google Scholar *
Hourigan CS, Karp JE. Minimal residual disease in acute myeloid leukaemia. Nat Rev Clin Oncol. 2013;10:460–71. https://doi.org/10.1038/nrclinonc.2013.100 Article CAS PubMed PubMed Central
Google Scholar * Freeman SD, Virgo P, Couzens S, Grimwade D, Russell N, Hills RK, et al. Prognostic relevance of treatment response measured by flow cytometric residual disease detection
in older patients with acute myeloid leukemia. J Clin Oncol. 2013;31:4123–31. https://doi.org/10.1200/JCO.2013.49.1753 Article PubMed Google Scholar * Walter RB, Gyurkocza B, Storer BE,
Godwin CD, Pagel JM, Buckley SA, et al. Comparison of minimal residual disease as outcome predictor for AML patients in first complete remission undergoing myeloablative or nonmyeloablative
allogeneic hematopoietic cell transplantation. Leukemia. 2015;29:137–44. https://doi.org/10.1038/leu.2014.173 Article CAS PubMed Google Scholar * Zhou Y, Othus M, Araki D, Wood BL,
Radich JP, Halpern AB, et al. Pre- and post-transplant quantification of measurable (“minimal”) residual disease via multiparameter flow cytometry in adult acute myeloid leukemia. Leukemia.
2016;30:1456–64. https://doi.org/10.1038/leu.2016.46 Article CAS PubMed PubMed Central Google Scholar * Walter RB, Buckley SA, Pagel JM, Wood BL, Storer BE, Sandmaier BM, et al.
Significance of minimal residual disease before myeloablative allogeneic hematopoietic cell transplantation for AML in first and second complete remission. Blood. 2013;122:1813–21.
https://doi.org/10.1182/blood-2013-06-506725 Article CAS PubMed PubMed Central Google Scholar * Oran B, Jorgensen JL, Marin D, Wang S, Ahmed S, Alousi AM, et al. Pre-transplantation
minimal residual disease with cytogenetic and molecular diagnostic features improves risk stratification in acute myeloid leukemia. Haematologica. 2017;102:110–7. Article CAS PubMed
PubMed Central Google Scholar * Chang Y-J, Wang Y, Liu Y-R, Xu L-P, Zhang X-H, Chen H, et al. Haploidentical allograft is superior to matched sibling donor allograft in eradicating
pre-transplantation minimal residual disease of AML patients as determined by multiparameter flow cytometry: a retrospective and prospective analysis. J Hematol Oncol. 2017;10:134. Article
PubMed PubMed Central Google Scholar * Chang YJ, Zhao XS, Wang Y, Liu YR, Xu LP, Zhang XH et al. Effects of pre- and post-transplantation minimal residual disease on outcomes in pediatric
patients with acute myeloid leukemia receiving human leukocyte antigen-matched or mismatched related donor allografts. Am J Hematol. 2017. https://doi.org/10.1002/ajh.24910 Article CAS
PubMed Google Scholar * Wang Y, Liu QF, Xu LP, Liu KY, Zhang XH, Ma X, et al. Haploidentical vs identical-sibling transplant for AML in remission: a multicenter, prospective study. Blood.
2015;125:3956–62. https://doi.org/10.1182/blood-2015-02-627786 Article CAS PubMed Google Scholar * Del Vecchio L, Brando B, Lanza F, Ortolani C, Pizzolo G, Semenzato G, et al.
Recommended reporting format for flow cytometry diagnosis of acute leukemia. Haematologica. 2004;89:594–8. PubMed Google Scholar * Feller N, van der Velden VH, Brooimans RA, Boeckx N,
Preijers F, Kelder A, et al. Defining consensus leukemia-associated immunophenotypes for detection of minimal residual disease in acute myeloid leukemia in a multicenter setting. Blood
Cancer J. 2013;3:e129 https://doi.org/10.1038/bcj.2013.27 Article CAS PubMed PubMed Central Google Scholar * Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows, et al.
1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant. 1995;15:825–8. CAS PubMed Google Scholar * Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et
al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol
Blood Marrow Transplant. 2005;11:945–56. https://doi.org/10.1016/j.bbmt.2005.09.004 Article PubMed Google Scholar * Wang Y, Liu DH, Xu LP, Liu KY, Chen H, Chen YH, et al. Superior
graft-versus-leukemia effect associated with transplantation of haploidentical compared with HLA-identical sibling donor grafts for high-risk acute leukemia: an historic comparison. Biol
Blood Marrow Transplant. 2011;17:821–30. https://doi.org/10.1016/j.bbmt.2010.08.023 Article PubMed Google Scholar * Luo Y, Xiao H, Lai X, Shi J, Tan Y, He J, et al. T-cell-replete
haploidentical HSCT with low-dose anti-T-lymphocyte globulin compared with matched sibling HSCT and unrelated HSCT. Blood. 2014;124:2735–43. https://doi.org/10.1182/blood-2014-04-571570
Article CAS PubMed PubMed Central Google Scholar * Casucci M, Perna SK, Falcone L, Camisa B, Magnani Z, Bernardi M, et al. Graft-versus-leukemia effect of HLA-haploidentical
central-memory T-cells expanded with leukemic APCs and modified with a suicide gene. Mol Ther. 2013;21:466–75. https://doi.org/10.1038/mt.2012.227 Article CAS PubMed Google Scholar * Yan
C, Liu D, Liu K, Xu L, Liu Y, Chen H, et al. Risk stratification-directed donor lymphocyte infusion could reduce relapse of standard-risk acute leukemia patients after allogeneic
hematopoietic stem cell transplantation. Blood. 2012;119:3256–62. Article CAS PubMed Google Scholar * Yan CH, Wang Y, Wang JZ, Chen YH, Chen Y, Wang FR, et al. Minimal residual disease-
and graft-vs.-host disease-guided multiple consolidation chemotherapy and donor lymphocyte infusion prevent second acute leukemia relapse after allotransplant. J Hematol Oncol. 2016;9:87
https://doi.org/10.1186/s13045-016-0319-5 Article PubMed PubMed Central Google Scholar * Dao MA AJ, Nolta JA. Reversibility of CD34 expression on human hematopoietic stem cells that
retain the capacity for secondary reconstitution. Blood. 2003;101:112–8. Article PubMed Google Scholar * Hess DA, Karanu FN, Levac K, Gallacher L, Bhatia M. Coculture and transplant of
purified CD34(+)Lin(−) and CD34(−)Lin(−) cells reveals functional interaction between repopulating hematopoietic stem cells. Leukemia. 2003;17:1613–25. https://doi.org/10.1038/sj.leu.2403028
Article CAS PubMed Google Scholar * Sato TLJ, Ogawa M. Reversible expression of CD34 by murine hematopoietic stem cells. Blood. 1999;94:2548–54. CAS PubMed Google Scholar * Tajima F,
Deguchi T, Laver JH, Zeng H, Ogawa M. Reciprocal expression of CD38 and CD34 by adult murine hematopoietic stem cells. Blood. 2001;97:2618–24. Article CAS PubMed Google Scholar * Guo Z,
Gao HY, Zhang TY, Liu XD, Yang K, Lou JX, et al. Analysis of allogeneic hematopoietic stem cell transplantation with high-dose cyclophosphamide-induced immune tolerance for severe aplastic
anemia. Int J Hematol. 2016;104:720–8. Article CAS PubMed Google Scholar * How J, Slade M, Vu K, Dipersio JF, Westervelt P, Uy GL, et al. T cell-replete haploidentical transplantation
with post-transplantation cyclophosphamide for hodgkin lymphoma relapsed after autologous transplantation: reduced incidence of relapse and of chronic graft-versus-host disease compared with
HLA-identical related donors. Biol Blood Marrow Transplant. 2017;24:627–32. Google Scholar Download references ACKNOWLEDGMENTS We thank all the faculty members that participated in these
studies. We would also like to thank American Journal Experts (www.aje.com) for the assistance in editing this manuscript. AUTHOR CONTRIBUTIONS Contribution: Y.-J.C. designed the study; J.
L, R. M, and Y.-J.C. collected data; J. L and Y.-J.C. analyzed the data and drafted the manuscript; all authors contributed to data interpretation, manuscript preparation, and approval of
the final version. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Peking University People’s Hospital & Peking University Institute of Hematology, Beijing Key Laboratory of Hematopoietic
Stem Cell Transplantation, No. 11 South Street of Xizhimen, Xicheng District, Beijing, 100044, P.R. China Jing Liu, Rui Ma, Yan-Rong Liu, Lan-Ping Xu, Xiao-Hui Zhang, Huan Chen, Yu-Hong
Chen, Feng-Rong Wang, Wei Han, Yu-Qian Sun, Chen-Hua Yan, Fei-Fei Tang, Xiao-Dong Mo, Kai-Yan Liu, Qiao-Zhen Fan, Xiao-Jun Huang & Ying-Jun Chang * Peking-Tsinghua Center for Life
Sciences, Beijing, 100871, China Xiao-Jun Huang * Collaborative Innovation Center of Hematology, Peking University, Beijing, China Xiao-Jun Huang & Ying-Jun Chang Authors * Jing Liu View
author publications You can also search for this author inPubMed Google Scholar * Rui Ma View author publications You can also search for this author inPubMed Google Scholar * Yan-Rong Liu
View author publications You can also search for this author inPubMed Google Scholar * Lan-Ping Xu View author publications You can also search for this author inPubMed Google Scholar *
Xiao-Hui Zhang View author publications You can also search for this author inPubMed Google Scholar * Huan Chen View author publications You can also search for this author inPubMed Google
Scholar * Yu-Hong Chen View author publications You can also search for this author inPubMed Google Scholar * Feng-Rong Wang View author publications You can also search for this author
inPubMed Google Scholar * Wei Han View author publications You can also search for this author inPubMed Google Scholar * Yu-Qian Sun View author publications You can also search for this
author inPubMed Google Scholar * Chen-Hua Yan View author publications You can also search for this author inPubMed Google Scholar * Fei-Fei Tang View author publications You can also search
for this author inPubMed Google Scholar * Xiao-Dong Mo View author publications You can also search for this author inPubMed Google Scholar * Kai-Yan Liu View author publications You can
also search for this author inPubMed Google Scholar * Qiao-Zhen Fan View author publications You can also search for this author inPubMed Google Scholar * Xiao-Jun Huang View author
publications You can also search for this author inPubMed Google Scholar * Ying-Jun Chang View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING
AUTHOR Correspondence to Ying-Jun Chang. ETHICS DECLARATIONS CONFLICT OF INTEREST The authors declare that they have no conflict of interest. ELECTRONIC SUPPLEMENTARY MATERIAL SUPPLEMENT
TABLE 1 RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Liu, J., Ma, R., Liu, YR. _et al._ The significance of peri-transplantation minimal residual
disease assessed by multiparameter flow cytometry on outcomes for adult AML patients receiving haploidentical allografts. _Bone Marrow Transplant_ 54, 567–577 (2019).
https://doi.org/10.1038/s41409-018-0300-8 Download citation * Received: 07 February 2018 * Revised: 27 June 2018 * Accepted: 12 July 2018 * Published: 20 August 2018 * Issue Date: April 2019
* DOI: https://doi.org/10.1038/s41409-018-0300-8 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is
not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative