Natural t-cell responses against minor histocompatibility antigen (mhag) hy following hla-matched hematopoietic cell transplantation: what are the requirements for a ‘good’ mhag?
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
Access through your institution Buy or subscribe Allogeneic hematopoietic cell transplantation (HCT) represents a potentially curative treatment modality for several hematologic
malignancies. Conventional myeloablative conditioning regimens are associated with high treatment-related mortality. To this end, the introduction of nonmyeloablative (NMA) conditioning
implies that older and more frail patients can be offered HCT, and recent data suggest comparable outcome of conventional and NMA–HCT, both with regards to efficacy and side effects, at
least for selected indications.1 The curative principle in allogeneic HCT with NMA conditioning is solely related to the graft-versus-leukemia (GVL) effect, and several lines of evidence
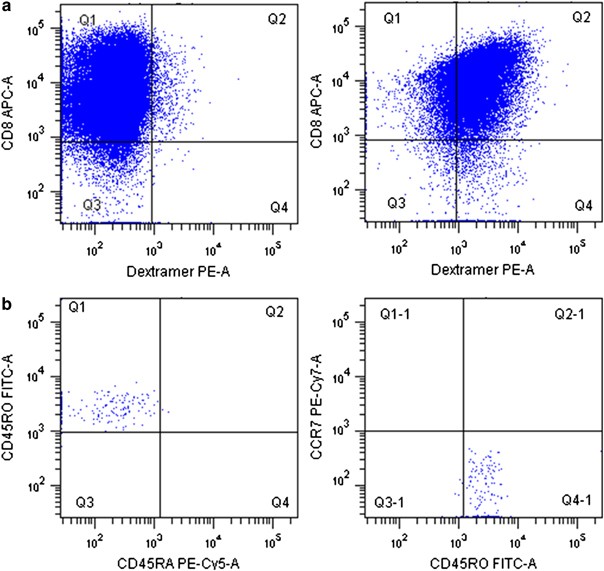
strongly suggest that donor T cells are the main effectors. In human leukocyte antigen (HLA), identical sibling HCT, T-cell responses to minor histocompatibility antigens (mHags) are—at
least in part—responsible for the GVL effect but also cause graft-versus-host disease (GVHD). GVHD represents a major side effect of HCT, and it is well established that there exists
correspondence between the GVL effect and GVHD. As a consequence, increased knowledge concerning mechanisms at play and the targets recognized may set the stage for development of treatment
strategies that focus on induction of GVL in the absence of GVHD.2 Obviously, increased insight into the cells, molecules and antigens involved with GVL and GVHD are important to possibly be
able to control and direct these events more precisely. mHags are known to represent prominent target structures in the HCT setting.3 In general, mHags may derive from antigens expressed on
the male Y chromosome, or from polymorphic proteins encoded on autosomal chromosomes. A limited number of mHags has been characterized, but the HA-1 and HA-2 antigens—derived from
nucleotide polymorphisms in proteins of hematopoietic lineage—have been shown to represent prominent targets at mismatch and therefore represent ideal target structures that could be used in
a therapeutic setting, for example, vaccination in combination with HCT.4 However, the practical applicability of single nucleotide polymorphism derived mHags in cancer therapy obviously
depends on the frequencies of the individual single nucleotide polymorphism in the population, which for several of the characterized mHags are quite low.3, 5 Moreover, the frequencies of
these mHags display significant differences among populations even in Europe.6 Conversely, Histocompatibility Y (HY)-derived mHags are relevant also in practical terms as this group of
antigens are potentially relevant in all female to male HCT, although it should be mentioned that female to male HCT is preferentially avoided due to a higher risk of GVHD. Concerning Y
chromosome encoded mHags, the Y-chromosomal protein SMCY-derived mHag restricted by HLA-A2.01; FIDSYICQV (HY-A2)7 could represent an important target as data from other studies suggested the
dominance of this antigen at parity for HA-1/2 antigens.8, 9, 10 This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through your institution
Subscribe to this journal Receive 12 print issues and online access $259.00 per year only $21.58 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full
article PDF Buy now Prices may be subject to local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs *
Contact customer support REFERENCES * Sorror ML, Storer BE, Maloney DG, Sandmaier BM, Martin PJ, Storb R . Outcomes after allogeneic hematopoietic cell transplantation with nonmyeloablative
or myeloablative conditioning regimens for treatment of lymphoma and chronic lymphocytic leukemia. _Blood_ 2007; 111: 446–452. Article PubMed Google Scholar * Dickinson AM, Wang XN,
Sviland L, Vyth-Dreese FA, Jackson GH, Schumacher TN _et al_. _In situ_ dissection of the graft-versus-host activities of cytotoxic T cells specific for minor histocompatibility antigens.
_Nat Med_ 2002; 8: 410–414. Article CAS PubMed Google Scholar * Spierings E, Wieles B, Goulmy E . Minor histocompatibility antigens—big in tumour therapy. _Trends Immunol_ 2004; 25:
56–60. Article CAS PubMed Google Scholar * Hambach L, Goulmy E . Immunotherapy of cancer through targeting of minor histocompatibility antigens. _Curr Opin Immunol_ 2005; 17: 202–210.
Article CAS PubMed Google Scholar * Minor Histocompatibility Knowledge Database; dbMinor (http://www.lumc.nl/5033/dbminor/), accessed 20 March 2008. * Spierings E, Hendriks M, Absi L,
Canossi A, Chhaya S, Crowley J _et al_. Phenotype frequencies of autosomal minor histocompatibility antigens display significant differences among populations. _PLoS Genet_ 2007; 3: e103.
Article PubMed PubMed Central Google Scholar * Meadows LM, Wang W, den Haan JM, Blokland E, Reinhardus C, Drijfhout JW _et al_. The HLA-A*0201-restricted H-Y antigen contains a
posttranslationally modified cysteine that significantly affects T cell recognition. _Immunity_ 1997; 6: 273–281. Article CAS PubMed Google Scholar * Takami A, Sugimori C, Feng X, Yachie
A, Kondo Y, Nishimura R _et al_. Expansion and activation of minor histocompatibility antigen HY-specific T cells associated with graft-versus-leukemia response. _Bone Marrow Transplant_
2004; 34: 703–709. Article CAS PubMed Google Scholar * Robertson NJ, Chai JG, Millrain M, Scott D, Hashim F, Manktelow E _et al_. Natural regulation of immunity to minor
histocompatibility antigens. _J Immunol_ 2007; 178: 3558–3565. Article CAS PubMed Google Scholar * Rufer N, Wolpert E, Helg C, Tiercy JM, Gratwohl A, Chapuis B _et al_. HA-1 and the
SMCY-derived peptide FIDSYICQV (H-Y) are immunodominant minor histocompatibility antigens after bone marrow transplantation. _Transplantation_ 1998; 66: 910–916. Article CAS PubMed Google
Scholar * Kollgaard T, Petersen SL, Reker S, Masmas TN, Seremet T, Andersen MH _et al_. Evidence for involvement of clonally expanded CD8+ T cells in anti-cancer immune responses in CLL
patients following nonmyeloablative conditioning and hematopoietic cell transplantation (HCT). _Leukemia_ 2005; 19: 2273–2280. Article CAS PubMed Google Scholar * Verdijk RM, Kloosterman
A, Pool J, van de KM, Naipal AM, van Halteren AG _et al_. Pregnancy induces minor histocompatibility antigen-specific cytotoxic T cells: implications for stem cell transplantation and
immunotherapy. _Blood_ 2004; 103: 1961–1964. Article CAS PubMed Google Scholar * Piper KP, McLarnon A, Arrazi J, Horlock C, Ainsworth J, Kilby MD _et al_. Functional HY-specific CD8+ T
cells are found in a high proportion of women following pregnancy with a male fetus. _Biol Reprod_ 2007; 76: 96–101. Article CAS PubMed Google Scholar * James E, Chai JG, Dewchand H,
Macchiarulo E, Dazzi F, Simpson E . Multiparity induces priming to male-specific minor histocompatibility antigen, HY, in mice and humans. _Blood_ 2003; 102: 388–393. Article CAS PubMed
Google Scholar * Mutis T, Gillespie G, Schrama E, Falkenburg JH, Moss P, Goulmy E . Tetrameric HLA class I-minor histocompatibility antigen peptide complexes demonstrate minor
histocompatibility antigen-specific cytotoxic T lymphocytes in patients with graft-versus-host disease. _Nat Med_ 1999; 5: 839–842. Article CAS PubMed Google Scholar * Wang W, Meadows
LR, den Haan JM, Sherman NE, Chen Y, Blokland E _et al_. Human H-Y: a male-specific histocompatibility antigen derived from the SMCY protein. _Science_ 1995; 269: 1588–1590. Article CAS
PubMed Google Scholar * Chen W, McCluskey J . Immunodominance and immunodomination: critical factors in developing effective CD8+ T-cell-based cancer vaccines. _Adv Cancer Res_ 2006; 95:
203–247. Article CAS PubMed Google Scholar * Hambach L, Spierings E, Goulmy E . Risk assessment in haematopoietic stem cell transplantation: Minor histocompatibility antigens. _Best
Pract Res Clin Haematol_ 2007; 20: 171–187. Article CAS PubMed Google Scholar * Cai J, Lee J, Jankowska-Gan E, Derks R, Pool J, Mutis T _et al_. Minor H antigen HA-1-specific regulator
and effector CD8+ T cells, and HA-1 microchimerism, in allograft tolerance. _J Exp Med_ 2004; 199: 1017–1023. Article CAS PubMed PubMed Central Google Scholar * Gratwohl A, Hermans J,
Niederwieser D, van BA, van Houwelingen HC, Apperley J . Female donors influence transplant-related mortality and relapse incidence in male recipients of sibling blood and marrow
transplants. _Hematol J_ 2001; 2: 363–370. Article CAS PubMed Google Scholar * Gale RP, Bortin MM, van Bekkum DW, Biggs JC, Dicke KA, Gluckman E _et al_. Risk factors for acute
graft-versus-host disease. _Br J Haematol_ 1987; 67: 397–406. Article CAS PubMed Google Scholar * Molitor ML, Burlingham WJ . Immunobiology of exposure to non-inherited maternal
antigens. _Front Biosci_ 2007; 12: 3302–3311. Article CAS PubMed Google Scholar Download references ACKNOWLEDGEMENTS We thank Tina Seremet for excellent technical assistance. We also
thank Jørgen Schøller, DAKO for supply of HY/dextramer complexes. The study was supported by the Danish Cancer Society, the Novo Nordisk Foundation, Danish Medical Research Council and the
Danish Foundation for Cancer Research. Eric Spierings was a special fellow of the Leukemia Society of America (3314-05). AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of
Hematology, Center for Cancer Immune Therapy (CCIT), University Hospital Herlev, Herlev Ringvej 75, Herlev, Denmark T Kollgaard, S Reker Hadrup, M H Andersen & P thor Straten *
Department of Hematology, The Allo-HCT Laboratory, Rigshospitalet, Copenhagen, Denmark S L Petersen, T N Masmas & L Vindeløv * Department of Immunohematology and Blood Transfusion,
Leiden University Medical Center, Leiden, The Netherlands E Spierings Authors * T Kollgaard View author publications You can also search for this author inPubMed Google Scholar * S Reker
Hadrup View author publications You can also search for this author inPubMed Google Scholar * S L Petersen View author publications You can also search for this author inPubMed Google
Scholar * T N Masmas View author publications You can also search for this author inPubMed Google Scholar * M H Andersen View author publications You can also search for this author inPubMed
Google Scholar * E Spierings View author publications You can also search for this author inPubMed Google Scholar * L Vindeløv View author publications You can also search for this author
inPubMed Google Scholar * P thor Straten View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to P thor Straten. RIGHTS
AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Kollgaard, T., Hadrup, S., Petersen, S. _et al._ Natural T-cell responses against minor histocompatibility
antigen (mHag) HY following HLA-matched hematopoietic cell transplantation: what are the requirements for a ‘good’ mHag?. _Leukemia_ 22, 1948–1951 (2008). https://doi.org/10.1038/leu.2008.75
Download citation * Published: 10 April 2008 * Issue Date: October 2008 * DOI: https://doi.org/10.1038/leu.2008.75 SHARE THIS ARTICLE Anyone you share the following link with will be able
to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing
initiative