Contralateral lateral rectus muscle recession in patients with duane retraction syndrome type 3
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
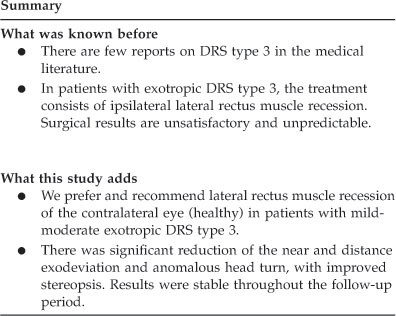
ABSTRACT AIMS The aim of this study was to evaluate the motor, sensory, functional, and head posture results of recession of the lateral rectus muscle contralateral to the involved eye in
patients with exotropic Duane retraction syndrome (DRS) type 3. METHODS This was a retrospective, longitudinal, observational study of a consecutive clinical case series. Of the 11 patients
with DRS type 3 operated on at a tertiary medical center from 1977 to 2012, 8 underwent recession of the lateral rectus muscle contralateral to the involved eye (with combined Y-splitting of
ipsilateral lateral rectus muscle in 3 of them). Full ophthalmic, orthoptic, and neurological examination was performed before and after surgery. Main outcome measures included intragroup
changes in motor misalignment, abnormal head turn, ocular upshoot, and stereopsis. RESULTS Mean patient age was 8.75±3.1 years at surgery. Mean exodeviation for distance was −17.3±3.5 prism
diopters (PD) preoperatively and −4.0±6.1 PD postoperatively; corresponding values for near were −23.1±7.2 PD and −5.9±8.7 PD. Motor deviation improved by 77% for distance (_P_=0.017) and
74.5% for near (_P_=0.01). In 7/8 patients, the postoperative residual exodeviation (distance and near) was <8.0 PD. There was an 80% improvement in head turn, from 15.3±4° before surgery
to 3.1±5.0° after (_P_=0.01). Stereopsis improved significantly in 6/8 patients. Findings remained stable during follow-up (mean duration 35.9±50.8 months, range 5–132 months). CONCLUSIONS
Contralateral lateral rectus muscle recession appears to be a promising technique for the treatment of moderate unilateral DRS type 3, with patients showing significant motor and functional
improvement and a decrease in head turn. SIMILAR CONTENT BEING VIEWED BY OTHERS DUANE—MINUS (DUANE SINE RETRACTION AND DUANE SINE LIMITATION): POSSIBLE INCOMPLETE FORMS OF DUANE RETRACTION
SYNDROME Article 24 August 2020 LONG-TERM SURGICAL OUTCOMES OF ESOTROPIC DUANE RETRACTION SYNDROME TYPE 1 Article Open access 27 January 2025 LONG TERM SURGICAL OUTCOMES OF UNILATERAL
RECESSION-RESECTION VERSUS BILATERAL LATERAL RECTUS RECESSION IN BASIC-TYPE INTERMITTENT EXOTROPIA IN CHILDREN Article Open access 29 September 2021 INTRODUCTION Duane retraction syndrome
(DRS) is a spectrum of congenital ocular motility disorders characterized by limitation of horizontal duction associated with globe retraction1, 2, 3 and consequent narrowing of the
palpebral fissure in adduction.4 DRS is caused by dysinnervation of the extraocular muscles (EOMs) by branches of the oculomotor nerve.5, 6 Huber7 classified DRS into three categories on the
basis of electromyography examinations: type 1, limitation of abduction; type 2, limitation of adduction of the involved eye; and type 3, limitation of abduction and adduction of the
involved eye. Co-contraction of the horizontal and/or vertical rectus muscle is typical to all three types.8 DRS type 3 is the second most common after DRS type 1, usually monocular, and
mostly sporadic. It is characterized by exotropic or esotropic deviation or orthophoria because of the abnormal innervation of the lateral and medial rectus muscle by the ipsilateral
oculomotor nerve.9, 10, 11 Traditionally, surgery for the treatment of exotropic DRS type 3 consists mainly of recession of the ipsilateral lateral rectus muscle to correct the horizontal
misalignment.11, 12, 13, 14 However, the resulting primary position of the eye is unpredictable, with increasing lateral rectus limitation, and the visual field of single binocular vision
may be reduced. An alternative surgical approach is recession of the lateral rectus muscle of the noninvolved (normal) eye in selected patients in order to better estimate the postoperative
horizontal alignment. The aim of the present study was to evaluate the motor and sensory functional results of recession of the lateral rectus muscle contralateral to the affected eye in
patients with exotropic DRS type 3. PATIENTS AND METHODS DESIGN AND PATIENTS A retrospective study design was used. Patients were identified by a search of the electronic database of the
Pediatric Ophthalmology Unit of Schneider Children’s Medical Center of Israel for all children treated for DRS type 3 from 1997 to 2012. Exclusion criteria were previous EOM or retinal
detachment surgery, presence of an ocular malformation or neurological deficit, and <5 months of postoperative follow-up. The study was presented to the Institutional Review Board and was
approved by the Ministry of Health and the hospital director. PATIENT EVALUATION Of the 31 patients with DRS who underwent EOM surgery at our unit during the study period, 11 had DRS type
3. All underwent full ophthalmic, orthoptic, and neurological evaluation before surgery, including cycloplegic refraction with 2 instillations (10 min apart) of cyclopentolate 1%. Distance
(6 m) and near (0.33 m) deviations in the primary position were measured by the alternate prism cover test on an accommodative target in all diagnostic positions of gaze and in down gaze
with normal head posture, and with the best optical correction, if necessary. Additional ocular upshoot and head turn (measured by goniometer) were evaluated as well, and binocular tests for
fusion (Worth 4-dot test) and stereopsis (Titmus fly test) were conducted. The presence of a space-occupying lesion, myasthenia gravis, or intracranial vascular problem was ruled out.
Duction limitation in the involved eye was identified by evaluating ocular motility toward the horizontal side, abduction and adduction, and nasal and temporal up/down positions, with
comparison of the findings with the (normal) contralateral eye. Only patients with ocular abduction and adduction limitation of ≥−2 were classified as DRS type 3. Indications for surgery
were horizontal distance and near vision misalignment of ≥10 prism diopters (PD) in the primary position, significant ocular upshoot, and abnormal head turn of >10°. A forced duction test
in all directions was performed intraoperatively in all cases. SURGICAL TECHNIQUE All operations on the noninvolved eye were performed under general anesthesia by two surgeons (MS and
NG-C). In patients with similar exotropia for distance and near, standard lateral rectus recession was performed in the uninvolved eye, as described by Parks.15 In patients with a
significant difference between distance and near exodeviation, we used the slanted procedure wherein the upper and lower pole of the lateral rectus muscle was recessed nonsymmetrical from
the original insertion, as described in detail by Snir _et al._16 In the presence of moderate–severe upshoot, this procedure was combined with Y-split (bifurcation) of the lateral rectus
muscle in the involved eye,17, 18 according to the guidelines of Rosenbaum and Santiago19 and Jampolsky.20, 21 The split ipsilateral lateral rectus muscle was recessed for 1.0 mm. The upper
half was sutured to the adjacent upper corner of the original insertion and the lower half was sutured adjacent to the lower corner of the original insertion. The distance between the two
halves at the suturing points was equal to the muscle width. OUTCOME MEASURES Surgical and functional results were evaluated by repeating the presurgical examinations (including double
Maddox rod test) on postoperative day 1, at 1, 3, and 6 months postoperatively, and periodically thereafter. Successful outcome was defined as a reduction in ocular horizontal
(distance/near) deviation to ≤8 PD, alleviation of abnormal head tilt to ≤5°, and minimal to no ocular upshoot with regain of binocular functions (stereopsis) at the last ophthalmic
examination. STATISTICAL ANALYSIS The amount of slanted lateral muscle recession was measured by the midpoint distance between the recession points of the upper and lower pole of the muscle.
To evaluate the impact on collapse of the angles of head turn and horizontal distance and near deviations, the mean postoperative measurements were deducted from the preoperative
measurements divided by the lateral rectus muscle recession. The nonparametric Wilcoxon test was used to analyze the change in abnormal head tilt and in distance and near horizontal
exodeviation and stereopsis from before to after surgery. The Mann–Whitney test was used to evaluate age at surgery and postoperative follow-up. A _P_-value of ≤0.05 was considered
significant. All statistical calculations were performed with the SPSS program (Professional statistic release 11.5/2003, Chicago, IL, USA). RESULTS Ages of the 11 patients with DRS type 3
ranged from 4 to 19 years. All were exotropic; none of the patients had orthotropia or esodeviation. Lateral rectus restriction was mild–moderate (+1) in 8 patients and moderate (+2/+3) in
3. Of the 11 patients, 8 (73%) underwent recession of the lateral rectus muscle contralateral to the involved eye, and formed the study group. The other 3 patients were treated by the
standard surgical approach (ipsilateral surgery of the involved eye). The study group consisted of 5 boys (62.5%) and 3 girls of mean age 8.75±3.1 years at surgery (range, 4–14). The left
eye was affected in 6 patients (75%) and the right eye in 2 patients. All patients were followed for ≥5 months postoperatively (mean 31±46.0 months, range 5–114 months). Standard lateral
rectus recession was performed in five patients and slanting recession procedures in three patients. The mean amount of lateral rectus muscle recession in the nondiseased eye was 6.95±1.2 mm
(range, 6–9). Mean exodeviation for distance in primary gaze improved from −17.3±3.5 PD preoperatively (range, −14 to 25) to −4.0±6.1 PD (range, 0–18) postoperatively; corresponding values
for near were −23.1±7.0 PD (range, −12 to 35) and −5.9±8.6 PD (range, 0–25). On statistical analysis, every 1.0 mm of lateral muscle recessed was associated with a 1.9 PD correction in
exodeviation for distance and a 2.5 PD correction for near. Four patients had ocular upshoot on adduction of the involved eye, of whom three underwent combined lateral rectus recession in
the noninvolved eye and Y-split procedure on the lateral rectus muscle in the involved eye. None had ocular upshoot postoperatively. The remaining patient presented with flick ocular upshoot
that resolved after horizontal EOM surgery in the noninvolved eye. Gross stereopsis was present preoperatively in 4 patients (50%), with a range of 80 to 3000 s of arc, and in 7 patients
(87.5%) postoperatively, with a range of 40 to 3000 s of arc (40 to 50 s of arc in 2 patients and 140 to 3000 s of arc in 5). Mean head turn measured 15.63±4.2° preoperatively (range 0–20)
and 3.1±5.3° postoperatively (0–15). According to our calculations, every 1.0 mm recession of the lateral rectus muscle in the noninvolved eye corrected the head turn by a mean of 1.8°. The
patients who underwent ipsilateral lateral rectus surgery were not included in the study because of their small number (_n_=3) and one of them was lost to follow-up. In all three patients,
results for all postoperative motoric and sensory parameters were unsatisfactory. Mean amount of lateral rectus recession in the involved eye measured 4.7±1.6 mm (range 4–9 mm). The
difference in mean exodeviation for distance from before to after surgery did not achieve statistical significance (_P_=0.29); the same was true for the corresponding changes for near
(_P_=0.1). One patient (1/3) had an ocular upshoot before and after surgery. None of the patients had stereopsis. Reoperation was recommended in 1/3 patients. Overall, the postoperative
evaluation of the study group yielded significant motor changes and improvement in alignment, with a 77% reduction in distance deviation (_P_=0.017) and a 74.5% reduction in near deviation
(_P_=0.012) in primary gaze. In some patients, the horizontal deviation in side gaze was measured only preoperatively. However, none of the operated patients complained of diplopia on
abduction of the noninvolved operated eye. In 7 of the 8 patients (87.5%), the postoperative residual exodeviation for distance and near was <8 PD; the remaining patient had hypertropia
with residual exotropia of >8 PD. In addition, there was a significant (80%) improvement in head turn (_P_=0.01). Single binocular visual field examination was not performed because of
technical problems. No torsional effect was found after surgery on double Maddox rod test. Reoperation was recommended in one patient. DISCUSSION The surgical strategy for DRS type 3 poses a
challenge as all three components of the disorder (horizontal deviation, head turn, and upshoot/downshoot) need to be taken into account on a case-by-case basis.22 The present study
evaluated the outcome of patients with exotropic DRS type 3 treated by contralateral lateral rectus recession instead of the traditional ipsilateral lateral rectus muscle recession. Motor
and functional results were good and remained stable throughout a follow-up period of ≥5 months. Specifically, distance/near exodeviation decreased to ≤8 PD in primary position, anomalous
head turn decreased to ≤5°, eliminating the ocular upshoot, and stereopsis was regained. Together, these findings emphasize the advantages of this surgical technique. Several surgical
methods have been proposed in the ophthalmic literature to treat DRS,23, 24, 25, 26, 27 but most apply to types 1 and 2. Published results of DRS type 3 surgery are sparse in the medical
literature, and the approaches used were not uniform. Most are also old. Using a tailored approach, Jampolsky21, 28 and others24, 25, 26 veered from the classification of Huber7 and
considered the coexisting horizontal (either esotropia or exotropia) or vertical deviation; that is, they applied the surgical treatment intended for esotropic or exotropic DRS types 1 and 2
to DRS type 3 patients with esotropia or exotropia. In two case reports, Von Noorden29 and Sprunger30 recessed the ipsilateral medial and lateral rectus muscles simultaneously in a patient
with DRS type 3 (with upshoot and downshoot), and Liu _et al_,31 in a study of 16 patients with DRS, 13 patients with type 3 (esotropic and exotropic), recessed both horizontal rectus
muscles, with good results in primary position in all patients. Spielmann _et al_32 also reported good results with a posterior fixation suture of the horizontal rectus muscles of the sound
eye. These procedures were based on the rationale of transposing the insertion of these muscles posteriorly in relation to the center of rotation of the globe. Owing to the severe
paradoxical EOM innervation in the involved eye in DRS type 3, operating on the ipsilateral lateral rectus muscle poses a risk of increasing the abduction limitation and incomitant
deviation, with unpredictable results. Furthermore, it is difficult to sufficiently weaken the lateral rectus muscle surgically and it increases esotropia in lateral gaze.21, 28 However,
when recession is performed on the lateral rectus muscle in the contralateral eye, with normal EOM innervation, the postoperative alignment is more predictable. This procedure also increases
the tone in the contralateral normally innervated medial rectus muscle. Surgery is planned according to the misalignment of the secondary deviation. Several authors agree with the notion of
operating on the noninvolved eye to improve alignment results.33, 34, 35 Lingua and Walonker35 suggested operating on the noninvolved eye when the weakened EOM retains enough strength to
rotate the eye into its field of action. Recession of either the yoke muscle of the paretic muscle or the yoke’s antagonist exerts the greatest effect in the primary direction of gaze, where
it is needed. Archer33, 34 suggested that recession of the contralateral (noninvolved) eye decreased both the innervation of the normal operated eye and the aberrant innervation to the EOM
in the involved eye. According to Saunders _et al_,36 two conditions are necessary to achieve good results with surgery on the contralateral agonist EOM of the involved DRS muscle. First,
very large recessions or posterior fixation sutures (Faden procedure) are used in the noninvolved eye to cause comparable duction limitations as in the affected eye. By matching the movement
abnormalities of the eye with DRS, alignment can be restored in the primary position, with the creation of a wider diplopia-free field (and improved single binocular vision)
postoperatively. Second, as the normal eye is usually the dominant one, this technique should be done only in patients with moderate-angle deviation. The rationale for contralateral rectus
muscle recession in DRS type 3 may be clarified by the study of Lingua and Walonker35 in patients with DRS type 1. These authors found that by using both recession and posterior fixation of
the normal medial rectus muscle, they eliminated the abnormal head position and corrected moderate-angle esotropia (up to 40 PD). Similarly, in a discussion of the study results of Saunders
_et al_,36 Kraft37 recommended that this technique be applied on the normal EOM only for esotropia of at least 20 PD (in DRS type 1). Upshoot and downshoot are more common in DRS type 3 than
in types 1 and 2.38 In the present study, half the patients had an upshoot of the affected eye on adduction. In three of these patients, we combined a splitting procedure of the lateral
rectus muscle on the involved side in the same session that successfully eliminated the disfiguration in all cases. This approach was based on the rationale, as advocated by Jampolsky,20, 21
that repositioning each half of the ipsilateral lateral rectus muscle could stabilize the globe and prevent its slippage above or below the horizontal plane. It may add a weakening impact
or reduce the residual postoperative exodeviation. Others reported that this combined technique in the involved eye led to dramatic improvement in patients with moderate globe retraction on
adduction.17, 18, 39, 40, 41 It is noteworthy that our cohort was considerably older (8.75±3.13 years) than in most other common strabismus studies. Kubota _et al_23 reported that 92.7% of
their patients with DRS underwent surgery after age 3 years, and Waddell _et al_9 suggested that surgery for DRS should be performed before age 8 years. However, although DRS is diagnosed
early, the indications for surgery may develop only later in life. Sloper and Collins8 and Chua _et al_12 reported the absence of binocular vision in 20% of their patients. Evaluation of the
postoperative functional/sensory results in our study showed that 6 of the 8 patients (75%) had improved binocular function (stereopsis) compared with preoperative ranges. It is noteworthy
that the improved motoric results were combined with better functional outcomes that helped to stabilize the ocular alignment during the follow-up period. Surgical treatment for DRS in the
literature appears to focus more on the motor than the sensory aspect. However, both features are important in visual rehabilitation, especially in patients with complicated DRS type 3. Our
study is limited by the retrospective design and lack of a control group. The small cohort was because of the rarity of DRS type 3: in the past 15 years, we operated on a total of only 11
patients, of whom 8 were treated with the new approach. Furthermore, the changes in horizontal deviation in side gazes from before to after surgery were not calculated and the field of
single binocular vision was not measured. In conclusion, the present study shows that in a selected group of patients with unilateral moderate exotropic DRS type 3, lateral rectus muscle
recession in the noninvolved eye has several important advantages. It reduces the mean distance/near exodeviation (to ≤8 PD in our cohort), minimizes the head turn (to ≤5° in our cohort),
and eliminates the disfiguring upshoot position (when combined with ipsilateral Y-split). In addition, most of the patients regained stereopsis. The motor, functional, and head posture
improvements remain stable during follow-up. At present, this technique is preferred at our center to correct moderate-angle exodeviation in DRS type 3 with anomalous head turn. Further
collaborative multicenter studies in larger cohorts are needed to corroborate these findings. REFERENCES * Duane A . Congenital deficiency of abduction, associated with impairment of
adduction, retraction movements, contraction of the palpebral fissure and oblique movements of the eye. _Arch Ophthalmol_ 1905; 14: 133–159. Google Scholar * Altintas AG, Arifoglu HB,
Arikan M, Simsek S . Clinical findings and surgical results of Duane retraction syndrome. _J Pediatr Ophthalmol Strabismus_ 2010; 47: 220–226. Article PubMed Google Scholar * De Respinis
PA, Caputo AR, Wagner RS, Guo S . Duane’s retraction syndrome. _Surv Ophthalmol_ 1993; 38: 257–288. Article CAS Google Scholar * Freedman HL, Kushner BJ . Congenital ocular aberrant
innervation – new concepts. _J Pediatr Ophthalmol Strabismus_ 1997; 34: 10–16. CAS PubMed Google Scholar * Parsa CF, Grant E, Dillon WP Jr, du Lac S, Hoyt WF . Absence of the abducens
nerve in Duane syndrome verified by magnetic resonance imaging. _Am J Ophthalmol_ 1998; 125: 399–401. Article CAS PubMed Google Scholar * Scott AB, Wong GY . Duane’s syndrome. An
electromyographic study. _Arch Ophthalmol_ 1972; 87: 140–147. Article CAS PubMed Google Scholar * Huber A . Electrophysiology of the retraction syndrome. _Br J Ophthalmol_ 1974; 58:
293–300. Article CAS PubMed PubMed Central Google Scholar * Sloper JS, Collins AD . Effects of Duane’s retraction syndrome on sensory visual development. _Strabismus_ 1999; 7: 25–36.
Article CAS PubMed Google Scholar * Waddell EM . Duane’s retraction syndrome reconsidered. _Br Orthoptic J_ 1980; 37: 56–65. Google Scholar * Isolated Duane retraction syndrome.
Genetics Home Reference. March 2009. At http://ghr.nlm.nih.gov/condition/isolated-duane-retraction-syndrome. Accessed 18 November 2011. * Barbe ME, Scott WE, Kutschke PJ . A simplified
approach to the treatment of Duane’s syndrome. _Br J Ophthalmol_ 2004; 88: 131–138. Article CAS PubMed PubMed Central Google Scholar * Chua B, Johnson K, Donaldson C, Martin F .
Management of Duane retraction syndrome. _J Pediatr Ophthalmol Strabismus_ 2005; 42: 13–17. PubMed Google Scholar * Natan K, Traboulsi EI . Unilateral rectus muscle recession in the
treatment of Duane syndrome. _J AAPOS_ 2012; 16: 145–149. Article PubMed Google Scholar * Pressman SH, Scott WE . Surgical treatment of Duane’s syndrome. _Ophthalmology_ 1986; 93: 29–38.
Article CAS PubMed Google Scholar * Parks MM . _Ocular Motility and Strabismus_. Harper & Row: Hagerstown, MD, 1975. Google Scholar * Snir M, Axer-Siegel R, Shalev B, Sherf I,
Yassur Y . Slanted lateral rectus recession for exotropia with convergence weakness. _Ophthalmology_ 1999; 10: 992–996. Article Google Scholar * Das JC, Chaudhuri Z, Bhomaj S, Sharma P .
Lateral rectus split in the management of Duane’s Retraction Syndrome. _Ophthalmic Surg Lasers_ 2000; 31: 499–501. CAS PubMed Google Scholar * Rao VB, Helveston EM, Sahare P . Treatment
of upshoot and downshoot in Duane syndrome by recession and Y-splitting of the lateral rectus muscle. _J AAPOS_ 2003; 7: 389–395. Article PubMed Google Scholar * Rosenbaum AL, Santiago AP
. _Clinical Strabismus Management. Principles and Surgical Techniques_. WB Saunders, St Louis 1999. Google Scholar * Jampolsky A . Surgical leashes and reverse leashes in strabismus
surgical management. In: Helveston EM (ed) _Symposium on Strabismus: Transactions of the New Orleans Academy of Ophthalmology_. CV Mosby: St Louis, MO, 1978 pp 244–268. Google Scholar *
Jampolsky A . Strategies in strabismus surgery. In: Crawford IC, Flynn IT, Haik BG, Helveston EM, Hayt CS, Jampolsky A _et al_ (eds). _Pediatric Ophthalmology and Strabismus: Transactions of
the New Orleans Academy of Ophthalmology_. Raven Press: New York, 1985 pp 363–368. Google Scholar * Kraft SP . A surgical approach for Duane syndrome. _J Pediatr Ophthalmol Strabismus_
1988; 25: 119–130. CAS PubMed Google Scholar * Kubota N, Takahashi H, Hayashi T, Sakaue T, Maruo T . Outcome of surgery in 124 cases of Duane’s retraction syndrome (DRS) treated by
intraoperatively graduated recession of the medial rectus for esotropic DRS, and of the lateral rectus for exotropic DRS. _Binocul Vis Strabismus Q_ 2001; 16: 15–22. CAS PubMed Google
Scholar * Souza-Dias C . Recession of both horizontal recti muscles in Duane’s retraction syndrome with elevation and depression of the adducted eye. _Am J Ophthalmol_ 1993; 115: 685–686.
Article CAS PubMed Google Scholar * Puerto-Hernández B, López-Caballero C, Rodríguez-Sánchez JM, González-Manrique M, Contreras I . [Surgical treatment of Duane’s syndrome type I by
recession of the medial rectus of the affected eye and faden operation of the contralateral medial rectus]. [Article in Spanish] _Arch Soc Esp Oftalmol_ 2008; 83: 113–116. Article PubMed
Google Scholar * Farvardin M, Rad AH, Ashrafzadeh A . Results of bilateral medial rectus muscle recession in unilateral esotropic Duane syndrome. _J AAPOS_ 2009; 13: 339–342. Article
PubMed Google Scholar * Nelson LB . Severe adduction deficiency following a large medial rectus recession in Duane’s retraction syndrome. _Arch Ophthalmol_ 1986; 104: 859–862. Article CAS
PubMed Google Scholar * Jampolsky A . When is supermaximal surgery safe? _Am Orthopt J_ 1987; 37: 33–44. Article Google Scholar * Von Noorden GK . Recession of both horizontal recti
muscles in Duane’s retraction syndrome with elevation and depression of the adducted eye. _Am J Ophthalmol_ 1992; 114: 311–313. Article CAS PubMed Google Scholar * Sprunger DT .
Recession of both horizontal rectus muscles in Duane syndrome with globe retraction in primary position. _J AAPOS_ 1997; 1: 31–33. Article CAS PubMed Google Scholar * Liu MM, Zhao KX,
Zhang W, Guo X, Zhu LN, Ma HZ _et al_. [Recession of both horizontal rectus muscles in Duane Retraction Syndrome with significant globe retraction]. [Article in Chinese] _Zhonghua Yan Ke Za
Zhi_ 2012; 48: 776–780. PubMed Google Scholar * Spielmann A, Lagrange B, Laurent M . Le syndrome de retraction de Stilling Duane. Etiopathogénie clinique. Regulation motrice par la
Faden-operation de Cüppers sur l’oeil sain, associé ou non a la chirurgie de l’oeil atteint. _J Fr Orthop_ 1976; 8: 105–107. Google Scholar * Archer SM . Contralateral medial rectus muscle
recession in patients with Duane syndrome. _J AAPOS_ 2004; 8: 296 author reply 296. Article PubMed Google Scholar * Archer SM . Results of bilateral medial rectus muscle recession in
unilateral esotropic Duane syndrome. _J AAPOS_ 2010; 14: 103–104 author reply 104-5. Article PubMed Google Scholar * Lingua RW, Walonker F . Use of the posterior fixation suture in type I
Duane’s syndrome. _J Ocul Ther Surg_ 1985; 4: 107–111. Google Scholar * Saunders RA, Wilson ME, Bluestein EC, Sinatra RB . Surgery on the normal eye in Duane retraction syndrome. _J
Pediatr Ophthalmol Strabismus_ 1994; 31: 162–169. CAS PubMed Google Scholar * Kraft SP . Surgery on the normal eye in Duane retraction syndrome: Discussion. _J Pediatr Ophthalmol
Strabismus_ 1994; 31: 170–171. Google Scholar * Mohan K, Saroha V . Vertical rectus recession for the innervational upshoot and downshoot in Duane’s retraction syndrome. _J Pediatr
Ophthalmol Strabismus_ 2002; 39: 94–99. Article PubMed Google Scholar * Britt MT, Velez FG, Thacker N, Alcorn D, Foster RS, Rosenbaum AL . Surgical management of severe cocontraction,
globe retraction, and pseudo-ptosis in Duane syndrome. _J AAPOS_ 2004; 8: 362–367. Article PubMed Google Scholar * Ohtsuki H, Hasebe S, Tadokoro Y, Kishimoto N, Watanabe S, Okano M .
Synoptometer analysis of vertical shoot in Duane’s retraction syndrome. _Ophthalmologica_ 1992; 204: 82–87. Article CAS PubMed Google Scholar * Von Noorden GK, Murray E . Up- and
downshoot in Duane’s retraction syndrome. _J Pediatr Ophthalmol Strabismus_ 1986; 23: 121–123. Google Scholar Download references ACKNOWLEDGEMENTS We thank Dorit Karesh for the statistical
analysis and Gloria Ginzach for her editorial assistance. AUTHOR INFORMATION Author notes * M Snir and A Dotan: These authors contributed equally to this work. AUTHORS AND AFFILIATIONS *
Pediatric Ophthalmology Unit, Schneider Children’s Medical Center of Israel, Petach Tikva, Israel M Snir, R Friling, Y Ron-Kella & N Goldenberg-Cohen * Department of Ophthalmology, Rabin
Medical Center, Petach Tikva, Israel M Snir, A Dotan & H Stiebel-Kalish * Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel M Snir, R Friling, N Goldenberg-Cohen &
H Stiebel-Kalish * Neuro-Ophthalmology Unit, Rabin Medical Center, Petach Tikva, Israel H Stiebel-Kalish Authors * M Snir View author publications You can also search for this author
inPubMed Google Scholar * A Dotan View author publications You can also search for this author inPubMed Google Scholar * R Friling View author publications You can also search for this
author inPubMed Google Scholar * Y Ron-Kella View author publications You can also search for this author inPubMed Google Scholar * N Goldenberg-Cohen View author publications You can also
search for this author inPubMed Google Scholar * H Stiebel-Kalish View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to
M Snir. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no conflict of interest. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Snir, M.,
Dotan, A., Friling, R. _et al._ Contralateral lateral rectus muscle recession in patients with Duane retraction syndrome type 3. _Eye_ 28, 279–284 (2014).
https://doi.org/10.1038/eye.2013.260 Download citation * Received: 07 February 2013 * Accepted: 30 October 2013 * Published: 06 December 2013 * Issue Date: March 2014 * DOI:
https://doi.org/10.1038/eye.2013.260 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * Duane syndrome 3 * contralateral * LR recession *
exotropia