Cord gas analysis, decision-to-delivery interval, and the 30-minute rule for emergency cesareans
- Select a language for the TTS:
- UK English Female
- UK English Male
- US English Female
- US English Male
- Australian Female
- Australian Male
- Language selected: (auto detect) - EN
Play all audios:
ABSTRACT OBJECTIVE: Our primary objective was to examine the relationship between umbilical arterial gas analysis and decision-to-delivery interval for emergency cesareans performed for
nonreassuring fetal status to determine if this would validate the 30-minute rule. STUDY DESIGN: For this retrospective cohort study, all cesarean deliveries performed for nonreassuring
fetal status from September 2001 to January 2003 were reviewed. A synopsis of clinical information that would have been available to the clinician at the time of delivery and the last hour
of the electronic fetal heart rate tracing prior to delivery were reviewed by three different maternal–fetal medicine specialists masked to outcome, who classified each delivery as either
emergent (delivery as soon as possible) or urgent (willing to wait up to 30 minutes for delivery) since immediacy of the fetal condition is the key factor affecting the type of anesthesia
used. RESULTS: Of 145 cesareans performed for nonreassuring fetal status during this period, 117 patients met criteria for entry, of which 34 were classified as emergent and 83 as urgent.
Kappa correlation was 0.35, showing only fair/moderate agreement between reviewers. In the emergent group, general anesthesia was more common (35.3%, 10.8%, _p_=0.003), and the
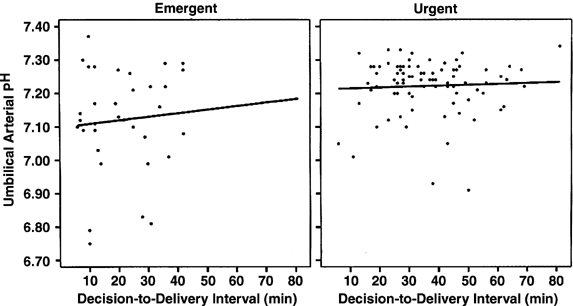
decision-to-delivery interval was 14 minutes shorter (23.0±15.3, 36.7±14.9 minutes, _p_<0.001). Linear regression showed a statistically significant relationship between increasing
decision-to-delivery interval and umbilical arterial pH (_r_=0.22, _p_=0.02) and base excess (_r_=0.33, _p_<0.001) showing that delivery proceeded sooner for most of those with the worst
cord gases, with a gradual improvement over time. For the 13 (11%) neonates with cord gases placing them at increased risk for long-term neurologic sequelae, the decision-to-delivery
interval was 24.7±14.6 minutes (range 6 to 50 minutes), and 3/13 (23%) were classified as urgent rather than emergent. CONCLUSION: Electronic fetal monitoring shows considerable variation in
interpretation among maternal–fetal medicine specialists and is not a sensitive predictor of the fetus developing metabolic acidosis. There is no deterioration in cord gas results after 30
minutes, and most neonates delivered emergently or urgently for nonreassuring fetal status even when born after 30 minutes have normal cord gases. The 30-minute rule is a compromise that
reflects the time it takes the fetus to develop severe metabolic acidosis, our imprecision in its identification, and its rarity in the presence of nonreassuring fetal monitoring. Access
through your institution Buy or subscribe This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through your institution Subscribe to this journal
Receive 12 print issues and online access $259.00 per year only $21.58 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now Prices
may be subject to local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer support
SIMILAR CONTENT BEING VIEWED BY OTHERS OPTIMAL DURATION OF CARDIOTOCOGRAPHY ASSESSMENT USING THE IPREFACE SCORE TO PREDICT FETAL ACIDEMIA Article Open access 29 July 2022 FETAL MONITORING
FROM 39 WEEKS’ GESTATION TO IDENTIFY SOUTH ASIAN-BORN WOMEN AT RISK OF PERINATAL COMPROMISE: A RETROSPECTIVE COHORT STUDY Article Open access 02 December 2021 BLOOD GAS MEASURES AS
PREDICTORS FOR NEONATAL ENCEPHALOPATHY SEVERITY Article 24 June 2021 REFERENCES * American Academy of Pediatrics, American College of Obstetricians and Gynecologists. _Intrapartum and
Postpartum care of Women. Guidelines for Perinatal Care_. Elk Grove Village, IL: AAP; Washington, DC: ACOG; 2002. p. 125–161. * Halsey H, Douglas R . Fetal distress and fetal death in labor.
_Surg Clin North Am_ 1957;37:421–434. Article PubMed Google Scholar * Choate J, Lund C . Emergency cesarean section. _Am J Obstet Gynecol_ 1968;100:703–715. Article CAS PubMed Google
Scholar * Shiono PH, Fielden JG, McNellis D, Rhoads GG, Pearse WH . Recent trends in cesarean birth and trial of labor rates in the United States. _JAMA_ 1987;257:494–497. Article CAS
PubMed Google Scholar * Goldaber KG, Gilstrap III LC, Leveno KJ, Dax JS, McIntire DD . Pathologic fetal acidemia. _Obstet Gynecol_ 1991;78:1103–1107. CAS PubMed Google Scholar * Low JA,
Lindsay BG, Derrick EJ . Threshold of metabolic acidosis associated with newborn complications. _Am J Obstet Gynecol_ 1997;177:1391–1394. Article CAS PubMed Google Scholar * Ross MG,
Gala R . Use of umbilical artery base excess: algorithm for the timing of hypoxic injury. _Am J Obstet Gynecol_ 2002;187:1–9. Article PubMed Google Scholar * Riley RJ, Johnson JWC .
Collecting and analyzing cord blood gases. _Clin Obstet Gynecol_ 1993;36:13–23. Article CAS PubMed Google Scholar * Sibanda J, Beard RW . Influence on clinical practice of routine
intra-partum fetal monitoring. _Br Med J_ 1975;3:341–343. Article PubMed PubMed Central Google Scholar * Amato JC . Fetal heart rate monitoring. _Am J Obstet Gynecol_ 1983;147:967–969.
Article CAS PubMed Google Scholar * Thacker SB, Stroup DF, Peterson HB . Efficacy and safety of intrapartum electronic fetal monitoring: an update. _Obstet Gynecol_ 1995;86:613–620. CAS
PubMed Google Scholar * Shy KK, Luthy DA, Bennett FC, et al. Effects of electronic fetal-heart-rate monitoring, as compared with periodic auscultation, on the neurologic development of
premature infants. _N Engl J Med_ 1990;322:588–593. Article CAS PubMed Google Scholar * Nelson KB, Dambrosia JM, Ting TY, Grether JK . Uncertain value of electronic fetal monitoring in
predicting cerebral palsy. _N Engl J Med_ 1996;334:613–618. Article CAS PubMed Google Scholar * American College of Obstetricians and Gynecologists. _Committee Opinion. Inappropriate Use
of the Terms Fetal Distress and Birth Asphyxia_. American College of Obstetricians and Gynecologists: Washington, DC; 1998, p. 122–123. * Chauhan SP, Magann EF, Scott JR, Scardo JA, Hendrix
NW, Martin JN . Emergency cesarean delivery for nonreassuring fetal heart rate tracings. _J Reprod Med_ 2003;48:975–981. PubMed Google Scholar * Roberts SW, Leveno KJ, Sidawi JE, Lucas
MJ, Kelly MA . Fetal acidemia associated with regional anesthesia for elective cesarean delivery. _Obstet Gynecol_ 1995;85:79–83. Article CAS PubMed Google Scholar * Mueller MD,
Bruhwiler H, Schupfer GK, Luscher KP . Higher rate of fetal acidemia after regional anesthesia for elective cesarean delivery. _Obstet Gynecol_ 1997;90:131–134. Article CAS PubMed Google
Scholar * Dyer RA, Els I, Farbas J, Torr GJ, Schoeman LK, James MF . Prospective, randomized trial comparing general with spinal anesthesia for cesarean delivery in preeclamptic patients
with a nonreassuring fetal heart trace. _Anesthesiology_ 2003;99:561–569. Article CAS PubMed Google Scholar * Leung AS, Leung EK, Paul RH . Uterine rupture after previous cesarean
delivery: maternal and fetal consequences. _Am J Obstet Gynecol_ 1993;169:945–950. Article CAS PubMed Google Scholar * Hawkins JL, Koonin LM, Palmer SK, Gibbs CP . Anesthesia-related
deaths during obstetric delivery in the United States, 1979–1990. _Anesthesiology_ 1997;86:277–284. Article CAS PubMed Google Scholar Download references AUTHOR INFORMATION AUTHORS AND
AFFILIATIONS * Department of Gyn-Ob, Division of Maternal–Fetal Medicine, Johns Hopkins University School of Medicine, Baltimore, MD, USA Cynthia J Holcroft MD, Ernest M Graham MD, Abimbola
Aina-Mumuney MD & Janice L Henderson MD * Ross Medical School, Dominica, West Indies Karishma K Rai MD * Department of Anesthesia, Johns Hopkins University School of Medicine, Baltimore,
MD, USA Donald H Penning MD Authors * Cynthia J Holcroft MD View author publications You can also search for this author inPubMed Google Scholar * Ernest M Graham MD View author
publications You can also search for this author inPubMed Google Scholar * Abimbola Aina-Mumuney MD View author publications You can also search for this author inPubMed Google Scholar *
Karishma K Rai MD View author publications You can also search for this author inPubMed Google Scholar * Janice L Henderson MD View author publications You can also search for this author
inPubMed Google Scholar * Donald H Penning MD View author publications You can also search for this author inPubMed Google Scholar ADDITIONAL INFORMATION Statistical Consultant: Elizabeth A.
Johnson, MS, Bloomberg School of Public Health, Biostatistics Department, Johns Hopkins University, USA. Presented at the annual meeting of the Society of Obstetrical Anesthesia and
Perinatology, Phoenix, AZ, USA, May 14–17, 2003. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Holcroft, C., Graham, E., Aina-Mumuney, A. _et al._ Cord
Gas Analysis, Decision-to-Delivery Interval, and the 30-Minute Rule for Emergency Cesareans. _J Perinatol_ 25, 229–235 (2005). https://doi.org/10.1038/sj.jp.7211245 Download citation *
Published: 23 December 2004 * Issue Date: 01 April 2005 * DOI: https://doi.org/10.1038/sj.jp.7211245 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this
content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative